Chapter 40 Low Back Pain
Epidemiology
Low back pain is a symptom, not a disease, and has many causes. It is generally described as pain between the costal margin and the gluteal folds. It is extremely common. About 40% of people say that they have had low back pain within the past 6 months.233 Studies have shown a lifetime prevalence as high as 84%.240 Onset usually begins in the teens to early 40s. Most patients have short attacks of pain that are mild or moderate and do not limit activities, but these tend to recur over many years. Most episodes resolve with or without treatment. The median time off work for a back injury is 7 days, and many people with low back pain never alter their activity. A small percentage of low back pain becomes chronic, however, and causes significant disability. In most studies about half of the sick days used for back pain are accounted for by the 15% of people who are home from work for more than 1 month. Between 80% and 90% of the health care and social costs of back pain are for the 10% who develop chronic low back pain and disability. Just over 1% of adults in the United States are permanently disabled by back pain, and another 1% are temporarily disabled.151
Anatomy and Biomechanics of the Lumbar Spine
The Vertebrae
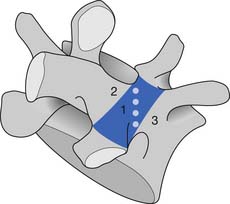
The bony anatomy of the lumbar spine consists of five lumbar vertebrae. A smaller percentage of the population has four (the fifth vertebrae is sacralized) or six (the first sacral segment is lumbarized). Anatomic variants also exist consisting of a partially lumbarized S1. The lumbar vertebrae have distinct components, which include the vertebral body, the neural arch, and the posterior elements (Figure 40-1). The vertebral bodies increase in size as you travel caudally in the spine. The lower three are typically more wedge-shaped (taller anteriorly), which helps create the normal lumbar lordosis. The structure of these large vertebral bodies serves its weight-bearing function well to support axially directed loads; however, they would fracture more routinely were it not for the shock-absorbing intervertebral disks placed strategically between the vertebral bodies.
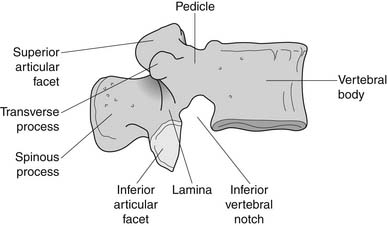
FIGURE 40-1 Lateral view of the lumbar vertebrae.
(Modified from Parke WW: Applied anatomy of the spine. In Rothman RH, Simeone FA, editors: The spine, ed 4, Philadelphia, 1999, Saunders.)
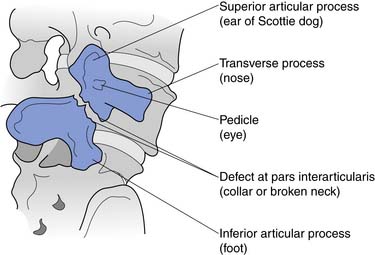
The sides of the bony neural arch are the pedicles, which are thick pillars that connect the posterior elements to the vertebral bodies. They are designed to resist bending and to transmit forces back and forth from the vertebral bodies to the posterior elements. The posterior elements consist of the laminae, the articular processes, and the spinous processes. The superior and inferior articular processes of adjacent vertebrae create the zygapophyseal joints. The pars interarticularis is a part of the lamina between the superior and inferior articular processes (Figure 40-2). The pars is the site of stress fractures (spondylolysis) because it is subjected to large bending forces. This occurs as the forces transmitted by the vertically oriented lamina undergo a change in direction into the horizontally oriented pedicle.23
The Joints
The Intervertebral Disk
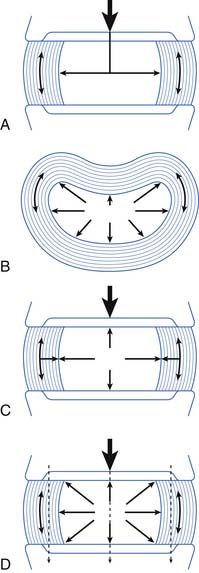
The intervertebral disk and its attachment to the vertebral end plate are considered a secondary cartilaginous joint, or symphysis. The disk consists of the internal nucleus pulposus and the outer annulus fibrosus. The nucleus pulposus is the gelatinous inner section of the disk. It consists of water, proteoglycans, and collagen. The nucleus pulposus is 90% water at birth. Disks desiccate and degenerate as we age and lose some of their height, which is one reason we are slightly shorter in our geriatric years.
The annulus fibrosus consists of concentric layers of fibers at oblique angles to each other, which help to withstand strains in any direction. The outer fibers of the annulus have more collagen and less proteoglycans and water than the inner fibers.19 The varying composition supports the functional role of the outer fibers in acting like a ligament to resist flexion, extension, rotation, and distraction forces.
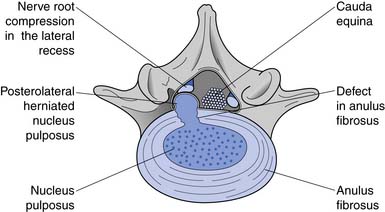
The main function of the intervertebral disk is shock absorption (Figure 40-3). It is primarily the annulus, not the nucleus, that acts as the shock absorber. (The nucleus is primarily a liquid and is incompressible.) When an axial load occurs, the increase in force in the incompressible nucleus pushes on the annulus and stretches its fibers. If the fibers break, then a herniated nucleus pulposus results.
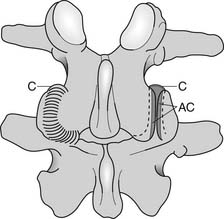
The Zygapophyseal Joints
The zygapophyseal joints (also known as Z joints and facet joints) are paired synovial joints, that is, they have a synovium and a capsule (Figure 40-4). Their alignment or direction of joint articulation determines the direction of motion of the adjacent vertebrae. The lumbar zygapophyseal joints lie in the sagittal plane and thus primarily allow flexion and extension. Some lateral bending and very little rotation are allowed, which limits torsional stress on the lumbar disks. Rotation is more a component of thoracic spine motion. The majority of spinal flexion and extension (90%) occurs at the L4–L5 and L5–S1 levels, which contributes to the high incidence of disk problems at these levels.
Biomechanics
Because flexion loads the anterior disk, the nucleus is displaced posteriorly.111 If the forces are great enough, the nucleus can herniate through the posterior annular fibers. The lateral fibers of the posterior longitudinal ligaments are thinnest, however, making posterolateral disk herniations the most common (Figure 40-5). The posterolateral portion of the disk is most at risk when there is forward flexion accompanied by lateral bending (i.e., bending and twisting). The zygapophyseal joints cannot resist rotation when the spine is in flexion. This increases torsional shear forces in the lumbar spine, making rotary movements in a forward-flexed posture probably the most risky for lumbar disks.
The Muscles
Muscles With Origins on the Lumbar Spine
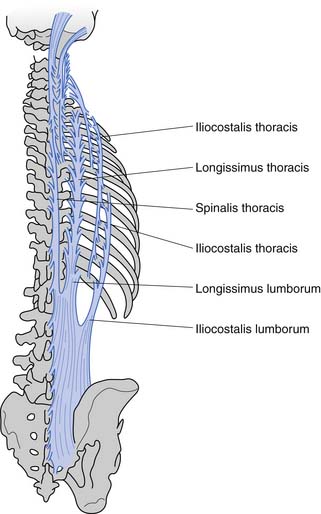
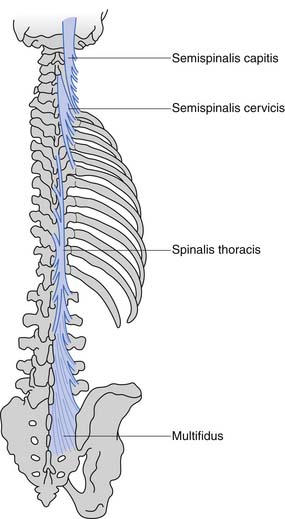
These muscles can be divided anatomically into posterior and anterior muscles. The posterior muscles include the latissimus dorsi and the paraspinals. The lumbar paraspinals consist of the erector spinae (iliocostalis, longissimus, and spinalis), which act as the chief extensors of the spine, and the deep layer (rotators and multifidi) (Figures 40-6 and 40-7). The multifidi are tiny segmental stabilizers that act to control lumbar flexion because they cannot produce enough force to truly extend the spine. Their most important function has been hypothesized to be that of a sensory organ to provide proprioception for the spine, given the predominance of muscle spindles seen histologically in these muscles.
Abdominal Musculature
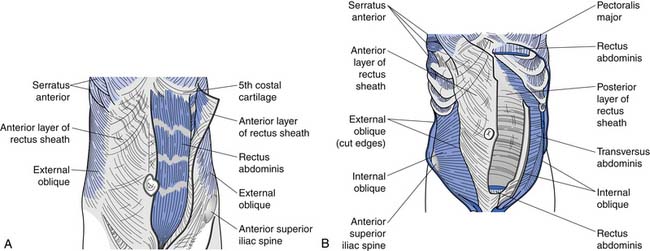
The superficial abdominals include the rectus abdominis and external obliques (Figure 40-8, A). The deep layer consists of internal obliques and the transversus abdominis (Figure 40-8, B). The transversus abdominis has received significant attention recently as an important muscle to train in treating low back pain. Its connection to the thoracolumbar fascia (and consequently its ability to act on the lumbar spine) has probably been the major reason it has received such attention of late.
Thoracolumbar Fascia
The thoracolumbar fascia, with its attachments to the transversus abdominis and internal obliques, acts as an abdominal and lumbar “brace.” It decreases some of the shear forces that other muscles and lumbar motions create. This abdominal bracing mechanism results from contraction of these deep abdominal muscles, which creates tension in the thoracolumbar fascia, which then creates an extension force on the lumbar spine without increasing shear forces.75
Pelvic Stabilizers
The piriformis is a hip and sacral rotator and can cause excessive external rotation of the hip and sacrum when it is tight. This can result in increased shear forces at the lumbosacral junction (i.e., the L5–S1 disk or Z joints). Some practitioners also believe that other pelvic floor muscles act to maintain proper positioning of the spine and are an important focus of some spine rehabilitation programs.
Biomechanical Lifting in Relation to Muscular Activity and Disk Loads
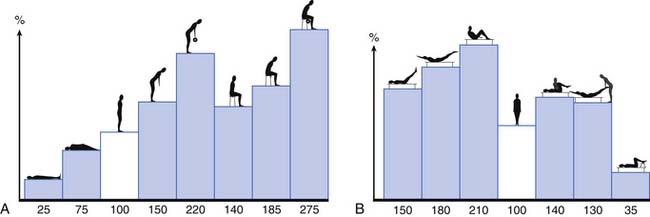
The activity of the lumbar muscles correlates well with intradiskal pressures (i.e., when back muscles contract, there is an associated increase in disk pressure). These pressures change depending on spine posture and the activity undertaken. Figure 40-9 demonstrates the changes in L3 disk pressure under various positions and exercises.149,150 Adding rotation to the already flexed posture increases the disk pressure substantially. Comparing lifting maneuvers, it has been shown that there is not a significant difference in disk pressure when lifting with the legs (i.e., with the back straight and knees bent) versus lifting with the back (i.e., with a forward-flexed back and straight legs).6,7 What decreases the forces on the lumbar spine is lifting the load close to your body because the farther the load is from the chest, the greater the stress on the lumbar spine.7
The Nerves
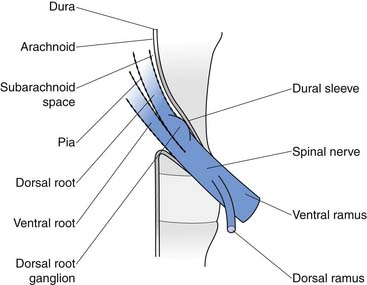
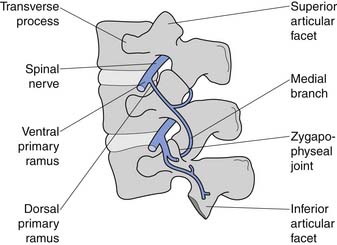
The conus medullaris ends at about bony level L2, and below this level is the cauda equina. The cauda equina consists of the dorsal and ventral rootlets, which join together in the intervertebral neuroforamen to become the spinal nerves (Figure 40-10). The spinal nerve gives off the ventral primary ramus. The ventral primary rami from multiple levels form the lumbar and lumbosacral plexus to innervate the limbs. The dorsal primary ramus, with its three branches (medial, intermediate, and lateral), innervates the posterior half of the vertebral body, the paraspinal muscles, and the zygapophyseal joints, and provides sensation to the back. The medial branch is the most important to remember because it innervates the zygapophyseal joints and lumbar multifidi and is the target during radiofrequency neurotomy for presumed zygapophyseal joint pain (Figure 40-11).24
Pathophysiology and Pain Generation
The Degenerative Spine Cascade
Kirkaldy-Willis et al.108 have supplied us with the most accepted theory describing the cascade of events in degenerative lumbar spine disease that results in spondylotic changes, disk herniations, and eventually multilevel spinal stenosis (Figure 40-12). At the heart of this theory is the fact that, although the posterior zygapophyseal joints and the anterior intervertebral disks are separated anatomically, forces and lesions affecting one certainly alter and affect the other. For example, axial compressing injuries can damage the vertebral end plates, which can lead to degenerative disk disease, which eventually stresses the posterior joints, leading to the common degenerative changes seen in them over time. Torsional stress can injure the posterior joints and the disks, which in turn leads to increased stress on both these elements, resulting in further degenerative changes over time. When these degenerative changes affect one level, such as L4–L5, a chain reaction occurs, placing stress on the levels above and below the currently affected level, and eventually resulting in more generalized multilevel spondylotic changes.
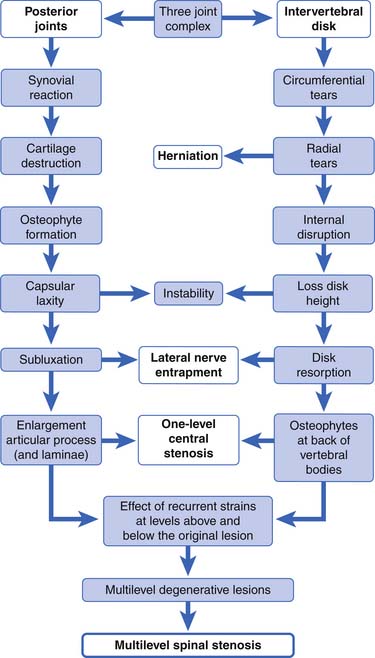
FIGURE 40-12 The spectrum of degenerative change that leads from minor strains to marked spondylosis and stenosis.
(Modified from Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, et al: Pathology and pathogenesis of lumbar spondylosis and stenosis, Spine 3:319-328, 1998, with permission of Lippincott Williams & Wilkins.)
In studying lumbar degenerative disease, the question of which came first (disk degeneration or zygapophyseal joint degeneration) always arises. Fujiwara67 has answered this by studying multiple magnetic resonance images (MRIs) of aging spines. He hypothesizes that disk degeneration precedes zygapophyseal joint osteoarthritis, and that it might take 20 years for zygapophyseal joint disease to occur after the onset of disk degeneration.
To describe the degenerative cascade in more detail, we will separate our discussion of the changes that occur in the posterior joints from those in the disk, but fully realizing that they both can occur simultaneously and affect each other (see Figure 40-12). The degenerative changes that occur in the zygapophyseal joints from aging and repetitive microtrauma are similar to those that occur in the appendicular skeletal joints. The process begins with synovial hypertrophy, which eventually results in cartilage degeneration and destruction. With lessened and weakened cartilage and capsular laxity, the joint can become unstable. With the repetitive abnormal joint motion that results from this instability, the bony joint hypertrophies. This narrows the central canal and lateral recesses, potentially impinging nerve roots.
Although this theory offers an explanation as to how the spine ages, it is still unclear why there is such a marked disconnect between the anatomic changes in the spine associated with aging, and back pain. Many patients with normal spine anatomy suffer from back pain, occasionally disabling pain, and many patients with marked degenerative changes on imaging are nearly or fully pain free. As a result, several theories have been developed to explain the occurrence of back pain.
Radiculitis and Radiculopathy
Many patients with radicular pain have no neural impingement noted on MRI. Studies have shown that disk herniations can cause an inflammatory response.131,136,187 The mechanism stems from the fact that the nucleus pulposus is highly antigenic as a result of being in an immunoprotected setting in nonpathologic states. When the fluid of the nucleus pulposus is exposed to neural tissue of the spinal canal and neuroforamen through a defect in the annular fibers, an autoimmune-mediated inflammatory cascade begins. The inflammatory mediators generated can cause swelling of the nerves. This can alter their electrophysiologic function, sensitizing these neurons and enhancing pain generation without specific mechanical compression.
The mechanism of mechanical compression of the nerve roots has been studied as well.13,184,185 Compression of nerve roots can induce structural and vascular changes as well as inflammation.150 Neural compression can result in impairment of intraneural blood flow, subsequently decreased nutrient supply to the neural tissue, local ischemia, and formation of intraneural edema. This can set off an inflammatory cascade similar to that described above. Mechanical stimulation of lumbar nerve roots has also been shown to stimulate production of substance P, the neuropeptide known to modulate sensory nociceptive feedback.13 With these biochemical reactions, the local structural effects of mechanical compression (demyelination and axonal transport block) just compound the symptomatic response.
Pain of Spinal Stenosis
If mechanical compression were the sole problem in spinal stenosis, decompressive surgeries would be the only needed cure. We know that this is untrue, and consequently alternative theories on the pathogenesis of symptomatic spinal stenosis have been studied. Two theories supporting a vascular component to symptoms of spinal stenosis are the venous engorgement and arterial insufficiency theories.1
In the venous engorgement theory, the spinal veins of patients with stenosis dilate, causing venous congestion and stagnating blood flow.45 This pooling of blood in the spinal veins increases epidural and intrathecal pressures, leading to a microcirculatory, neuroischemic insult (i.e., an ischemic neuritis), which in turn leads to the typical neurogenic claudication symptoms of stenosis.
The arterial insufficiency theory of spinal stenosis is based on the arterial dilatation of the lumbar radicular vessels during lower limb exercise to provide increased blood flow and nourishment to the nerve roots. In patients with spinal stenosis, this reflex dilatation might be defective.14Because patients with spinal stenosis are typically elderly, they are also at higher risk for atherosclerosis, which in turn just amplifies the arterial insufficiency.
Pain Generators of the Lumbar Spine
The low back is an anatomically diverse set of structures, and there are many potential sources of pain. One useful strategy to clarify these potential sources of pain is learning what low back structures are innervated (and can transmit pain through neural pain fibers) and what structures have no innervation (Box 40-1).
Segmental Dysfunction
Segmental dysfunction can occur when either a segment is too stiff or too mobile. A segment encompasses the disk, the vertebrae on each side of the disk, and the muscles and ligaments that act across this area. Excessive stiffness is thought to be caused by arthritic and ligamentous changes. Excessive mobility, also called instability, or potentially better termed “functional instability,” can be the result of tissue damage, poor muscular endurance, or poor muscular control, and is usually a combination of all three factors. Structural changes from tissue damage, such as strained or failed ligaments that cause joint laxity, vertebral end-plate fractures, and loss of disk height, can lead to segmental dysfunction because of the altered anatomy. Muscles also provide a critical component of spinal stability. This is of particular interest to the physiatrist because it can be affected by exercise. In normal situations, only a small amount of muscular coactivation (about 10% of maximal contraction) is needed to provide segmental stability. In a segment damaged by ligamentous laxity or disk disease, slightly more muscle coactivation might be needed. Because of the relatively gentle forces required to perform the activities of daily living, muscular endurance is more important than absolute muscle strength for most patients. Some strength reserve, however, is needed for unpredictable activities such as a fall, a sudden load to the spine, or quick movements. In sports and heavy physical work, both strength and endurance needs increase. For example, in rapid breathing caused by exertion, there is rhythmic contraction and relaxation of the abdominal wall. A fit person can simultaneously provide spine support with abdominal wall muscles and meet breathing demands, but a less-fit person might not be able to do so and therefore could more easily become injured or have pain.139 This biomechanical model is particularly complex in the spine because of the presence of global movement patterns and segmental movement patterns. Two interrelated muscular tasks must be carried out at the same time: maintaining overall posture and position of the spine, and control of individual intersegmental relationships. Sufficient but not excessive joint stiffness is required at the segmental level to prevent injury and allow for efficient movement. This stiffness is achieved with specific patterns of muscle activity, which differ depending on the position of the joint and the load on the spine. The inability to achieve this stiffness, and the resulting segmental problems, is thought to be a factor in low back pain.178
Muscular Imbalances and Neural Procession Problems
There appear to be consistent muscular problems in patients with chronic low back pain. Some of these factors might exist preinjury and make the spine more susceptible to injury, and some are adaptations to injury. Just as is seen in other areas of the body (such as the knee), muscle function and strength around the spine are altered after injury.177 Studies have shown abnormal firing patterns in the deep stabilizers of the spine and transversus abdominus with activities such as limb movements, accepting a heavy load, and responding to balance challenges. Other researchers have found strength ratio abnormalities and endurance deficits in patients with low back pain, such as abnormal flexion to extension strength ratios and lack of endurance of torso muscles.140
Studies of lumbar paraspinals have found several abnormalities in patients with low back pain. Multiple imaging studies have demonstrated paraspinal muscle atrophy, particularly of the multifidi, in patients with chronic low back pain.178 Recovery of the multifidi does not appear to occur spontaneously with the resolution of back pain.91 Biopsies of multifidi in patients with low back pain also show abnormalities. Atrophy of type 2 muscle fibers is found, and internal structural changes of type 1 fibers that give them a moth-eaten appearance are seen. In a study of patients undergoing surgery for lumbar disk herniations with duration of symptoms from 3 weeks to 1 year, multifidi biopsies collected at the time of surgery showed type 2 muscle atrophy and type 1 fiber structural changes. Biopsies were repeated 5 years postoperatively. Type 2 fiber atrophy was still found in all patients, in both those who had improved with surgery and those who had not. In the positive outcome group, however, the percentage of type 1 fibers with abnormal structures had decreased, and in the negative outcome group there was a marked increase in abnormal type 1 fibers.175 Increasingly strong scientific support is found for the multifactorial nature of low back pain, which includes both structural and dynamic factors.
Psychosocial Factors and Low Back Pain
Pain is an individual experience, and biomechanical and neurologic factors alone do not explain much of the variance seen clinically in patients with back pain. Multiple psychosocial factors have been found to play a role in low back pain. This is briefly discussed here and more thoroughly discussed in the chapter on chronic pain (see Chapter 42), as these issues are shared by multiple painful conditions and not just low back pain.
Depression, Anxiety, and Anger
It appears that between 30% and 40% of those with chronic back pain also have depression.115 This rate is so high because depressed patients are more likely to develop back pain and to become more disabled by pain, and because some patients with persistent pain become depressed. Patients who are depressed are at increased risk of developing back and neck pain. In a recent analysis of factors leading to the onset of back and neck pain, those in the highest quartile for depression scores had a fourfold increased risk of developing low back pain than those in the lowest quartile for depression scores.39 Strong evidence also shows that psychosocial factors are closely linked to the transition from acute pain to chronic pain and disability. In a study of 1628 patients with back pain seen at a pain clinic, those with a comorbid diagnosis of depression were more than 3 times more likely to be in the worst quartiles of physical and emotional functioning on the 36-Item Short-Form Health Survey than those who were not depressed.70 Multiple other studies have found that depression, anxiety, and distress are strongly related to pain intensity, duration, and disability.118
Research has also shown a high correlation with anger measurements and pain, thought to be related to deficient opioid modulation in those with high anxiety, anger, and fear reactivity.32 Patients with posttraumatic stress disorder have a high incidence of chronic low back pain as well.201
Patient Beliefs About Pain and Pain Cognition
Beliefs about back pain can be highly individual and are often not based on facts. Some patients with back pain, especially those with chronic low back pain that keeps them from working, have a great deal of fear about back pain. These include fears that their pain will be permanent, that it is related to activity, and that exercise will damage their back. This set of beliefs is referred to as fear avoidance. For example, studies have found that patients with chronic low back pain who perform poorly on treadmill exercise tests,191 walk slower on treadmill tests,2 and perform more poorly on spinal isometric exercise testing3 were the ones with more anticipation of pain than those who did well on these tests. Fear-avoidance beliefs rather than actual pain during testing predicted their performance. Fear-avoidance levels explain self-reported disability and time off work more accurately than actual pain levels or medical diagnosis does.127 This finding has led Waddell and other experts to state that “the fear of pain may be more disabling than pain itself.”234
A large, population-based study found that subjects with high levels of pain catastrophizing, characterized by excessively negative thoughts about pain and high fear of movement and injury or reinjury (kinesophobia), who had back pain at baseline were much more likely to have especially severe or disabling pain at follow-up evaluation compared with those who did not catastrophize. For those without back pain at the initial questionnaire, catastrophizers were more likely to have developed low back pain with disability at follow-up evaluation than noncatastrophizers.171 Thought processes, such as the presence of catastrophizing, are not limited to back pain and are often part of a larger pattern of relationships and thought processes.
Patients’ beliefs about pain and their approach to dealing with pain have been consistently found to affect outcomes. Fortunately, changes in these beliefs and cognitive patterns are possible. Multidisciplinary pain programs have proven effective in decreasing fear-avoidant beliefs and catastrophizing (see Chapter 42).205
These changes in beliefs can also improve function. For example, a study in which a group of patients with chronic low back pain underwent a cognitive behavioral treatment program found that, although there were not significant changes in pain intensity, those with reductions of fear-avoidance beliefs had significant reductions in disability. Changes in fear-avoidant beliefs accounted for 71% of the variance in reduction in disability in this study.252
Centralization and Pain
The experience of nociception is processed by the body in complex ways. The theory that pain is a simple loop from injury to perception of injury is much too simplistic. Pain processing begins in the spinal cord and continues extensively in the brain, and the ultimate pain that someone experiences is the sum of multiple descending and ascending faciliatory and inhibitory pathways. Extensive evidence now supports the theory that persistent pain might be caused by central sensitization, which could help explain why often no pain generator is found in chronic low back pain.46
The History and Physical Examination of the Low Back
The History
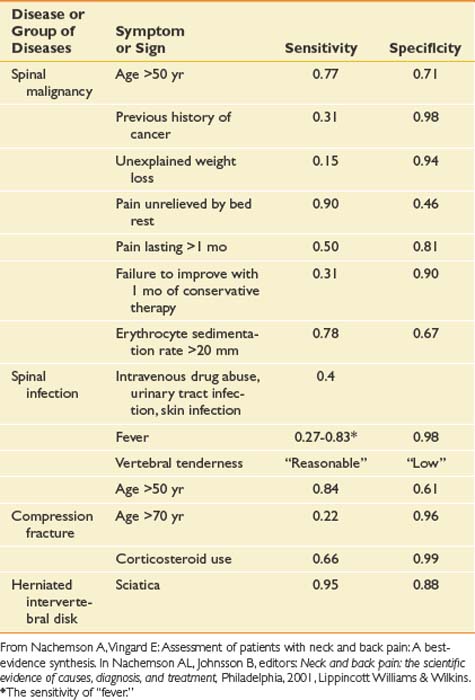
As with any pain history, features of back pain that should be explored include location; character; severity; timing, including onset, duration, and frequency; alleviating and aggravating factors; and associated signs and symptoms. Each of these features can assist the clinician in obtaining a diagnosis and prognosis and determining the appropriate treatment. The causes of back pain are often very difficult to determine. For as many as 85% of patients, no specific cause for back pain is found.50 One of the main purposes of the history is to rule out rare but serious causes of back pain. Elements of historical information that suggest a serious underlying condition as the cause of the pain such as cancer, infection, long tract signs, and fracture are called red flags (Box 40-2). When these are present, further workup is necessary (Table 40-1).
Table 40-1 Sensitivities and Specificities of Different Elements of the History and Examination for Some Specific Causes of Low Back Pain
Besides determining a diagnosis, a purpose of the history is to explore the patient’s perspective and illness experience. Certain psychosocial factors are valuable in determining prognosis (Box 40-3). Factors such as poor job satisfaction, catastrophic thinking patterns about pain, the presence of depression, and excessive rest or downtime are much more common in patients in whom back pain becomes disabling. These are called yellow flags because the clinician should proceed with caution, and further psychologic evaluation or treatment should be considered if they are present. Some of these psychosocial factors are addressed by specific questions, and some become evident through statements that patients make during the history as they describe their illness experience. Questions about, for example, what patients believe is causing the pain, their fear and feelings surrounding this belief, their expectations about the pain and its treatment, and how back pain is affecting their lives (including work and home life) can yield valuable information. Many of these yellow flags are better prognostic indicators than the more traditional medical diagnoses.235
The Physical Examination
Table 40-2 outlines a thorough examination of the lumbar spine.
Table 40-2 Physical Examination for Low Back Pain
| Examination Component | Specific Activity | Reason for This Part of the Examination |
|---|---|---|
| Observation | Observation of overall posture | Determine whether structural abnormality or muscle imbalances are present |
| Observation of lumbar spine | Further define muscle imbalance and habitual posture | |
| Observation of the skin | Search for diagnoses such as psoriasis, shingles, or vascular disease as cause of the pain | |
| Observation of gait | Screen the kinetic chain and determine whether muscular, neurologic, or joint problems are contributing to symptoms | |
| Palpation | Bones | Search for bony problems such as infection or fracture |
| Facet joints | Identify whether specific levels are tender | |
| Ligaments and intradiskal spaces | Determine whether these are tender | |
| Muscles | Search for trigger points, muscle spasms, muscle atrophy | |
| Active range of motion | Forward flexion | Amount, quality if painful |
| Extension | — | |
| Side bending | Same, also side to side differences | |
| Rotation | — | |
| Neurologic examination | Manual muscle testing of L1–S1 myotomes | Determine weakness |
| Pinprick and light touch sensation, L1–S1 dermatomes | Determine sensory loss | |
| Reflexes: patellar, hamstring, Achilles | Test injury to L4, L5, or S1 roots if diminished, upper motor neuron disease if brisk | |
| Balance and coordination testing | Signs of upper motor neuron disease | |
| Plantar responses | Same | |
| Straight leg raise | Neural tension at L5 or S1 | |
| Femoral nerve arch | Neural tension at L3 or L4 | |
| Orthopedic special tests | Abdominal muscle strength | Determines weakness and deconditioning |
| Pelvis stabilizer strength, i.e., gluteus medius, maximus, etc. | Determines weakness and deconditioning | |
| Tightness or stiffness of hamstrings | Determines areas of poor flexibility | |
| Tightness or stiffness of hip flexors | — | |
| Tightness or stiffness of hip rotators | — | |
| Prone instability test | Signs of instability |
Observation
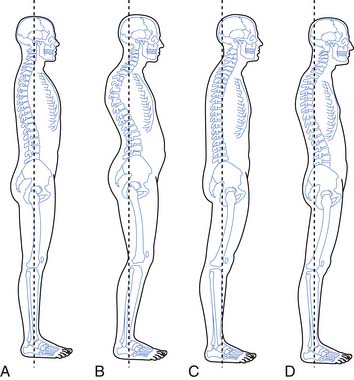
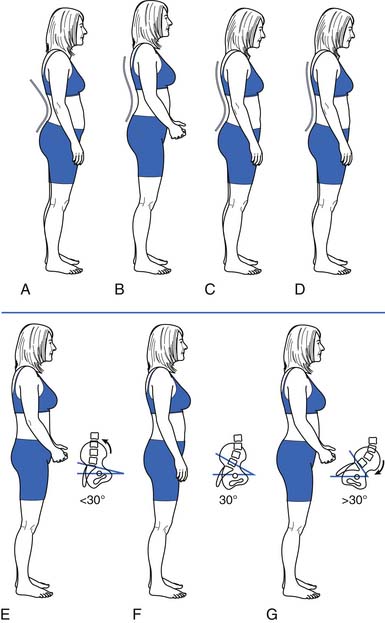
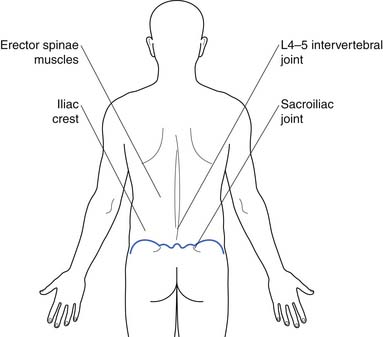
Observation should include a survey of the skin, muscle mass, and bony structures, as well as observation of overall posture (Figures 40-13 and 40-14), and the position of the lumbar spine in particular. Gait should also be observed for clues regarding etiology and contributing factors.
Palpation
Palpation should begin superficially and progress to deeper tissues. It can be done with the patient standing. To ensure that the back muscles (Figure 40-15) are fully relaxed, palpation is often done with the patient lying prone, perhaps with a pillow under the abdomen to slightly flex the spine into a position of comfort. It should proceed systematically to determine what structures are tender to palpation.
Range of Motion
Quantity of Range of Motion
Several methods can be used to measure spinal range of motion (ROM). These include using a single or double inclinometer; measuring the distance of fingertips to floor; and, for forward flexion, the Schober test (measuring distraction between two marks on the skin during forward flexion). Of these methods, the double inclinometer has been shown to correlate the closest to measurements on radiographs.77,210 Fingertip to floor has good interrater and intrarater reliability, but this takes into account the movement of the pelvis and is affected by structures outside the spine, such as tight hamstrings.168 The Schober test is commonly used to assess a decrease in forward flexion in ankylosing spondylitis. It is sensitive for this condition but is not specific. General figures for normal ROM are forward flexion, 40 to 60 degrees; extension, 20 to 35 degrees; lateral flexion, 15 to 20 degrees; and rotation, 3 to 18 degrees. Studies to determine normal ROM in asymptomatic adults have found large variations within the normal range.165 It is unclear what the significance of decreased ROM is in patients with back pain because many people without back pain also have limited range. ROM can also change depending on the time of day, the effort the patient expends, and many other factors.255
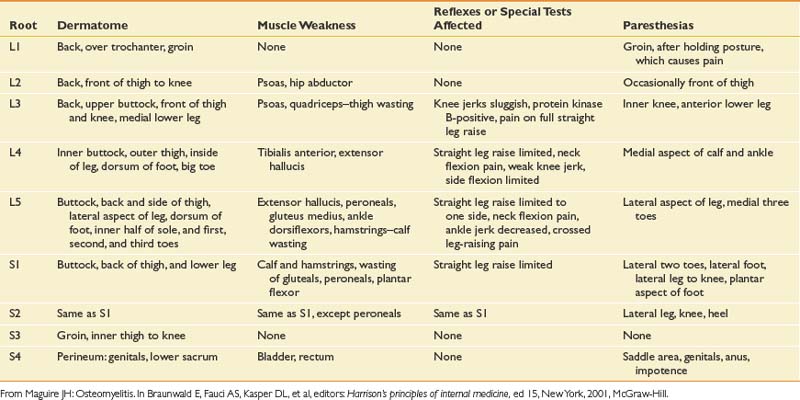
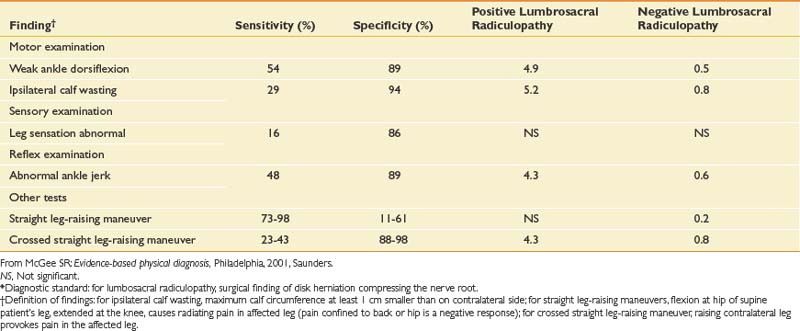
The Neurologic Examination
The neurologic examination of the lower limbs can rule out clinically significant nerve root impingement and other neurologic causes of leg pain (Tables 40-3 and 40-4). The physical examination should logically proceed to discover whether a particular root level is affected by combining the findings of weakness, sensory loss, diminished or absent reflexes, and special tests such as straight leg-raising sign. Upper motor neuron abnormalities should also be ruled out. The accuracy of the neurologic examination in diagnosing herniated disk is moderate. The accuracy can be increased considerably, however, with combinations of findings.50 The sensitivity and specificity of different findings for lumbar radiculopathy have been well studied (Table 40-5).
Table 40-3 Factors That Affect Posture
| Reason for Abnormality | Clinical Example |
|---|---|
| Bone structure | Compression fractures |
| Scheuermann disease | |
| Ligamentous laxity | Hyperextension of the knees, elbows |
| Muscle and fascial length | Tight hamstrings that cause a posterior pelvic tilt |
| Weak and long abdominal muscles that allow an anterior pelvic tilt | |
| Body habitus | Obesity or pregnancy causes changes in force and increased lumbar lordosis |
| Neurologic disease | Spasticity causes an extension pattern of the lower limb |
| Mood | Depression causes forward slumped shoulders |
| Habit | Long-distance cyclists have increased thoracic kyphosis and flat spine from prolonged positioning while riding |
Orthopedic Special Tests to Assess for Relative Strength and Flexibility
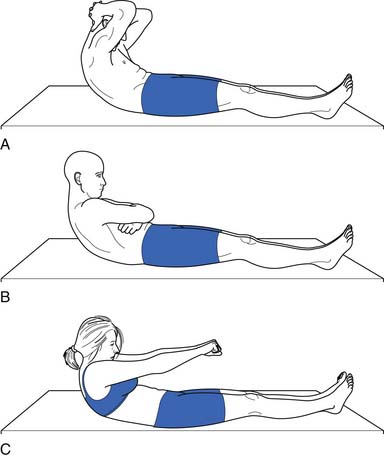
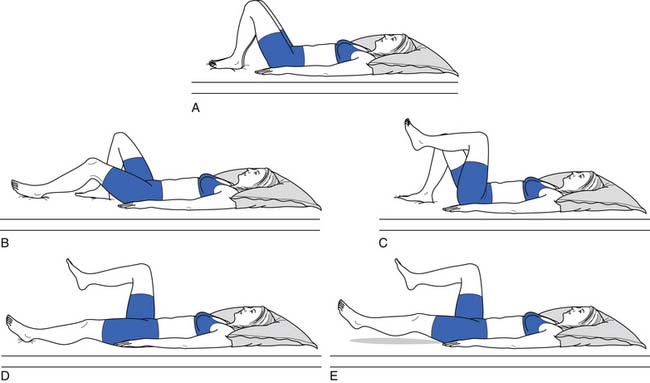
Because of their stabilizing effect on the spine, abdominal muscle strength and endurance is important. Several different ways can be used to measure abdominal muscle strength and control (Figures 40-16 and 40-17). One grading system assesses whether the patient is able to maintain a neutral spine position while adding increasingly more challenging leg movements(Figure 40-18).
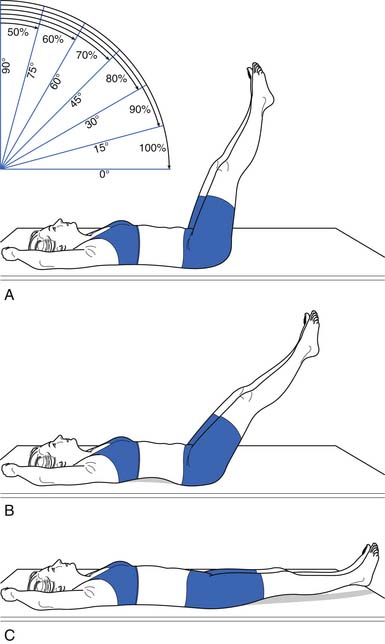
FIGURE 40-17 Leg lowering: grading. In the second test, the patient raises the legs one at a time to a right angle, and then flattens them back on the table. The patient slowly lowers the legs while holding the back flat. A 100% or normal grade is the ability to hold the low back flat on the table as the legs are lowered to the fully extended position. An 80% or good grade is the ability to hold the low back flat and lower the legs to a 30-degree angle. A, A 60% or fair plus grade is the ability to lower the legs to 60 degrees with the low back flat. B, The pelvis tilted anteriorly and the low back arched as the legs were lowered. C, The final position. Kendall notes that this second test is more important than the first (see Figure 40-16) in grading muscles essential to proper posture, and that often patients who do well on the first test do poorly on the second.
(Modified from Kendall FP, McCreary EK: Trunk muscles in muscle testing and function, Philadelphia, 1983, Williams and Wilkins.)
Orthopedic Special Tests for Lumbar Segmental Instability
Passive Intervertebral Motion Testing
The patient lies prone. The examiner applies a firm steady pressure over the spinous process anteriorly and assesses the amount of vertebral motion and whether pain is provoked.90
Prone Instability Test
The patient lies prone, with the torso on the examining table and the legs over the edge of the table with the feet resting on the floor. The examiner performs passive intervertebral motion testing at each level and notes provocation of pain. Then the patient lifts the legs off the floor, and the painful levels are repeated. A positive test is when the pain disappears when the legs are lifted off the table. This is because the extensors are able to stabilize the spine in this position.90,138
Examining the Area Above and Below the Lumbar Spine
Generally in musculoskeletal medicine, the joint above and the joint below the painful area should be assessed to make sure nothing is missed. This is a good idea for the examination of the lumbar spine as well. ROM of the hip joints should be assessed, and a quick screen of the knee and ankle joint can determine whether pathology in these areas is contributing to the back problem. The thoracic spine can be quickly screened as well during ROM and palpation.
Illness Behavior and Nonorganic Signs Seen on Physical Examination
Multiple reasons can explain why patients with back pain might display symptoms out of proportion to injury. Illness behaviors are learned behaviors and are responses that some patients use to convey their distress. Several studies have found that patients with chronic low back pain and chronic pain syndrome experience significant anxiety during the physical examination, even to the level experienced during panic attacks. This complicates the assessment by altering the clinical presentation of the condition. This anxiety is generally manifest as avoidance behavior, such as decreased ROM or poor effort with muscle testing.81 Other reasons for illness behavior include a desire to prove to physicians how disabling the pain is and malingering. One way to assess for illness behavior on physical examination is to perform parts of the examination to search for Waddell’s signs. Waddell’s signs are forms of illness behavior.234 They are nonorganic findings on physical examination that correlate with psychologic distress. They are as follows:
Clinical Evaluation: Diagnostics
Imaging Studies
Plain Radiography
Conventional radiographs are indicated in trauma to evaluate for fracture and to look for bony lesions such as tumor when red flags are present in the history. As an initial screening tool for lumbar spine pathology, however, they have very low sensitivity and specificity.73 Anterior–posterior and lateral views are the two commonly obtained views. Oblique views can be obtained to examine for a spondylolysis by visualizing the pars interarticularis and the “Scottie dog” appearance of the lumbar spine (Figure 40-19). Lateral flexion–extension views are obtained to check for dynamic instability, although the literature does not support their usefulness.55 They are potentially most helpful from a surgical screening perspective when evaluating a spondylolisthesis. They are commonly obtained in posttrauma and postsurgical patients.
Magnetic Resonance Imaging
MRI is the preeminent imaging method for evaluating degenerative disk disease, disk herniations, and radiculopathy (Figure 40-20) (see also Chapter 7). On T2-weighted imaging, the annulus can be differentiated from the internal nucleus, and annular tears can be seen as high-intensity zones. These zones are of unclear clinical significance but are thought to be potential pain generators.
Adding gadolinium contrast enhancement helps to identify structures with increased vascularity. Contrast is always indicated in evaluating for tumor or infection or to determine scar tissue (vascular) versus recurrent disk herniation (avascular) in postsurgical patients with recurrent radicular symptoms.
The downside of MRI is that, although it is a very sensitive test, it is not very specific in determining a definite source of pain. It is well established that many people without back pain have degenerative changes, disk bulges, and protrusions on MRI. Boden et al.21 demonstrated that one third of 67 asymptomatic subjects were found to have a “substantial abnormality” on MRI of the lumbar spine. Of the subjects younger than 60 years, 20% had a disk herniation, and 36% of those older than 60 had a disk herniation and 21% had spinal stenosis. Bulging and degenerative disks were even more commonly found. In another study of lumbar MRI findings in people without back pain, Jensen et al.97 demonstrated that only 36% of 98 patients had normal disks. They found that bulges and protrusions were very common in asymptomatic subjects, but that extrusions were not. In a more recent study in 2001, Jarvik confirmed these findings.96
Computed Tomography
Because of the resolution of anatomic structures in MRI, it has essentially replaced computed tomography (CT) scanning as the imaging study of choice for low back pain and radiculopathy. CT scanning is still more useful than MRI, however, in evaluating bony lesions. CT scans are also useful in the postsurgical patient with excessive hardware that can obscure MRIs, and in patients with implants (aneurysm clips or pacemakers) that preclude MRI.
Myelography
In myelography, contrast dye is injected into the dural sac and plain radiographs are performed to produce images of the borders and contents of the dural sac (Figure 40-21). CT images can also be obtained after contrast injection to produce axial cross-sectional images of the spine that enhance the distinction between the dural sac and its surrounding structures. This is typically reserved as a potential presurgical screening tool but has been used less with the advancement of MRI.
Scintigraphy
Radionuclear bone scanning is a fairly sensitive but not specific imaging modality that can be used to detect occult fractures, bony metastases, and infections. To increase anatomic specificity, single-photon emission computed tomography (SPECT) bone scanning is used to obtain bone scans with axial slices. This allows the diagnostician to differentiate uptake in the posterior elements from more anterior structures of the spine. The diagnostic use of this study with regard to altering clinical decision-making is controversial. Studies have been published demonstrating that the use of SPECT can help identify patients with low back pain who might benefit from Z-joint injections.172
Electromyography
Electromyography is useful in evaluating radiculopathy because it provides a physiologic measure for detecting neurogenic changes and denervation with good sensitivity and high specificity. It can help to provide information as to which anatomic lesions found in imaging studies are truly physiologically significant.181 See Chapters 9 through 11 for further details.
Differential Diagnosis and Treatment: The Prototype of Back Pain Greater Than Leg Pain
Mechanical Low Back Pain
Nearly 85% of those who seek medical care for low back pain do not receive a specific diagnosis.50 The majority of these patients most probably have a multifactorial cause for back pain, which includes deconditioning; poor muscle recruitment; emotional stress; and changes associated with aging and injury such as disk degeneration, arthritis, and ligamentous hypertrophy. This type of back pain can be given many names; simple backache, nonspecific low back pain, lumbar strain, and spinal degeneration are a few of the common names for this condition. The name given to a condition sends certain messages to the patient who receives the diagnosis. The term simple backache might cause a patient to think that the physician misunderstands because, from the patient’s perspective, the pain is not simple if it has not resolved in a few days. The label nonspecific low back pain can cause the patient to continue to seek care from multiple providers to receive a specific diagnosis. Lumbar strain suggests that the condition was caused by overactivity, which is often not the case, and that further physical activity would cause it to recur, which is not true. Spinal degeneration sends the message that the changes are permanent and will probably worsen.235 The term mechanical low back pain is perhaps the best term for this multifactorial axial backache. It suggests the mechanism of injury better than terms such as strain or sprain, and it does not imply permanence.
The biomechanics of the spine are not unlike the biomechanics of other systems, in that longevity of the components and efficiency of the system depend on precise movements of each segment. In the spine, this means both an alignment in sustained postures and movement patterns that reduce tissue strain and allow for efficient muscle action without trauma to the joints or soft tissue.189 Clinicians and researchers alike theorize that when alignment and movement patterns deviate from the ideal, degeneration and tissue overload is more likely. This is analogous to the abnormal tire wear that occurs on a car when the wheels are out of alignment. Unlike machinery, the body can adapt over the course of time to stress on the segments. This adaptation can be the healthy response of tissue to loading (as is seen with exercise), such as muscle hypertrophy or increased bone density. It can also, however, begin a cycle of microtrauma that can lead to macrotrauma.125,140,189 The theoretic model for this approach is strong, and research is beginning to validate many of these concepts, although this is not easy given the complex nature of the system.
Treatment of Low Back Pain
Reassurance and Patient Education
Education should include providing as much of an explanation as patients need in terms they can understand. The physician should also provide empathy and support and impart a positive message. Reassurance that there is no serious underlying pathology, that the prognosis is good, and that the patient can stay active and get on with life despite the pain can help counter negative thoughts and misinformation that the patient might have about back pain.235
Strong evidence from systematic reviews indicates that the advice to continue ordinary activity as normally as possible fosters faster recovery and can lead to less disability than the advice to rest and “let pain be your guide.”236 It is controversial whether patients with low back pain fare better with a specific diagnosis or not. Education and explanations, however, should be adequate. As Waddell states in his book The Back Pain Revolution, “Simply saying that ‘I can’t find anything wrong’ might imply that you are not sure and make patients worry more!”235 On the other hand, some diagnoses carry negative messages to patients that suggest permanent damage and the need to “get fixed,” such as degenerative disk disease or arthritis.235 Mechanical low back pain is a useful diagnostic term because it implies the mechanism of the pain and the way it is best treated without suggesting permanence.
Beyond a diagnosis, there is other information that patients want about low back pain. In a study of patients who presented with low back pain to their primary care doctors in a health maintenance organization setting, the information that patients wanted from their doctor included the likely course of their back pain, how to manage their pain, how to return to usual activity quickly, and how to minimize the frequency and severity of recurrences. They ranked each of these areas of education a higher priority than finding a cause or receiving a diagnosis for their pain.235 Providing this information in an amount and in a way that patients can understand helps build a therapeutic doctor–patient relationship and, it is hoped, helps reduce anxiety and speed recovery.
Back Schools
The term back school is generally used for group classes that provide education about back pain. The content and length of these classes varies a great deal, but generally they include information about the anatomy and function of the spine, common sources of low back pain, proper lifting technique and ergonomic training, and sometimes advice about exercise and remaining active. Studies have generally found back schools to be effective in reducing disability and pain for those with chronic low back pain.224
Exercise
No well-controlled studies show that exercise is effective for the treatment of acute low back pain. Many practitioners believe that exercise for patients with acute low back pain is appropriate to prevent deconditioning, to reduce the chance of recurrence of symptoms, and to reduce the risk of the development of chronic pain and disability. This is consistent with rehabilitation principles for other acute injuries, such as sports-related injuries or rehabilitation after joint replacement surgery.239 This principle is not yet supported by scientific research, perhaps because of problems with long-term exercise compliance, the overall favorable prognosis for each episode of acute back pain, or the outcome measures used.
Multiple high-quality studies have found, however, that exercise results in positive outcomes in the treatment of chronic low back pain.226 This includes pain relief (although this relief is modest, with a recent metaanalysis of 43 trials showing a mean difference of 10 points on a 100-point scale), improvement in function, and slightly reduced sick leave.43,87 It appears that the most effective exercise for low back pain includes an individualized regimen learned and performed under supervision that includes stretching and strengthening.87 This is not surprising because it is generally believed that the purpose of exercises for the treatment of low back pain is to strengthen and increase endurance of muscles that support the spine and improve flexibility in areas where this is lacking. This is combined with motor retraining to establish normal patterns of muscle activity, and treatment of deficits of the kinetic chain that interfere with biomechanical efficiency. One reason that studies have not been able to determine what exercises are best for patients with low back pain could be that multiple forms of exercise can achieve the goal of restoring function and regaining physical fitness.116,225,239
The exact dose of exercise, how much exercises should be advanced, and the ideal length of supervised treatment is not known. Because endurance is a significant problem with many patients with persistent back pain, activity levels should be increased in planned, fixed increments based on realistic goals rather than on symptoms. This is because it is normal in the course of low back pain that there will be temporary exacerbations of pain along the way. Beyond the physiologic benefits of exercise, increasing activity has positive effects on beliefs and behaviors about pain. Small doses of exercise that are not sufficient to cause physiologic change have been found to increase function and decrease pain. When specifically studied, this appeared to be from decreased fear-avoidance beliefs and reduced anxiety. By exposing fearful patients to physical activity through gradually increasing activity levels despite pain, they receive positive reinforcement by meeting goals, and personal experience can reduce fear of movement, reinjury, and catastrophizing.22 Adverse effects of exercise for low back pain are rarely reported, so it is generally a very safe form of treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree