Lower Extremity Orthotics, Shoes, and Gait Aids
Alberto Esquenazi
Lower limb orthoses, with their many variations, are among the most commonly prescribed biomechanical devices intended to assist walking in individuals with gait dysfunction, caused by musculoskeletal or neuromuscular diseases, (1). Walking is one of the most desirable self-reported goals for patients entering a rehabilitation program and the preponderance of lower limb orthotic devices in clinical use reflects this desire and the fact that present orthotic technology often does a reasonable job of restoring gross physical capacity for level walking and standing.
ROLE AND USE OF ORTHOTICS
Orthoses are devices applied to the external surface of the body to achieve one or more of the following; relieve pain, immobilize musculoskeletal segments, prevent or correct deformity, and improve function. Orthoses provide a direct support component to the braced limb segment and limit the range of motion of a joint. This mechanism largely gives rise to reduction of axial loads and thus perhaps aids in joint pain relief. It may also be used to partially or fully immobilize the joint, and in this manner produce deformity prevention or correction and also improve function. In conjunction with the above two mechanisms, a more difficult mechanism to visualize is the fact that orthoses modify the total static and dynamic force/moment distributions in the braced and more distal segments (“in” joints or about a joint center) and provide a substitute power source for weak muscles while maintaining level surface walking safety and efficiency.
Overall, orthotics can be divided into two major categories, namely, corrective and accommodative devices. In the near future, orthotic technology will also provide artificial strength. Corrective devices are meant to improve the position of the limb segment, either by stretching a contracture or correcting the alignment of skeletal structures (1). Accommodative devices are meant to provide additional support to an already deformed tissue, to prevent further deformity, and ultimately to improve function. Orthoses can be further classified as static (resting) or dynamic, the latter permitting movement of the involved joint(s) while controlling the direction or alignment of the movement and, at times, providing a substitute power source for weak muscles. The spectrum of orthotic devices available is quite broad, ranging from a simple plastic device applied across one joint to a much more complex device made of a variety of materials and crossing multiple joints (2), some also include control microprocessors. Knowledge of the disease or disorder being addressed with an orthosis, functional anatomy, biomechanics, orthotic components, materials, and, finally, recognition of the anticipated functional outcome are essential for proper orthotic prescription (3,4).
TERMINOLOGY
In the past, the lexicon of terms used to describe orthoses was very confusing; often, clinicians used different terms to describe even the most basic device. Orthoses or parts of devices were given names that might describe their purpose, the body part to which they were applied, the inventor of the device, or the town or institution where they were developed. To facilitate communication and minimize the use of acronyms, a logical, easy-to-use system of standard universal terminology for orthotic devices was developed in the early 1970s by the International Committee on Prosthetics and Orthotics (3). Orthotic devices are named by the joints they encompass in correct sequence followed by the word orthosis. For example, an orthosis that crosses the ankle and the foot is named an ankle-foot orthosis (AFO). One that crosses the knee, ankle, and foot is called a knee-ankle-foot orthosis (KAFO). The intended biomechanical function or material may complement the terminology (i.e., dorsiflexion assistance plastic AFO). More elaborate names or eponyms are typically given to such devices (3), but such language should be avoided whenever possible.
MATERIALS
The orthotic components chosen depend on the functions they fulfill, but most orthoses consist of three basic elements: interface components, structural components and if intended to be articulated, the type of joints. In orthoses of newer design, it may be impossible to differentiate the joints from the structural and interface components, for example, plastic AFO (2).
The choice of materials in the fabrication of orthotics is expanding rapidly, and a full review of them is beyond the scope of this chapter. The reader is encouraged to expand knowledge on the subject by reading elsewhere about this topic (5). The two primary material categories are plastics and metals. Plastics have the benefits of light weight, total contact, adjustable flexibility, the ability to adjust in shape, and a more cosmetic appearance. Metal orthoses often have the advantage of increased durability and, in the hands of a skilled orthotist, built-in adjustability. With the advent of new products such as carbon graphite and extruded plastic materials, the advantages of maximal tension strength, lightweight design, and ease of adjustability are combined (6). Factors that dictate the type of material used in orthotic fabrication include the length of time the orthosis will be used, the amount of forces applied across the orthosis, and the amount of axial weight loading. A complete orthotic prescription should include the joints it encompasses and suggest the desired biomechanical alignment and materials of fabrication and materials to use for closures (e.g., leather straps, Velcro, etc.), and where they should be attached (Fig. 76-1).
When the orthosis is ready, it should be evaluated off and on the patient to ensure proper construction, fit, and function. When these characteristics are achieved, appropriate training of the patient and family should be organized.
Orthotic management is best accomplished in the majority of patients with the use of plastic molded orthoses. They provide more intimate contact with better distribution of the controlling/corrective forces over a larger surface area. These devices generally fit inside the shoe, tend to be more cosmetic, and hence better accepted. The patient is permitted to exchange shoes as long as constant heel height is maintained to avoid altering the intended dynamic alignment of the device. Plastic materials are lighter in weight and easier to maintain. The recent availability of adjustable ankle joints that can be attached to plastic orthoses has eliminated a major disadvantage of these devices when compared to metal/leather device. Lack of sensation and fluctuating edema are relative contraindications to the prescription of plastic molded devices. If the patient has adequate visual perception, cognition, and good social support, he or she can compensate for these two deficits and receive the added benefits provided by plastic braces. Two major types of plastic materials are used in orthotics: thermosetting and thermoplastic. Thermosetting plastics include formaldehyde, epoxy, and polyester resins that are typically used as laminates in a similar manner than that used for prosthetic socket fabrication. They require heat produced by a chemical reaction to harden a multilayer of weaved fibers of different products but do not soften with subsequent heating.
Thermoplastics soften when they are heated, making the material moldable. Subsequent heating will soften the material for further molding, and lowering the temperature hardens the material once again. High-temperature thermoplastics, such as polyethylene, polypropylene, copolymers, ortholene, thermo plastic elastomers and vinyl polymers, require heating to temperatures greater than 150°F to mold. Fabrication of an orthosis made of any of these materials requires an exact plaster mold of the desired body part. The heated plastic is then applied to the replica for proper molding under vacuum. These materials are durable, and they have a “good elastic memory,” returning to their original position after flexible deformation. Adjustments to the biomechanical alignment and fit of an orthosis require the intervention of an orthotist. Based on the trim lines of the material, orthosis provide support and may also give a springaction force (Fig. 76-2).
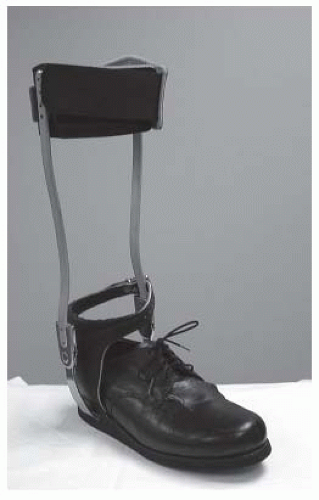
Metal/leather orthoses continue to have a definite place in the treatment of many patients such as those with fluctuating edema, soft tissue wound, hyperhydrosis or intolerance to plastics. Traditional orthotic devices use metals to provide strength and durability. Straps and padding are made of leather. The metals primarily used are steel and aluminum, mostly in alloy forms with various other metals to further increase their strength and to resist corrosion. Although metal orthoses are heavier and are cosmetically less appealing to many patients, their durability and adjustability allows them to accommodate for longitudinal growth and the changing needs of the patient (Fig. 76-3). The choice of orthotic material depends on the clinical purpose and the clinical characteristics of the patient.
Proper biomechanical alignment of any orthosis is critical to maximize the ambulatory capability of a patient. Biomechanical malalignment can and does prevent a borderline patient from becoming a functional ambulator; those patients with better recovery or less deficit may be able to compensate for inadequate orthotic alignment. In those patients for whom orthotic joint motion is required, close correlation between the orthotic and the anatomic joint centers of rotation is mandatory to avoid a discrepancy in the axis of motion which could likely produce pain, joint swelling, skin breakdown, and other preventable problems.
Adjustability of alignment is a significant advantage to current practice patterns where patients are transferred to inpatient rehabilitation programs much earlier than in the past, and the length of stay in the rehabilitation programs has decreased significantly. Predicting the final rehabilitation outcome of these patients so early in their recovery may be very difficult. The ability to adjust the biomechanical alignment of the orthosis with simple tools or to convert a controlling force into an assistive one in order to respond to the patient’s needs
is an important advantage. This is also a potential risk as individuals or patients without the needed knowledge may alter the alignment of the brace or simple use over time may loosen the components (2).
is an important advantage. This is also a potential risk as individuals or patients without the needed knowledge may alter the alignment of the brace or simple use over time may loosen the components (2).
THE SHOE
The shoe is an integral part of any lower limb orthosis that includes the foot, as it serves as the foundation for the device and directly impacts its function (7). The basic function of the shoe is to protect the foot from rough walking surfaces, the weather, and the environment and to provide support for the feet during standing and walking. The use of properly fitting shoes is absolutely essential to the success of any foot orthosis or AFO (8). Factors to consider when selecting a shoe are size, shape, fit, and function. Proper shoe size must take into consideration fit while standing, as the foot configuration changes with weight bearing and pathological phenomenon such as spasticity (9). The foot may swell with prolonged sitting or activity and is often best fitted at the end of the day and after walking around. If a plastic brace is used, then the shoe may need to be slightly longer and or wider to accommodate for this. The parts of a shoe consist of the sole, the heel, the counter (heel and longitudinal arch), the upper, the linings, and reinforcements (10).
Each shoe component can be made of a wide variety of materials and designs, depending on the quality and specific use. It is often best to use flexible, breathable materials such as leather and canvas and not synthetic (plastic) materials for the shoe’s upper components. The construction material of the shoe is very important when considering the function and the modifiability of a shoe. Many off-the shelf shoe styles are available and most can be modified, thereby limiting the need for custom shoes reducing cost and increasing cosmesis resulting in better compliance.
Shoes are built around a positive model or replica of the weight-bearing foot, which is called a last (11). The last, which is made of solid rock maple or plastic materials, determines the fit, walking comfort, appearance, and style of the shoe. Usually the last has a slight fore foot in-flare. Other common lasts include the broad-toe last with a straight medial border that extends from the heel to the toe; the juvenile symmetric straight last, which can be bisected into nearly equal right and left halves; and the orthopedic last with special features designed to accommodate various structural and anatomic problems (e.g., varus, valgus).
During fabrication, the insole is nailed to the last, the lining is tucked to the inner sole rim, and the reinforcements (i.e., counter, toe box) are attached. The upper of the shoe is softened by humidity for easier molding and fitted snugly to the last to conform to its every detail and then nailed or glued to the inner sole. Finally, the outer sole and heel are attached. The Goodyear welt construction of shoes is a method used in production of high-quality shoes in which the upper is sewn to the sole. This method provides a perfectly smooth inner surface, comfort, and a strong shoe that retains its shape and is easy to modify and repair. Unfortunately, these shoes tend to be bulky, heavy, and less flexible.
The upper is that part of the shoe that is above the sole. It is most commonly made of leather, although any soft and durable material may be used. Leather is found to be most comfortable because it allows evaporation and absorption of moisture and molds well to the shape of the foot. Deerskin is significantly softer than leather. It stretches more easily and is generally more accommodative, but is not nearly as durable as leather.
Upper materials are important because they affect the comfort and fit, and performance and durability of the shoe. Shoe uppers are also frequently made of man-made materials such as fabric, nylon, canvas, and plastic but in general they are more difficult to stretch or modify. Recently heat moldable uppers and other elastic plastic materials (e.g., neoprene) have been introduced to the fabrication of shoes. The material is capable of easily stretching around anatomical deformities such as bunions or hammer toes but a problem with this material is its reduced capacity to dissipate heat and moisture. They are an especially useful alternative to custom shoes in patients with severe fore foot deformities who otherwise would need costly custom shoes.
The upper consists of the vamp, quarters, and lace stay. The vamp is the anterior portion of the upper, which covers the toes and the instep. The tongue, a strip of leather lying under the laces, and the throat, the opening at the base of the tongue, are parts of the vamp. Anteriorly, the vamp has a reinforced toe box or toe cap to maintain appearance and to protect the toes against trauma. The lace stay or the portion containing the eyelets for laces is usually part of the vamp, but it may also be part of the quarters. The two quarters make up the posterior part of the shoe. The quarters are usually reinforced by the heel counter, which stabilizes the foot by supporting the calcaneus and giving structural stability to the
shoe. The counter usually extends anteriorly to the heel breast, but it may extend further forward or upward on specially designed shoes. Similar to the toe box, the counter is made of firm leather or synthetic material. Sometimes a band of leather, referred to as a collar, is stitched to the top of the quarters to reduce foot pistoning and to stiffen the shoe. Laterally, the quarter is cut lower to avoid infringing on the malleolus. The linings are made of leather, cotton, or canvas and should be used in all portions of the shoe that are in contact with the foot to absorb perspiration and smoothen the contact area, thus providing added comfort.
shoe. The counter usually extends anteriorly to the heel breast, but it may extend further forward or upward on specially designed shoes. Similar to the toe box, the counter is made of firm leather or synthetic material. Sometimes a band of leather, referred to as a collar, is stitched to the top of the quarters to reduce foot pistoning and to stiffen the shoe. Laterally, the quarter is cut lower to avoid infringing on the malleolus. The linings are made of leather, cotton, or canvas and should be used in all portions of the shoe that are in contact with the foot to absorb perspiration and smoothen the contact area, thus providing added comfort.
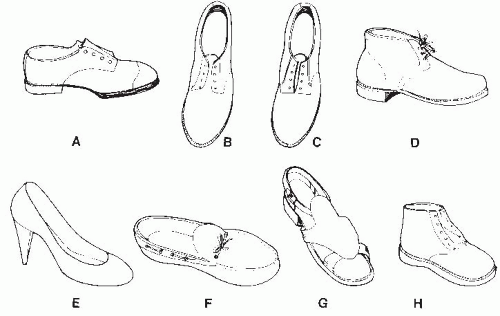 FIGURE 76-4. Shoe types and styles. A: Oxford or low quarter. B: Blucher-type Oxford. C: Bal-type Oxford. D: Chukka or high quarter. E: Pump. F: Moccasin. G: Sandal. H: Child’s shoe. |
The heel of the shoe is attached to the outer sole under the anatomic heel and is made of leather, wood, plastic, rubber, or metal. The heel block, which is fastened to the heel seat, is made of a firm material, but the plantar surface is usually made of hard rubber. The anterior surface of the heel is called the breast. The height and design of the heel vary greatly. Its height is measured at the breast. The flat heel has a broad base and measures 0.75 to 1.25 in. (2 to 4 cm) in height. A Thomas heel is a flat heel that has a medial extension to support a weak longitudinal foot arch. Heels up to 3 in. (7 cm) high are available, but they are mainly used for fashionable appearance rather than for extended walking. Shoes with lower heels, no heels, or negative heels popularized by the earth shoe also exist.
The clinician needs to be aware that the height of the heel has a direct impact on the foot and ankle positions and affects the proximal joints and general posture of the trunk. When a brace is manufactured and aligned, this is done with a particular shoe heel height as part of the design (4). High heels, especially those with a tapered, narrow striking point, make the ankle and foot more unstable and thereby contribute to foot stress, ankle injuries, and falls. Some studies have linked the use of such shoes to abnormal forces in the more proximal joints (12).
Types and Styles
There are innumerable shoe types and styles, although basic designs are relatively few (Fig. 76-4). The basic designs are determined mainly by the shape of the upper, particularly the design of the toe and the height of the quarters. The low-quarter shoe, also known as Oxford shoe, is characterized by the quarters finishing approximately 1 in. below the malleoli with no restriction of ankle or subtalar movement. In high-quarter shoes, the quarters may extend up to barely cover the malleoli, as in the chukka shoe, or extending to the lower third of the tibia or higher, as in boots. This style prevents piston action during walking and back-and-forth sliding of the foot. In addition, it provides some degree of medial-lateral stability at the ankle and subtalar joints, and some restriction of plantar/dorsiflexion ankle motion. The most common opening style is the blucher type, in which the lace stay is not directly fastened to the vamp. This style gives a wide opening for the foot for easy insertion and greater adjustability over the mid foot. For ease of access the surgical opening shoe allows exposure of the entire foot by opening up to the toes. The bal-type (Balmoral) throat, which has the face stay attached directly to the vamp, does not provide such easy foot access. Shoe closure usually is accomplished by cotton laces, which thread through two or more pairs of eyelets, although closure can also be achieved by buckles, zippers, Velcro flaps, or elastics.
Modifications to commercial footwear and in some instances, custom footwear are an important aspect of orthotic practice. Shoe modifications can successfully treat many simple problems that affect walking and is an integral part of any orthotic prescription (11,13).
Dozens of base materials and literally hundreds of variations of those base materials are used in the manufacture of shoes. In this section, discussion is limited to the general categories of materials found in shoes used in conjunction with orthosis and with or as corrective devices. The shoe can be
modified by adding a variety of alterations including changes to the heel, the addition of metatarsal pads, rockers, and other modifications.
modified by adding a variety of alterations including changes to the heel, the addition of metatarsal pads, rockers, and other modifications.
Sole Materials
Materials used in the construction of shoe soles vary greatly and have significantly different properties with regard to weight, durability, shock absorption and attenuation, flexibility, and support.
Leather soles are extremely durable and once it was the choice soling material but now it is reserved primarily for high-end dress shoes. Leather tends to be stiff and heavy, and offers little or no shock absorption when compared to other materials and can be slippery in wet conditions. Leather soles do allow for relatively simple attachment of AFOs.
Hard rubber is a great alternative to leather, especially when used to attach an AFO as it has some degree of impact absorption at heel strike and it is less slippery when used to walk in wet environments. Crepe is a cellular rubber compound that typically offers a great combination of shock absorption and traction. A shoe with a crepe sole can still have an AFO attached to it, although it is not as easy as with a leather or rubber-soled shoe to fabricate. Crepe is the most commonly used material for shoe modifications.
Vibram® is a dense microcellular rubber. It has many qualities of crepe but is more durable and can be more shock absorbing. This material can also be used with a shoe in the construction of an AFO.
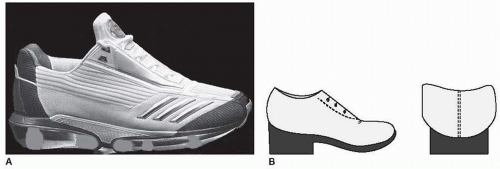
Ethylene vinyl acetate (EVA) is a more recent introduction in the industrial manufacture of most types of shoe. It is shock absorbing, moldable, lightweight, and flexible and can have a multitude of colors. Sometimes this material can be difficult to use in AFO fabrication due to lack of adherence to commonly used cements. In recent years athletic shoes (Fig. 76-5A) have changed dramatically in design and materials used in their fabrication. Different sports may require different design features for optimal performance and comfort. The sole of a good athletic shoe is stiff at the heel and at the shank but very flexible at the fore foot, where it should bend easily at the ball. The outer sole usually is made of highly durable rubber compounds that provide a good grip on the ground, whereas the inner sole is designed to closely fit the contours of the foot. Between the outer and inner soles, fluid, gel or cavitated materials are placed for cushioning and shock dampening. The outer sole is often designed to flare out laterally at the heel and towards the mid foot to improve the mediolateral stability at the ankle and to ensure the foot is flat as it strikes the ground in the normal, slightly supinated position. Rising up from the rear sole to a height of approximately 0.5 in. (1.2 cm) is a heel cup, which further increases mediolateral control and provides hind foot stability. The rigid and non-compressible heel counter provides added ankle and foot stability, but for athletes with a tendency for recurrent ankle sprains, there is the option of using high-top shoes. The upper is reinforced in the mid foot area for maximum stability and to resist excessive side-to-side motion. Such reinforcement is obtained by adding stiffening bands, stabilizing lacing systems, or motion control straps.
Due to their natural increase in coefficient of friction, rubber soles have more traction than leather shoes when walking on carpeted or dry surfaces. Sometimes it is desirable to reduce friction, and application of an external leather toe slider covering the front 1/3 of the sole can be of great benefit to facilitate limb advancement when limb clearance is impaired.
Fitting
The first requirement of a shoe is that it fits and does not cause pain, skin problems, or deformities. Ideally both feet should be measured in length and width, and the shoes tried on both feet in case of size discrepancy, in which case the shoe size should be chosen to comfortably fit the larger foot while some filling material may be used in the smaller one. If more than a one size difference exist, using split size shoes is encouraged (14,15). Footwear preferably should be purchased at the end of the day, when the feet often are slightly swollen. When shoes are fitted, each shoe should be judged individually in a fully weight-bearing position. The shoe should fit snugly enough not to fall off but be loose enough to adapt to the size and shape of the foot,
which changes with climate, ambient temperature, time of day, body position, and standing weight bearing. Because the foot changes shape with weight bearing and some pathological conditions, shoes initially should be carefully tested for fit, both in length and width, not only by standing but by walking for several steps and stopping fast. In length, the shoes should extend at least a half-inch (1.2 cm) beyond the longest toe, usually the hallux or the second toe. The heel-to-ball distance of the foot and the shoe should be equal. Thus, the first metatarsal joint should be located at the inner curve of the shoe, and on toe dorsiflexion, the shoe should bend easily at the toe break that should run directly across the ball of the foot. The widest part of the shoe should coincide with the broadest part of the foot, leaving enough free space medial and lateral to the heads of the first and fifth metatarsal bones, respectively. The shoe widths measured at the ball are available in different sizes, ranging from A (narrow) to E (wide). Each size represents a 0.25-in. (0.6 cm) increase in width.
which changes with climate, ambient temperature, time of day, body position, and standing weight bearing. Because the foot changes shape with weight bearing and some pathological conditions, shoes initially should be carefully tested for fit, both in length and width, not only by standing but by walking for several steps and stopping fast. In length, the shoes should extend at least a half-inch (1.2 cm) beyond the longest toe, usually the hallux or the second toe. The heel-to-ball distance of the foot and the shoe should be equal. Thus, the first metatarsal joint should be located at the inner curve of the shoe, and on toe dorsiflexion, the shoe should bend easily at the toe break that should run directly across the ball of the foot. The widest part of the shoe should coincide with the broadest part of the foot, leaving enough free space medial and lateral to the heads of the first and fifth metatarsal bones, respectively. The shoe widths measured at the ball are available in different sizes, ranging from A (narrow) to E (wide). Each size represents a 0.25-in. (0.6 cm) increase in width.
The transverse arch of the foot should function normally, weight should be evenly distributed, and no sliding of the fore foot within the shoe should occur. There should be no gap between medial and lateral quarters and the heel counter should close around the heel bone without bulges, allowing only a small amount of pistoning. The height of the quarters should be sufficient to hold the shoe securely on the foot. Some pistoning usually is unavoidable in a modified shoe with a rigid sole and heel counter. The height of the vamp should be adequate to prevent pressure or irritation over the toes and the instep. If the material is soft and pliable it should be possible to fold some material from the top of the toe box to confirm appropriate space for the toes. Shoes are not usually fabricated in different depths, although extra-depth shoes and shoes with removable insoles are available to accommodate foot abnormalities and shoe inserts. The real proof of fit, however, is if the shoe is comfortable after hours of continuous wear or walking.
If there is a pathological condition with loss of sensation in the feet, new shoes should be worn using a gradually increasing schedule starting at 2 hours/day only, after which shoes and socks should be removed and the feet carefully inspected. Before donning, each shoe should be carefully inspected visually or with the hand for irregularities or foreign objects on the inside, which could injure the foot.
Shoe Modifications
Stock shoes may require minor or major modifications by various methods to support the abnormal foot during weight bearing, to reduce pressure on painful areas, and to limit motion or accommodate deformed, weak, unstable, or painful joints. For these purposes, the clinician may select a special type of shoe, order certain alterations in the construction of the shoe, or apply corrections directly to the foot. For this approach to be effective, the clinician needs to make an accurate diagnosis of the problem, have a clear understanding of why corrections are needed, and write a specific prescription that is best accompanied by a simple drawing to clarify the request (Fig. 76-5B). Although certain simple external modifications may be applied easily to many types of commercial shoes, welt shoes are more suitable to work with, especially for major internal modifications, because the process of removing and reattaching the sole to the upper does usually not alter the structure of the shoe.