Organism
Percentage (%)
Staphylococcus aureus
41.7
Staphylococcus epidermidis
16.5
Mixed flora
15.4
Streptococcus sp.
4.7
Enterococcus
2.8
Escherichia coli
1.7
Pseudomonas
1.4
Diphtheroids (Corynebacterium)
1.4
Pneumococcus
1.1
Proteus sp.
1.1
Clostridium sp.
0.8
Bacteroides
0.5
Anaerobic cocci
0.5
Serratia
0.3
Klebsiella
0.3
Acinetobacter
0.3
Enterobacter
0.3
Peptococcus
0.3
Propionibacterium acnes
0.3
Mycobacterium tuberculosis
0.3
Unknown
8.3
Table 59.2
Common aetiology of the different TKR infection types
Acute postoperative (17 %) | Acute haematogenous (13 %) | Chronic (70 %) |
|---|---|---|
Gram-positive organisms (i.e. Staphylococcus aureus) | Gram-positive cocci (i.e. Staphylococcus aureus) | Coagulase-negative staphylococci |
Coagulase-negative staphylococci | Beta-haemolytic streptococci | Staphylococcus aureus |
Gram-negative bacilli | Enterococci | Gram-negative bacilli |
Gram-negative bacilli | Streptococci | |
Enterococci | ||
Anaerobic | ||
Polymicrobial |
Methicillin-sensitive staphylococci, streptococci and anaerobic cocci are commonly considered as low-virulence bacteria, while methicillin-resistant staphylococci, enterococci and gram-negative organisms represent bacteria of high virulence. These may be difficult to eradicate because of their intrinsic resistance to antimicrobial agents and antibiotics [35].
Low-virulence bacteria generally cause a late chronic infection, whereas patients claim only moderate knee pain and stiffness without an evident clinical onset. Less frequently, low-virulence bacteria cause an acute postoperative infection characterized by moderate knee stiffness and/or a delayed rehabilitation only. An acute haematogenous infection is characterized by a sudden deterioration in a previously well-functioning total joint [19].
Low-virulence bacteria generally cause late chronic infection, whereas patients claim only moderate knee pain and stiffness without an evident clinical onset.
The treatment of an infected TKR is still controversial, and many surgical options are available, such as:
While each of these methods may be appropriate for a given patient, two-stage revision surgery has been reported to be the most successful procedure with a success rate of more than 90 % [21, 30, 31, 36, 41, 46, 53]. However, these success rates have not been stratified on the basis of type and virulence of infecting organisms. Certainly, treatment of low-grade TKR infections has been reported to be more successful than treatment of infections caused by resistant organisms [12, 36, 42, 52, 54].
Treatment of low-grade TKR infections has been reported to be more successful than treatment of infections caused by resistant organisms.
59.1 Clinical History and Diagnosis
The diagnosis of low-grade infection after TKR is challenging, since clinical symptomatology and diagnostic studies may be highly conflicting. Moreover, patients often present with well-fixed components, above all in acute infections.
Low-virulence bacteria often determine a late chronic infection. Inoculum of organisms originates at the time of surgery, whereas clinical onset is delayed (1–24 months) depending on the virulence and number of infecting bacteria and the immunologic response of the patient. Classic presentation with pain, fever and local signs such as sinus tract, redness and swelling is uncommon. More frequently patients claim only moderate knee pain and stiffness. It is important to elicit the history of the perioperative period at the time of TKR.
Diagnosis of low-grade infection after TKR is challenging, since clinical symptomatology and diagnostic studies may be highly conflicting. Typically patients often present with well-fixed components, above all in acute infections. Classic presentation with pain, fever and local signs such as sinus tract, redness and swelling is uncommon. More frequently patients claim only moderate knee pain and stiffness.
The following information is of great help:
1.
Wound healing problems, prolonged or persistent postoperative drainage
2.
Prolonged antibiotics after surgery
3.
Any kind of early revision surgery with irrigation and debridement
4.
Comorbidities and risk factors of the patient, such as immunodeficiency, immunosuppressive therapy, diabetes mellitus, obesity, compromised nutrition, hypokalaemia and smoking
5.
Genitourinary or gastrointestinal tracts infections or dental extraction before or after initial TKR
Acute infection caused by low-virulence bacteria is rare (early postoperative or haematogenous). Acute postoperative infection is caused by direct or airborne wound colonization during the procedure, infected haematomas or acute superficial wound infections spreading to the periprosthetic space. The presentation is usually during the first postoperative month. Acute postoperative low-grade TKR infection generally presents only with moderate knee pain and stiffness and/or difficult and delayed rehabilitation; persistent fever, systemic toxicity, severe pain, warmth, erythema and swelling are often absent. Haematogenous infection is characterized by a rapid and unexpected loss of function of a well-functioning TKR. A history of an acute illness may be followed by sudden deterioration in knee function, fever and chills.
Standard radiographs are not helpful for diagnosing low-grade infection after TKR. Clinically, the knee very often looks almost normal. This might be different in low-grade chronic infections, when early loosening occurs and rapidly progressive radiolucent lines appear. This is, however, very infrequent and generally caused by high-virulence bacteria. Different degrees of focal osteolysis, periostitis, endosteal scalloping and implant loosening may be found (Fig. 59.1).
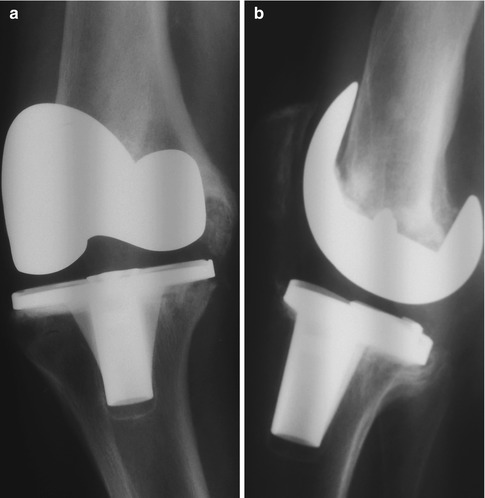
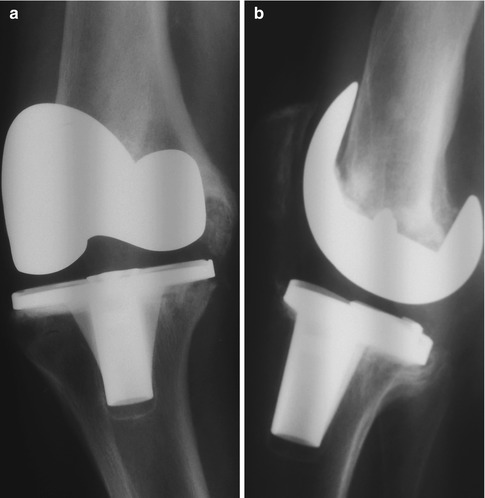
Fig. 59.1
AP (a) and lateral (b) radiographs show femoral component loosening associated with periprosthetic tibial and femoral osteolysis
Standard radiographs are not helpful for diagnosing low-grade infection after TKR. Clinically, the knee very often looks almost normal.
ESR and CRP levels remain the most useful laboratory investigation for the diagnosis of TKR infection, with a sensitivity of about 90 % when used together [1, 16, 37]. However, the sensitivity of the ESR and CRP may be diminished in low-grade TKR infections [58]. WBC count is rarely elevated in chronic infections [16], while in acute infection WBC count results are not very useful as they are strongly influenced by the recent TKR. Patients with chronic infection generally present a raised ESR and/or CRP. ESR may remain elevated for months, but it can also return to normal within 4–8 weeks after surgery [7, 25, 44]. Therefore, CRP results in a more sensitive indicator of infection, especially in early postoperative infections. An ESR of greater than 30 mm/h or a CRP of greater than 10 mg/l should be considered abnormal [8, 16, 17, 37]. Other reasons for elevated serology must be always considered, such as rheumatoid arthritis or other inflammatory diseases. Elevated ESR and CRP levels constitute the basis for obtaining additional diagnostic investigations to document the presence of infection.
ESR and CRP levels remain the most useful laboratory investigation for the diagnosis of TKR infection, with a sensitivity of about 90 % when used together.
Biomarkers such as interleukin-6 (IL-6), procalcitonin and TNF-alpha have become more of a focus when diagnosing infected TKR. It has been shown that procalcitonin and TNF-α have a very high specificity of 0.98 and 0.94, respectively, but a very low sensitivity of 0.33 and 0.45, respectively [9].
In contrast, IL-6 and CRP have the highest sensitivity (0.95) but the IL-6 showed a slightly lower specificity of 0.87 and 0.96, respectively. The combination of CRP and IL-6 is recommended to detect infection in TKR. Similar findings have been reported by others [26].
Nuclear medicine imaging, particularly Tc-99 bisphosphonate scans in conjunction with indium-111 labelled leukocyte scans, can contribute to a proper diagnosis [59]. In particular, if uptake on the leukocyte scan is more intense than uptake on the technetium scan, it is probable that TKR is infected. Normal radionucleotide scans suggest that loosening and infection are not the likely cause of pain. Isotope scanning is certainly sensitive but not specific in diagnosing TKR infection; moreover, sensitivity depends on the infection grade and timing of infection. Within the first postoperative year, an increased scan activity may be present in around 85–90 % of tibial and 60–65 % of femoral components in asymptomatic knees [59].
Microbiologic analysis of the material from the fistula is compulsory. However, a sinus tract is unlikely in low-grade chronic TKR infection due to the low local invasiveness of the organisms.
If most authors favour a selective role for total hip aspiration, routine aspiration for failed TKR with a suspicion of infection is still under debate. If the first aspirate is negative, then at least two additional aspirations should be performed [59]. Specimen obtained from the joint must be separated into two or three samples: if all samples are positive for the same organism, the aspiration is considered positive. If only one sample is positive or presents an unexpected positive result, aspiration must be repeated [48]. Antibiotic therapy must be suspended at least two weeks before the aspiration to avoid false-negative results [17, 30, 37]. The aspirate should be sent for aerobic, anaerobic and fungal cultures.
The most useful laboratory investigation for the diagnosis of TKR infection is ESR and CRP. Joint aspiration and biopsy is recommended. If all samples are positive for the same organism, the aspiration is considered positive. If only one sample is positive or presents an unexpected positive result, aspiration must be repeated. Antibiotic therapy must be suspended at least two weeks before the aspiration to avoid false-negative results.
A WBC count with differential should be per- formed [15, 34]. The detection of bacterial (deoxy)ribonucleic acid in synovial fluid by polymerase chain reaction studies could be helpful. Unfortunately, molecular techniques cannot distinguish between lie and dead organisms, therefore generating false positives (low sensitivity) and resulting in little clinical utility [6].
Biopsies have shown a much higher sensitivity than fluid aspiration and can be easily taken arthroscopically or even in a blind puncture technique. Biopsies should be considered when suspicion of infection remains even after negative aspiration. Fink et al. compared fluid aspiration with arthroscopic biopsies in patients after TKR scheduled for revision surgery because of infection [20]. Fluid aspiration showed a sensitivity of 72.5 % and a specificity of 95.2 %, but arthroscopic biopsies showed superior results with a sensitivity of 100 % and specificity of 98.1 %.
Regarding the intraoperative evaluation, frozen section histologic examination of synovial membrane or prosthetic interface can be helpful in the diagnosis of low-grade infections: 5–10 polymorphonuclear leukocytes per high-power field (×400) (PMNs/HPF) in at least five fields are consistent with infection [8, 30, 34]. This method is highly dependent on the tissue selected and the interpretation of the pathologist. Moreover, the poor sensitivity of this technique in low-grade infection is probably due to the low inflammatory response caused by the coagulase-negative staphylococci, the organisms more commonly infecting TKR [8].
59.2 Treatment Options
The optimal outcome of an infected TKR is represented by eradication of the infection and restoration of a painless and well-functioning joint. The best management is still under debate and many treatment options are available. These include suppressive antibiotics, arthroscopic irrigation and debridement, open debridement with insert exchange, single-stage reimplantation and two-stage reimplantation. The choice of the treatment depends on many variables, including integrity of the implant, timing of the infection, host factors (age, health, immunologic status), virulence of the infecting organism and wishes of the patient. In this context, the validity of each procedure will be evaluated in the treatment of low-grade infection.
Optimal outcome of an infected TKR is represented by eradication of the infection and restoration of a painless and well-functioning joint. Treatment consists of suppressive antibiotics, arthroscopic irrigation and debridement, open debridement with insert exchange, single-stage reimplantation and two-stage reimplantation.
59.2.1 Suppressive Antibiotics
Suppressive antibiotics require a stable implant and a low-virulence organism. The organism must be susceptible to oral antibiotics, and the patient must be tolerant of these antibiotics, perhaps for extended periods of time or even lifelong [10, 22]. Treatment with suppressive antibiotics is reserved for the poorest of the hosts who are medically unable to receive surgery, or when implant removal is not possible [29, 40]. This treatment has had little reported success in eradicating infection, also in low-grade TKR infection [30].
59.2.2 Irrigation and Debridement
In the setting of a low-grade TKR infection, debridement with retention of components could be indicated in healthy patients affected by acute infection with no implant loosening, well-functioning prosthesis and good soft tissue envelope with no fistula [4, 11, 34]. Contraindications are chronic infection, prosthesis loosening, poor soft tissue envelope and patients with other joint replacement or with heart valve replacement [11, 30, 34]. Debridement needs to be performed as early as possible but at least within 4 weeks after surgery or the onset of symptoms. When attempting component retention, thorough debridement and rapid treatment of the infection prior to the accumulation of any biofilm are paramount for a successful outcome [24, 34, 45]. Polyethylene exchange is always necessary because the bacterial glycocalyx that deposits on the polyethylene bearings can cause a recurrence of the infection [8, 24].
One reason for the failure of arthroscopic debridement is likely due to inability to eliminate the biofilm at the polyethylene-prosthesis interface and debride the posterior aspect of the knee [11, 24] (Fig. 59.2). Waldman et al. reported a 62 % failure rate in treating 4 early postoperative and 12 haematogenous TKR infections using arthroscopic irrigation and debridement within 7 days from symptoms [61]. Intraoperative cultures are performed from synovial fluid and membrane, infected tissues and polyethylene-implant interface. The organism-specific intravenous antibiotics are administered for 4–6 weeks, followed by protracted oral antibiotics. Factors associated with failed open debridement include: sinus tract, prolonged postoperative wound drainage, constrained prosthesis, methicillin-resistant staphylococci infections, chronic infections (>4 weeks), immunocompromised patients, rheumatoid arthritis and diabetes mellitus [11, 34].
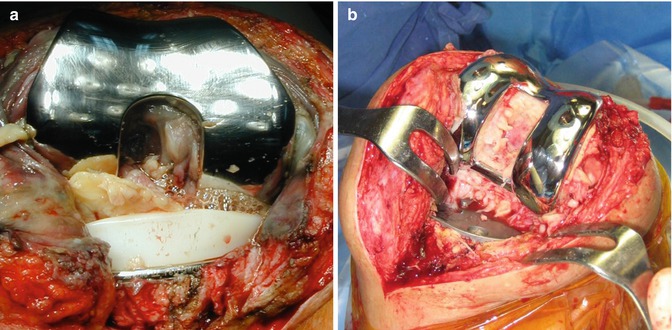
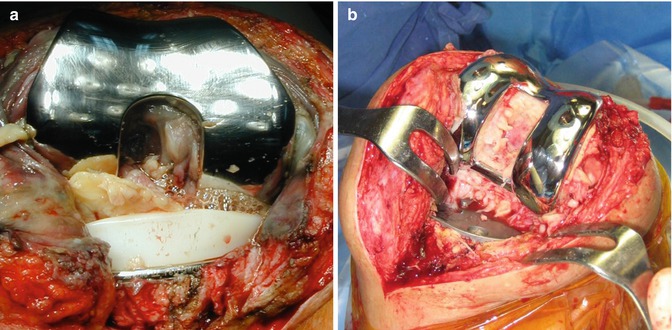
Fig. 59.2
Open debridement with polyethylene removal allows elimination of biofilm on the polyethylene (a) and at the polyethylene-prosthesis interface (b), gaining access to the posterior aspect of the knee and performance of a complete synovectomy (b)
In acute infection, primary open debridement has been reported as successful in 56 % of patients infected by low-grade organisms such as Staphylococcus epidermidis or streptococcal species, but only in 8 % of patients infected by Staphylococcus aureus [14]. Barberan et al. reported higher failure rate in patients with a methicillin-resistant Staphylococcus aureus infection treated with open debridement and irrigation [4]. Azzam et al. recently recommended limiting this procedure to select healthy patients with low-virulence organisms [2]. Mont et al. reported a 100 % success rate in early postoperative infections and a 71 % success rate in haematogenous infections [43]. Silva et al. reported a 32 % success rate when open debridement was used within 4 months after index TKR or 4 weeks after onset of symptoms [55]. Certainly, debridement has been shown to be unsuccessful in treating chronic infections in several series [2, 21, 24]. In particular, Barberan et al. reported an overall failure rate of 35 % of debridement, but it ranged from 17 % in patients with symptom duration less than 1 month to 69 % in patients with symptom duration more than 6 months [4]. However, these data show the correlation between failure rate and time from index surgery.
59.2.3 Single-Stage Reimplantation
Reimplantation after a TKR infection requires specifically an immunocompetent patient and organisms sensitive to antibiotic therapy without any risk of drug toxicity. Adequate bone stock and soft tissue coverage are necessary, and the patient must be fit enough to undergo multiple procedures if needed. Aggressive debridement is an important step in reimplantation after septic loosening. Infected soft tissue and bone removal is essential to eradicate a wide amount of bacteria [34, 62]. At the time of prosthesis removal, sonication could improve sensitivity of microbiologic investigations [1, 51].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








