Gail Latlief
Christine Elnitsky
Robert Kent
![]()
10: Lower Extremity Amputation
![]()
PATIENT CARE
GOALS
Provide competent patient care that is compassionate, appropriate, and effective for the evaluation, treatment, education, and advocacy for lower extremity amputee (LEA) patients across the entire spectrum of care, from the acute injury until death, and the promotion of good health.
OBJECTIVES
1. Perform a comprehensive interdisciplinary assessment of the adult with a lower limb amputation.
2. Describe the key components of a rehabilitation program for the lower limb amputee, including long-term follow-up.
3. Identify the main components of an effective patient education strategy for this population to prevent further limb loss as well as potential complications associated with lower limb loss.
Assessment of a person with a new amputation is a vastly important undertaking. This overall assessment will help define the rehabilitation process, identify key areas of possible success or failure, and allow for the highest quality of care for that patient. The first step in the assessment of a person with a lower limb amputation should be developing a clear medical history, including the cause of the amputation and a comprehensive understanding of comorbidities. Description of the amputation surgery, date of surgery, and postoperative complications are all important factors to document.
The past medical history should include direct questioning regarding coronary artery disease, peripheral vascular disease, diabetes mellitus, peripheral neuropathy, stroke, chronic obstructive pulmonary disease, contralateral limb history of ischemia, foot ulcers, trauma, fractures, depression, glaucoma, cataracts, osteoarthritic and rheumatological disorders, end-stage renal disease, and dialysis (including dialysis schedule).
The past surgical history review should include documentation of prior revascularization attempts and their dates, limb salvage surgeries, and prior amputations. Prior amputations should be outlined to demonstrate the progression of the disease. For example, if a person has peripheral vascular disease and has multiple amputations starting with a toe amputation progressing to a transfemoral amputation, the timeline should be identified to help understand the disease process and the patient’s experience. This will aid in further development of a care plan.
Review of systems should include a basic overall review of symptoms with some issues highlighted due to common comorbidities as well as rehabilitation planning. The presence of chest pain, shortness of breath, or other signs of cardiac or respiratory deficiency should be documented. Impaired vision, pain secondary to musculoskeletal conditions (e.g., low back pain) or nerve injury, hand dexterity difficulties, impaired memory and concentration, anxiety, depression, skin issues, and contralateral limb issues should all be documented. Included in the review of systems for specific patient subsets, especially in traumatic amputations, is a clear history of burns or skin grafts. Assessment of burns and skin grafts is necessary for appropriate rehabilitation planning as well as prosthetic design.
Allergies and medications should be reviewed as in any patient. Certain key points in medication review should include pain medications for appropriate pain control and identification of medications that may lead to balance or cognitive deficits.
Social and functional history is an important part of the physiatric assessment and is especially important in amputees. Level of independence with ambulation and activities of daily living prior to and post amputation, employment and hobby history, home environment, presence of stairs and level of support from family, as well as smoking, alcohol, and drug abuse history, should be documented. The physical examination should be thorough and comprehensive (Table 10.1).
Patient and family education is of utmost importance in dealing with amputee patients due to the possibility of negative sequelae that can develop chronically by poor mechanics or skin care, progression of disease and disability, and the need for continued patient-driven rehabilitation. Patients and their families should be educated on proper foot and skin care of the contralateral limb to minimize the risk of limb loss, strategies to minimize the risk of knee and hip flexion contractures, appropriate biomechanics, diabetic education if the patient is diabetic, medication management, pain management techniques including patient-performed physical modalities (e.g., desensitization techniques), fall prevention strategies, safe ambulation and transfers with appropriate assistive devices, and smoking cessation. These educational strategies should take into account the patient’s age, level of education, language preference, preferred method of learning, and ethnicity. Educational content should be presented in multiple formats and repeated to maximize comprehension.
TABLE 10.1 Physical Examination Components
|
|
|
|
|
|
|
|
|
|
|
The assessment of the patient will continue and change as the plan is developed and the patient progresses through the rehabilitation process. There are some key things to identify and discuss concerning each individual at this point. Identifying a K level is important to quickly describe an amputee’s overall functional level. This rating was developed by Medicare (Table 10.2).
TABLE 10.2 K-Level Rating With Brief Description
|
|
|
|
|
MEDICAL KNOWLEDGE
GOALS
Demonstrate knowledge of established evidence based on evolving biomedical, clinical, epidemiological, and sociobehavioral sciences pertaining to LEA, as well as the application of this knowledge to guide holistic patient care.
OBJECTIVES
1. Describe the epidemiology, etiology, anatomy, physiology, and pathophysiology of LEA.
2. Identify the major medical problems faced by amputees and their management.
3. Describe the five phases in the rehabilitation of the LEA.
4. Describe the components of a comprehensive rehabilitation program in the adult with a major limb amputation.
5. Describe the different levels of amputations of the lower limb and the choices of prosthetic limb components in the LEA.
6. Describe postamputation complications in the LEA.
7. Identify causes of gait abnormalities in the LEA ambulating with a prosthesis.
8. Describe management considerations in unique populations with an amputation such as brain injury, spinal cord injury, coronary artery disease, and renal disease.
In the United States, there are approximately 1.6 million people living with limb loss. It has been estimated that 1 of every 200 people in the United States has had an amputation, with dysvascular amputations accounting for 82% of all causes of limb loss. Lower limb amputations are the most common types of amputations. In patients with dysvascular amputations, 15% to 28% will undergo contralateral amputation within the next 3 years after their initial amputation. In elderly patients, only 50% survive longer than 3 years after their initial limb amputation. Greater than half of all diabetic amputees will face a second amputation within 5 years. Traumatic amputations account for 6% to 25% of all amputations. Malignancy-related causes are responsible for roughly 5% of all amputations, most commonly occurring in children and adolescents between 10 and 20 years of age. It is estimated that by 2050 there will be 3.6 million people living with amputations (2). Trauma is seen as a cause of amputation in higher instances in specific populations, including military patient subsets (2–5). Congenital abnormalities are the most common cause for amputation in young pediatric populations. Recent wars have resulted in an increase in traumatic amputations. The Department of Defense–Department of Veterans Affairs Extremity Trauma and Amputation Center of Excellence reports a total of 1,577 Operations Enduring Freedom, Iraqi Freedom, and New Dawn patients with amputations in all military facilities; of these 273 have upper extremity involvement (personal communication, December 20, 2012).
Important elements in the care of the individual with a lower limb amputation include optimizing the management of medical, surgical, and psychiatric comorbidities; optimal treatment of painful conditions; minimizing the risk of future amputations in both the ipsilateral and contralateral limbs; preventing the development of additional impairments; optimal use of a wellfitted prosthesis; and maximizing functionality. These elements of care are important throughout the continuum of care of the amputee, beginning before the amputation surgery and continuing in the preprosthetic and prosthetic phases of rehabilitation and throughout the lifetime of the amputee. The rehabilitation of the lower limb amputee can be divided into five distinct phases: (a) preoperative, (b) acute postoperative, (c) preprosthetic, (d) prosthetic, and (e) long-term follow-up.
In the preoperative phase, the patient is educated on the amputation surgery, the rehabilitative process, basic prosthetic design, and strategies to minimize the risk of contralateral limb loss. Additional education on smoking cessation and nutrition is also important. Rehabilitative efforts during this phase include general strengthening programs for key muscle groups in the upper and lower extremities as well as endurance training to optimize the patient’s physical condition. Psychological counseling and peer counseling can be very helpful in this phase to optimize the patient’s mental state prior to the surgery. In the acute postoperative period, limb shaping should be initiated and strict pain control should be attempted. Prior to transfer to an acute rehabilitation floor or a skilled nursing facility, a person’s medical condition must be optimized so it does not interfere with the rehabilitation process and the person’s safety once transferred.
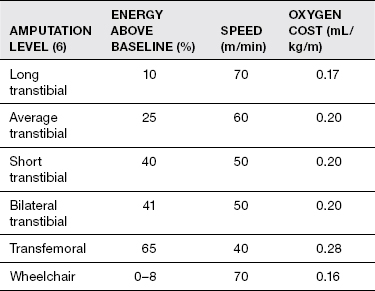
In the preprosthetic phase, the following are important: (a) pain management of residual limb and phantom pain using pharmacological and nonpharmacological interventions; (b) optimization of wound healing of the residual limb; (c) minimization of risk of contractures of the residual limb; (d) management of medical comorbidities such as hypertension, coronary artery disease, diabetes, and chronic obstructive pulmonary disease; (e) optimization of nutrition and hydration; and (f) evaluation and treatment of adjustment disorder, depression, anxiety, and substance abuse as needed. Rehabilitation interventions during this phase include (a) range of motion exercises to the noninvolved extremities and the residual limb; (b) strengthening exercises to key muscle groups in the upper and lower extremities as well as core trunk muscles; (c) bed mobility, transfer training, wheelchair mobility, and gait training with appropriate assistive devices; and (d) training in activities of daily living such as bathing, grooming, dressing, and hygiene. A common question asked by clinical staff and persons with an amputation has to deal with the issue of an appropriate timeline for preprosthetic training during this period. While every patient is different and this should only be seen as a basic reference, the acute postoperative period usually lasts from postoperative day (POD) 1 to day 4; POD 4 to 3 weeks out, continue wound healing with preprosthetic rehabilitation; 3 to 4 weeks after amputation, suture or staple removal and temporary prosthesis fitting and continued physical therapy. Throughout preprosthetic training, crutches are avoided due to possible development of poor gait mechanics with crutch use. Ambulation with a walker is an adequate gauge of the patient’s functionality and relative energy expenditure with the eventual prosthesis (1). During the preprosthetic rehabilitation phase, it is important to identify the patient’s ability and capacity beyond K level and understand the increased energy demands by differing levels. This will allow the clinician to tailor appropriate rehabilitation planning to each individual patient (Table 10.3).
TABLE 10.3 Energy Demands by Level of Limb Amputation
Volume management and protection of the residual limb are an integral part of residual limb management and need to progress during the preprosthetic period. Rigid limb dressings and wrapping of the residual limb are often used to accomplish these goals. Ace wrapping with the figure eight method of wrapping is often the most effective for volume management in the initial postoperative period, but this must be done several times a day and is dependent on proper technique. It is also important to monitor the surgical incision line for evidence of infection and to treat the infection when present. Contractures can occur in the residual limb with the most common sites: (a) knee flexion and (b) hip flexion and hip abduction. Interventions during this phase to minimize the risk of contractures include prone lying and active range of motion. Strategies and techniques for residual limb pain management include desensitization techniques, medications, and strategies for volume control and shaping of the residual limb. The preferred shape for the transfemoral residual limb is conical and for a transtibial residual limb it is cylindrical. Improved outcomes for a shorter transfemoral residual limb are noted with preservation of the greater trochanter and hip adductors attachment. In a transtibial amputation, the tibial tuberosity with patellar attachment is a key structure to save. Other important interventions in this phase include fall prevention strategies and strategies to minimize the risk of additional amputations.
In the prosthetic phase, there is continuation of the interventions started in the earlier phases with the addition of fitting and training in the use of the lower limb prosthesis. Rehabilitation interventions focus on preservation of range of motion in all the limbs with added focus on strategies to reduce and/or treat contractures, strengthening protocols of key muscle groups in the limbs and trunk, balance training—static and dynamic with the prosthesis—as well as gait training. Gait training often begins in the parallel bars and is progressed to other flat surfaces indoors with an appropriate assistive device. As the person becomes more confident, ambulation up and down stairs is added to the training program, as is ambulation on different types of terrain outdoors (i.e., gravel, grass, up/down inclines). Car transfers and driver training are also often offered to amputees as well as opportunities to return to work and sports with modifications. For transtibial amputees, 4 to 6 weeks of physical therapy is usually appropriate, whereas transfemoral amputees often need 6 to 12 weeks. Patient education includes pain control strategies, residual limb care, prosthetic education, care of prosthesis, donning/doffing of the prosthesis, sock management, monitoring of skin for evidence of skin breakdown, coping strategies, patient safety, and weight management.
Long-term follow-up of the patient with a lower limb amputation is recommended for proper fit of the prosthesis, counseling on weight control, smoking cessation, and strategies to preserve the contralateral limb and to ensure appropriate community reintegration. Continued long-term follow-up should be at least annually if not more often, and the condition of components of the prosthesis should continue to be monitored in conjunction with prosthetist in the community or facility.
Prosthetic Fit and Design
Understanding the different types of amputation and the prosthetic options will always help a clinician develop a more effective rehabilitation program with the appropriate prosthetic device. Different levels of amputations of the lower limb will lead to different choices of prosthesic components. While transfemoral and transtibial are the most common lower limb amputations, other amputations, such as knee and hip disarticulations or the Symes procedures, may be seen in the rehabilitation setting as well. A Symes procedure is an ankle disarticulation with the heel pad attached to the distal tibia and accounts for about 3% of lower limb amputations. Transtibial amputations account for 59% of lower limb amputations, transfemoral amputations account for 35% of lower limb amputations, hip disarticulations account for 2% of lower limb amputations, and knee disarticulations account for 1% of lower limb amputations (7). There are also a number of partial foot amputations that should be reviewed by clinicians as well. Another factor to consider in deciding on an appropriate prosthesis is the length of the residual limb length (Tables 10.4 and 10.5).
TABLE 10.4 Transtibial Residual Limb Length
Short: <20% of limb below the knee remains |
Standard: 20%–50% of limb below the knee remains |
Long: 50%–90% of limb below the knee remains |
When choosing a transtibial prosthetic socket design (Table 10.6), the most commonly used is the total contact socket. This type of socket has a medial tibial flare, with relief areas built in for the hamstring tendon and femoral head and a patellar bar for contact at the patellar tendon. Pressure-tolerant areas include the patellar tendon, popliteal fossa and gastroc-soleus complex, pretibial musculature, medial tibial flare, and lateral fibular surface. Pressure-sensitive areas include fibular head, tibial condyles, distal fibula, and hamstring tendons. The development of heterotopic ossification, anatomic variability, and type of surgical amputation performed can all lead to differences in prosthetic fit. A close working relationship with the prosthetic team is integral to rehabilitation success. Transfemoral amputation prosthetic fitting is more complicated for a number of reasons, including use of a prosthetic knee joint, difference in biomechanics, and increased energy expenditure (Table 10.7). Transfemoral amputations are fitted in slight flexion and adduction for improved mechanical advantage to hip extensors and abductors.
The current concepts in amputee care revolve around two major themes: technology and holistic approach to the amputee. In recent years, significant advances have been made in both the fabrication and quality of prosthetic components. Lower limb prostheses are more dynamic and lighter and often incorporate microprocessor technology to improve patient safety, gait, and comfort of use. However, it is important to identify the appropriate candidate for use of this technology since a significant cause of limited use or abandonment of technology is lack of clinician assessment of appropriateness of technology for a patient (1). While patients may wish for the latest technology, it may not always be available to every patient nor indicated, and this should be openly discussed with each individual patient.
Select Postamputation Complications
Phantom pain can start soon after the amputation or years later. It is extremely important to differentiate between phantom sensation and phantom pain. Up to 79% experience phantom sensation and 72% experience phantom pain (8). Physical modalities should be considered prior to initiation of medication, and it is important to remember that use of a prosthesis and weight bearing tends to decrease phantom pain. Physical modalities may include massage and desensitization techniques, ultrasound, wrapping, mirror therapy, short-wave diathermy, and transcutaneous electrical nerve stimulation (TENS). Medications that may have a positive effect on phantom pain include beta-blockers, neuromodulators such as gabapentin, tricyclic antidepressants, calcitonin, and topical analgesics. One topical analgesic that is being used more commonly in peripheral neuropathy is topical ketamine. The mechanism of action is unknown peripherally, as NMDA receptors have only been found centrally; however, research and the efficacy of use have led to the hypothesis that peripheral NMDA receptors are targeted by topical ketamine, thereby providing peripheral pain relief. Gabapentin is often the first-line medication and can be a successful treatment; however, renal function and cognitive impairment need to be identified in this patient group. Increasingly, interventional procedures are being used. Some of the techniques that may be used in refractory cases include trigger point, ultrasound-guided neurolysis, and peripheral nerve stimulation. Narcotics are often used but are not recommended for neuropathic pain.
TABLE 10.5 Transfemoral Residual Limb Length
Short: 0%–35% of the femur remains |
Standard: 35%–60% |
Long: >60% |
TABLE 10.6 Transtibial Prosthetic Sockets and Suspension
Differential pressure |
Silicone suction with shuttle lock
|
Anatomic |
Brim suspension
|
Supracondylar cuff
|
Sleeve
|
COMMON FOOT–ANKLE ASSEMBLIES |
Solid ankle-cushioned heel (SACH foot)—most common one used
|
Single-axis foot
|
Multiaxis foot
|
Dynamic elastic response
|
Microprocessor and power foot/ankles |
TABLE 10.7 Transfemoral Prosthetic Sockets and Suspension*
Quadrilateral design |
|
Ischial containment design
|
SUSPENSION OPTIONS |
Suction
|
Silesian belt |
|
Total elastic suspension belt |
|
Pelvic band and belt suspension |
|
|
|
KNEE COMPONENTS |
Single axis |
|
|
Stance control or safety knee |
|
|
|
|
Polycentric |
|
|
|
Fluid controlled |
|
|
|
|
*Foot components will be the same as listed in Table 10.6.
Other complications and issues to continually monitor in amputee patients include skin care and biomechanics. Skin care of the residual limb and the contralateral limb is important to avoid downtime from prosthetic use, further amputations, and life-threatening infections.
Biomechanics, specifically in gait related to prosthetic use, can be difficult to correct; however, this needs to be addressed as early as possible. Tables 10.8 and 10.9 outline some common stance and swing phase problems.
Special Populations
Multitrauma, Traumatic Brain Injury, and Amputations
The diversity in pathologies that lead to amputations or exist as comorbidities can complicate the rehabilitation process. Multitrauma patients, such as patients who sustain blast injuries, motor vehicle accidents, or gunshot wounds with concomitant traumatic brain injuries, pose particular safety concerns. As for patients who suffer traumatic brain injuries along with amputation of one or multiple limbs, understanding and identifying key safety features in the rehabilitation process are integral to patient safety. These patients are prone to falls for having cognitive impairment that is compounded by an amputation, along with further issues such as spasticity, visual impairment, impulsivity, or vestibulo-cochlear deficits.
TABLE 10.8 Stance Phase Problems
Excessive trunk extension/lumbar lordosis during stance phase |
|
Foot slap |
|
Knee instability |
|
Lateral bending |
|
|
Vaulting |
|
Whip |
|
|
|
TABLE 10.9 Swing Phase Problems
Abducted gait |
|
|
|
Circumducted gait |
|
Foot drag |
|
|
Excessive heel rise |
|
Terminal swing impact
|
Another important consideration is patients who undergo craniectomy after the initial event, which leads to increased possibility of severe injury if a fall were to occur. While wearing a helmet is not usually a consideration for a noncomplicated amputee, in this patient population it is our practice to always have a helmet in place during gait training in any patient with a craniectomy.
Along with fall issues, understanding the etiology and ramifications of the patients’ other injuries is important to map out a safe rehabilitation process. Patients with multiple injuries may have an amputation along with weight-bearing restrictions on other joints that complicate safety issues. When progressing weight bearing, the use of a tilt table or overhead tracts and harness systems allows for offloading weight in order to continue to work on balance, mobility, and upright tolerance.
Polypharmacy is a major concern when it comes to patients with traumatic brain injuries, and this again is compounded when a patient has an amputation. The sedating side effects of pain medications, neuromodulators, and antispasticity medications can impact cognitive therapies and ability to participate as well as decrease safety in cognitively impaired patients.
Heterotopic ossification of joints and soft tissue can cause pain, skin integrity, and mobility issues. The treatment of heterotopic ossification can also be limited by the presence of other healing fractures. This is an extremely important area for prosthetists to work closely with therapists and providers to make socket modifications, such as windows, as well as identify pain with increased weight bearing or any skin breakdown that may be due to the underlying heterotopic ossification. An interdisciplinary team approach to manage these patients is of utmost importance to identify safety concerns as early as possible. Working within these teams, educating family members of patients with amputations with concomitant cognitive deficits needs to be a focus to ensure safety and help prevent complications. Patient families need to be educated on issues such as skin monitoring, stump sock management, donning and doffing prosthesis, residual limb hygiene, componentry inspection, and maintenance.
Spinal Cord Injuries and Amputations
Another complex subset of amputee patients are those with spinal cord injuries. These injuries can be cervical, thoracic or lumbar, complete or incomplete, with varying degrees of ability to tolerate a prosthesis, ambulation, skin complications, and level of independence or expected independence. Working closely with the patient’s primary spinal cord injury team is integral to optimize safety. Identifying team and patient goals—often dictated by their level of injury—is important to be able to choose the most appropriate prosthesis. While some persons may only wish to have a prosthesis for cosmesis, others may be able to progress on to future ambulation, and the most appropriate prosthetic limb for their individual situation will help them safely attain these goals. Working within an interdisciplinary team here again is in the patient’s best interest. Identification of pain issues, early skin issues, progress of limb shaping, or changes in independence will need to be monitored to assure the highest level of safety for these patients while they progress through rehabilitation.
Renal Disease and Amputation
Renal patients are of special concern and offer their own specific complexities. While the list of comorbidities can be extensive, patients with amputations secondary to dysvascular issues are more likely to have renal impairment as well. With changes in limb size due to fluctuating edema, prosthetic fit needs to be monitored closely to identify early skin breakdown or further complications such as pistoning, which could also lead to falls. Dosing of medications that are cleared by the kidneys and creatinine clearance should be monitored, and close co-management with the patient’s nephrologist is recommended. Gabapentin is often used in phantom limb pain and requires especially close monitoring as it can cause further renal damage, and the dosing will change depending on clearance issues. It is also important to keep an updated dialysis schedule if the patient’s renal issues have progressed to that point. Comorbidities such as visual impairment, diabetes mellitus, cardiovascular issues, and increased metabolic demand should all be closely monitored in patients with severe renal disease to optimize safety. Patients with poorly controlled diabetes mellitus should have their blood glucose levels regularly checked to identify and correct for extreme changes in blood sugar that could compromise safety.
Coronary Artery Disease
Coronary artery disease is prevalent in patients with lower extremity peripheral vascular disease, especially among those who go on to amputation. The use of dipyridamole-thallium imaging in these patients may improve the ability to diagnose asymptomatic coronary artery disease before initiating an exercise program, thereby allowing adequate treatment and preventing complications during rehabilitation.
Exercise testing using lower extremity exercise has been the “gold standard” for screening for coronary artery disease, but many patients with peripheral vascular disease and those with amputations have difficulty performing this type of exercise. Arm ergometry is a safe and effective exercise alternative for detecting asymptomatic coronary disease in those unable to exercise their lower extremities and can be used to determine safe upper extremity exercise levels in poorly conditioned patients and those with known coronary disease. Arm ergometry testing is also useful for providing prognostic information concerning functional outcome after a rehabilitation program. Exercise testing is therefore indicated in all vascular amputee patients before beginning an exercise training and prosthetic rehabilitation program. Exercise training can safely and inexpensively enhance the functional capacity of amputee patients with peripheral vascular disease (PVD) (9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


















































































