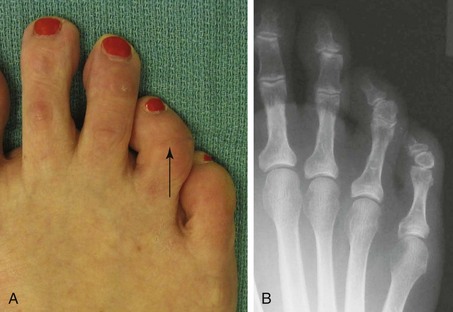
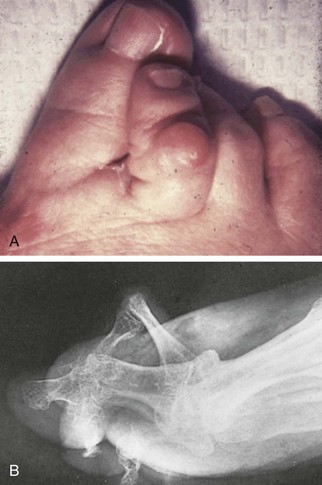
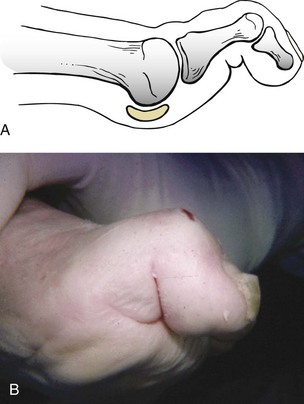
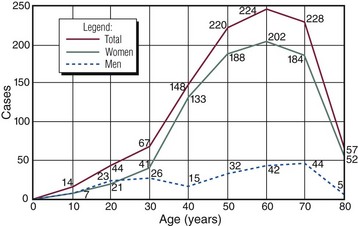
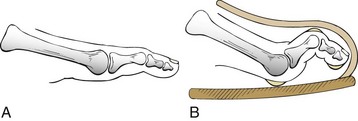
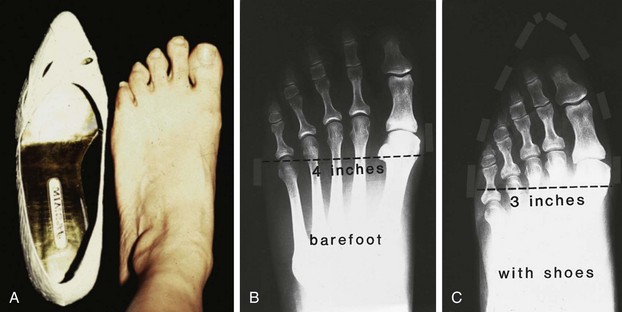
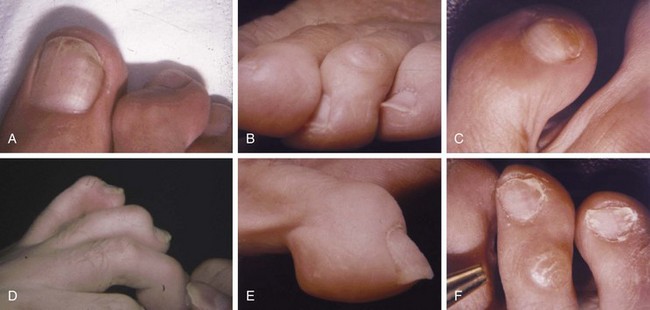
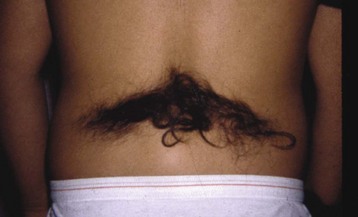
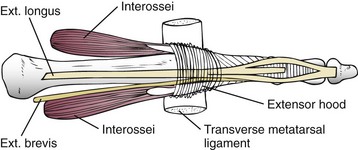
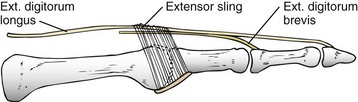
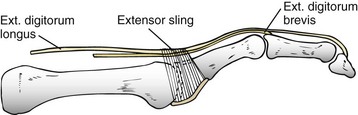
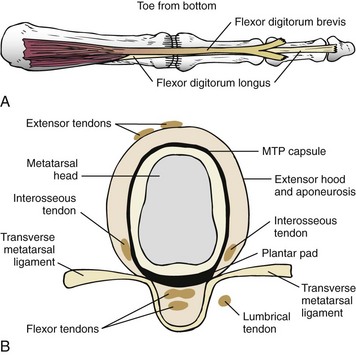
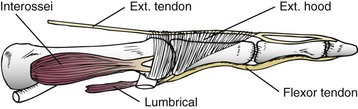
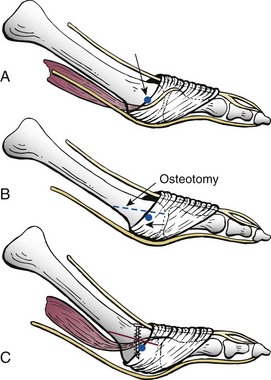
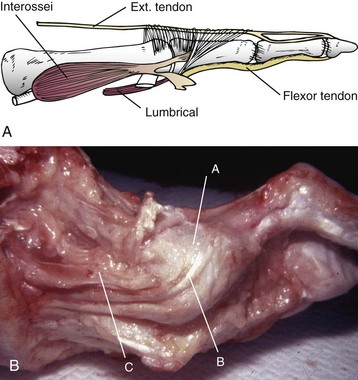
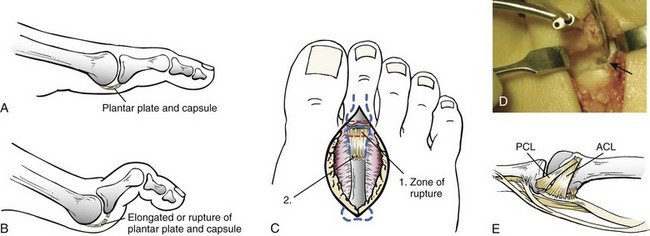
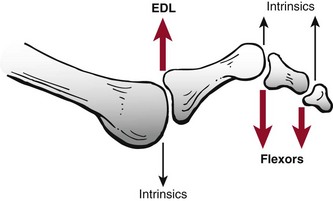
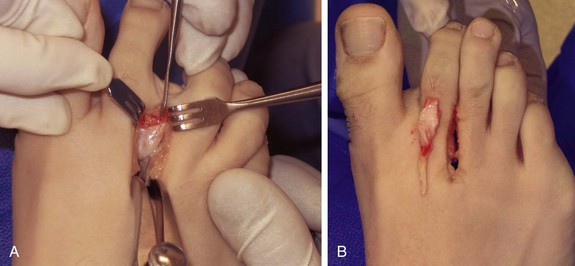
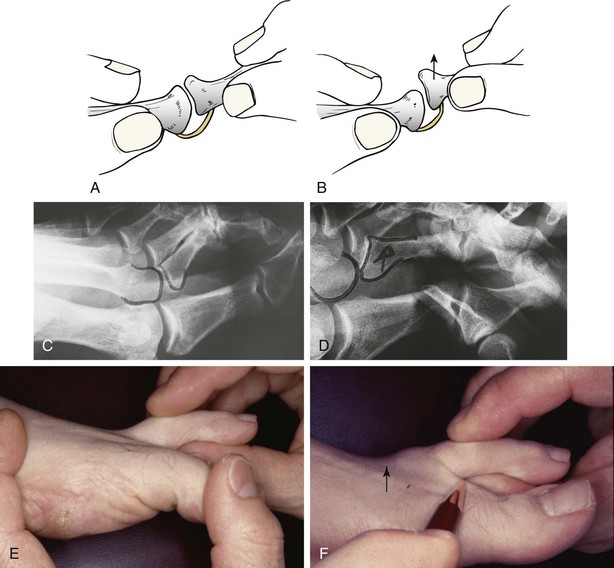
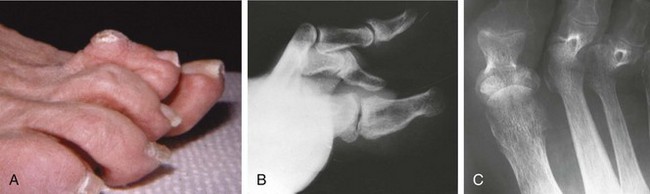
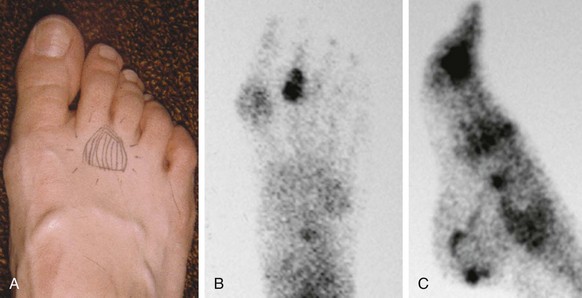
Chapter 7 FIXED HAMMER TOE DEFORMITY (Video Clip 75, 76 FLEXIBLE HAMMER TOE DEFORMITY (Video Clip 77 MALLET TOE DEFORMITY (Video Clip 74 CLAW TOE DEFORMITIES (Video Clip 75 SUBLUXATION AND DISLOCATION OF THE LESSER METATARSOPHALANGEAL JOINT MILD OVERLAPPING FIFTH TOE DEFORMITIES SEVERE OVERLAPPING FIFTH TOE DEFORMITIES (Video Clip 73 KERATOTIC DEFORMITIES OF LESSER TOES Lesser toe deformities can be static or dynamic. They can occur as isolated entities or be associated with deformities of the hallux, midfoot, or hindfoot. Poor footwear is the most commonly attributed cause of lesser toe deformities, but they also can be due to heritable causes or can result from congenital and neuromuscular conditions.32,35,40,45,46,204 The terms hammer toe, mallet toe, and claw toe have been used interchangeably by various authors in describing deformities of the toes, and their definitions have been confusing. The nomenclature adopted for this book is simple, and to a certain extent, it follows that used to describe deformities of the fingers. A mallet toe involves the distal interphalangeal (DIP) joint; the distal phalanx is flexed on the middle phalanx (Fig. 7-1). A simple hammer toe involves the proximal interphalangeal (PIP) joint; the middle and distal phalanges are flexed on the proximal phalanx (Fig. 7-2A). A complex hammer toe typically involves one toe and consists of a flexion deformity of the PIP joint and hyperextension deformity of the metatarsophalangeal (MTP) joint (Figs. 7-2B and 7-3). A claw toe involves a hammer toe deformity of the phalanges and dorsiflexion (extension) deformity at the MTP joint (Fig. 7-4).212 To some extent, there is an overlap in the definitions of complex hammer toes and claw toes; however, claw toes usually involve all of the lesser toes and often have an underlying neuromuscular cause. With regard to the great toe, a hammer toe can involve the interphalangeal joint. No mallet toe deformity exists in the hallux (Fig. 7-5). A claw toe deformity, which is essentially synonymous with a cock-up deformity of the great toe, occurs when there is also hyperextension of the MTP joint. These deformities of the lesser toes range in severity from a mild and easily correctable flexible deformity to a rigid and fixed contracture. In most cases, these deformities are acquired. Both the mallet toe and the hammer toe deformities can occur in one or several toes of the same foot35,40,45; a claw toe deformity often involves multiple toes but can occur as an isolated entity.39 These deformities occur with varying frequency among different populations, but they are much more common in shoe-wearing societies. The literature dealing with deformities of the forefoot in populations that rarely wear shoes rarely mentions the mallet toe, hammer toe, or claw toe deformities.5,71,111,233 In various surveys regarding the incidence of these deformities among industrial workers54,128 and military male recruits,102,105 the incidence of hammer toe and claw toe deformities ranged from 2% to 20%. All of these studies seem to indicate that the deformities develop slowly and insidiously and that their incidence increases almost linearly with age, peaking in the sixth and seventh decades.* These deformities occur much more commonly in women than in men (4 to 5 : 1).26,40,45,46,51 A hammer toe deformity rarely is seen in infants (Fig. 7-6).104 The incidence of forefoot surgery is unknown, but in studies of specific regional populations, Shirzad et al210 suggested these deformities constitute between 28% and 48% of all forefoot surgery. Footwear is generally considered to play an important role in the etiology of hammer toe and mallet toe deformities.32,40,45 Placing the forefoot into the constricted confines of a pointed shoe no doubt plays a major role in the onset of these deformities. The toes, to conform to a small toe box, must of necessity buckle (Fig. 7-7). This fact explains why acquired mallet toes and hammer toes are among the most common deformities of the forefoot in shoe-wearing societies (Fig. 7-8). DuVries66 thought that shoes restrict the normal movement of the joints and impedes the actions of the intrinsic muscles of the foot. It must be kept in mind, however, that anatomic predisposing factors vary extensively, and a large number of shoe wearers do escape deformities of the forefoot. Other than its general relationship to pressure of the toe against the shoe, the specific cause of a mallet toe is unknown. Although most often idiopathic in nature, it can develop after a hammer toe repair or trauma,40,130 or it can be associated with inflammatory arthritis.40,41 A mallet toe can also develop after a hammer toe repair, possibly because of scarring on contracture of the long flexor tendon. The high incidence of mallet toe in the female population has led to speculation that a constricting toe box is a causative factor.34,39,40 Female subjects constituted 84% of the patient population in one reported series,42 the gender difference being highly significant. Brahms21 stated that a mallet toe is often limited to one toe, although Mann and Coughlin140 noted that the deformity can occur in more than one toe. Coughlin40 noted in his report (60 patients, 86 toes) that although 65% of patients had single toe involvement, 18% of patients had multiple toe involvement, with three to five toes affected. A mallet toe occurs with equal frequency in the second, third, and fourth toes,40 but most often the involved toe is longer than the adjacent toes (Fig. 7-9). Because of pressure against the end of the shoe, the toe becomes plantar flexed at the DIP joint. Tightness of the flexor digitorum longus tendon in patients with a mallet toe deformity can be demonstrated, but whether this tightness is a primary cause or a secondary change is not known. In young children, a tight flexor tendon can result in a flexion deformity of the PIP and DIP joint. This pediatric deformity has been termed a curly toe* and may also be associated with a delta-shaped phalanx.58 The major symptoms leading to surgical repair in the adult population include discomfort because of pressure on the tip of the toe, with callus formation or dorsal pain over the DIP joint.† Preoperative nail deformities occurred in 7% of mallet toes in Coughlin’s series, and 93% were noted to have dorsal pain or pain at the tip of the toe, with callus formation (Figs. 7-10B and F and 7-11C and D). The causes of a hammer toe appear to be multifactorial. The high incidence of hammer toes in the female population has led some to suggest that a constricting toe box is also a causative factor of this deformity.17,37,51,201 Coughlin45 reported that 62% of the patients in his series considered ill-fitting shoes to be a cause of their hammer toe deformity. The high incidence of female involvement has been previously reported26,51,188,196,201; females constituted 85% of the patient population in a large series,45 the gender difference being highly significant. The incidence of hammer toes is reported to increase with increasing age,26,51,201 with the peak incidence in the fifth through seventh decades. Coughlin45 noted in his report (67 patients, 118 toes) that 30% had only single toe involvement, and 40% had three or more toes involved. Although Reece,188 Coughlin,45 and others202,203,228 have reported the second toe to be the most commonly involved, Ohm170 reported an equal frequency of occurrence in the second, third, and fourth toes. Coughlin45 noted that increased length in comparison to adjacent digits might be a factor in hammer toe development, although this was not a factor in almost one half of cases. A hammer toe deformity may be caused by a muscle imbalance in association with neuromuscular diseases, such as Charcot-Marie-Tooth disease, Friedreich ataxia, cerebral palsy, myelodysplasia, multiple sclerosis, and degenerative disk disease. The deformity also is seen in patients with an insensate foot associated with diabetes mellitus and Hansen disease.43 Patients with rheumatoid arthritis, psoriatic arthritis, and other types of inflammatory arthritis also can develop a hammer toe deformity.37,39,43 Associated hallux valgus deformities have also been implicated as a cause of hammer toe formation.22,43,202,203 Occasionally, after fractures of the tibia or other trauma,74,203 a progressive hammer toe deformity is observed and is likely the result of nerve or muscle injury from elevated compartment pressures in the involved leg or foot.137 The cause of a claw toe deformity often is unclear, but it may be associated with the same neuromuscular diseases, arthritic deformities, and metabolic diseases that cause hammer toe deformities (Fig. 7-12). In many patients with a severe claw toe deformity, no cause can be identified. A claw toe is a result of muscle imbalance between the intrinsic and extrinsic musculature.157,203 Simultaneous contracture of the long flexors and extensors of the toe, without the modifying action of the intrinsic muscles of the foot, causes the typical deformity seen in this condition (Figs. 7-13 and 7-14).201 Taylor,216 however, found no abnormality of the intrinsic muscles in a series of 68 patients who had claw toes and in whom the muscles were examined by gross inspection, stimulation, and histologic analysis. A claw toe deformity usually involves multiple toes and often both feet (Fig. 7-15).35 The deformity may be either rigid or flexible. It is often associated with a cavus foot, with or without a contracted Achilles tendon. Claw toes are often made worse because the patient cannot find adequate shoes, and a painful bursa develops over the PIP joint. As the claw toe deformity becomes more rigid, the toes strike the top of the shoe and the metatarsal heads are forced plantarward. As the toes subluxate dorsally, the plantar fat pad is pulled distally, and the metatarsal heads become more prominent on the plantar aspect of the foot. This deformity can result in the development of painful plantar callosities, which can ulcerate in severe cases, particularly if sensation of the foot is impaired. The central dorsal structure of the toe is formed by the tendon of the extensor digitorum longus, which divides into three slips over the proximal phalanx; the middle slip inserts into the base of the middle phalanx, and the two lateral slips extend over the dorsolateral aspect of the middle phalanx and converge to form the terminal tendon, which inserts into the base of the distal phalanx (Fig. 7-16).198,199 The tendon is held in a central position dorsally by a fibroaponeurotic sling that anchors the long extensor to the plantar aspect of the MTP joint and to the base of the proximal phalanx. It is surprising that there is no dorsal insertion of the extensor digitorum longus into the proximal phalanx; rather, the phalanx is virtually suspended by the extensor digitorum longus tendon and its extensor sling (Fig. 7-17). The main function of the extensor digitorum longus is to dorsiflex the proximal phalanx (Fig. 7-18). Only when the proximal phalanx is held in flexion or in a neutral position at the MTP joint can this tendon become an extensor of the PIP joint. This concept is important because, with a hammer toe deformity, the long extensor tendon function on the PIP joint may be neutralized by extension of the proximal phalanx.201 The flexor digitorum longus tendon inserts into the distal phalanx and flexes the DIP joint, whereas the flexor digitorum brevis inserts into the middle phalanx, flexing the PIP joint. There is no insertion into the proximal phalanx, so the long flexor tendon influence on the proximal phalanx is minimal (Fig. 7-19A). Resistance to flexion at the MTP joint is maintained in the normal toe by the long extensor. Another important factor is the reactive force of the foot against the ground, which pushes the MTP joint into extension. As a result, with the proximal phalanx in an extended position, there are no major motor antagonists to the long and short flexors; thus the toe buckles, resulting in flexion of the DIP joint and the PIP joint. Over a long period of time, if this position becomes fixed, a hammer toe deformity occurs. The interosseous tendons are located dorsal to the transverse metatarsal ligament, and the lumbricals are located plantar to this ligament (Fig. 7-19B). Both tendons of the intrinsic muscles, however, pass plantar to the axis of motion of the MTP joint, flexing the MTP joint (Fig. 7-20), and pass dorsal to the axis of the PIP joint and DIP joint, extending these joints. This is an important concept to understand when performing a Weil osteotomy of the distal metatarsal; the center of MTP joint rotation is shifted plantarward, effectively making the intrinsic musculature MTP joint dorsiflex, which can lead to the development of a hyperextension deformity of the MTP joint (Fig. 7-21).224,231,232 The plantar and dorsal interossei have only a few fibers that reach the extensor sling and therefore are weak extensors of the interphalangeal joints. The lumbrical, with all of its fibers terminating in the extensor sling, is a stronger extensor of these joints. The interossei flex the proximal phalanx by their direct attachment to the base of the proximal phalanx, whereas the lumbrical achieves flexion by placing tension on the extensor sling (Fig. 7-22). With marked dorsiflexion at the MTP joint, the lumbrical flexion power is quite limited because it is pulling at a 90-degree angle. The most significant stabilizing factor of the MTP joint is the plantar plate, a combination of the plantar aponeurosis and plantar capsule.* During the walking cycle, varying degrees of dorsiflexion occur at the MTP joint. The static resistance of the plantar capsule combines with the dynamic force of the intrinsic flexors to pull the proximal phalanx back into a neutral position at the MTP joint (Fig. 7-23A). With chronic hyperextension forces on the proximal phalanx, the plantar plate can become stretched or attenuated and rendered less efficient (Fig. 7-23B). The lesser MTP joint is stabilized by both the collateral ligaments and the plantar plate.8,61,62 (Fig. 7-23C and D).The plantar plate inserts on the base of the proximal phalanx, but it is attached to the metatarsal head by only a thin layer of synovial tissue that inserts just proximal to the articular surface.61 The distal attachment of the plantar plate is composed of a medial and a lateral bundle. Proximally, the plantar plate forms the major attachment of the plantar aponeurosis. The plantar plate is the central stabilizing structure that determines the position of the flexor digitorum longus. The collateral ligaments are composed of two major structures: the phalangeal collateral ligament (PCL), which inserts onto the base of the proximal phalanx, and the accessory collateral ligament (ACL), which inserts onto the plantar plate (Fig. 7-23E).61 The transverse metatarsal ligament attaches to the adjacent medial and lateral borders of the plantar plate.115 Fortin and Myerson78 reported that the collateral ligaments were the primary stabilizers of the lesser MTP joint. When the collateral ligaments were sectioned in vitro, 48% less force was required to dislocate the lesser MTP joint. When the researchers did an isolated release of the plantar plate, 29% less force was required to dislocate the MTP joint. The position of the proximal phalanx at the MTP joint is subject to the actions of the strong extensor digitorum longus through its sling mechanism, in opposition to the decidedly weaker antagonistic intrinsic muscles and the more static capsule and plantar aponeurosis complex. The positions of the middle and distal phalanges, on the other hand, are subject to the forces of the long and short flexors, which are directly opposed by the weaker intrinsic muscles. At each of these joints, an obvious mismatch can occur, and in each case, the extrinsic muscle overpowers the intrinsic muscle (Fig. 7-24). The sensory status of a foot must be evaluated as well. An impaired sensory status can indicate a systemic disease, such as diabetes, a peripheral neuropathy, or lumbar disk disease. Careful physical examination is necessary to differentiate MTP joint pain from an interdigital neuroma of the adjacent interrmetatarsal space (Fig. 7-25).48,49 Preoperative documentation of sensation is important because a surgical dissection can diminish postoperative sensation. The plantar aspect of the foot is examined for development of intractable plantar keratoses. Callosities can develop in association with contractures of the lesser toes, the result of a buckling effect of the toes. A patient typically complains of pain caused by a callus over the distal aspect of the PIP joint but also can develop pain beneath the tip of the toe or a lesser metatarsal head (Fig. 7-26).45,135 Realignment of the MTP joint and interphalangeal joints can decrease plantar pressure and help relieve symptomatic calluses. The alignment of the MTP joint must be evaluated.201 Medial or lateral deviation of the toe should be noted, as well as an MTP joint hyperextension deformity. The stability of the digit is assessed by the drawer test. The digit is grasped between the thumb and index finger of the examiner, and with the digit slightly dorsiflexed, dorsal pressure is placed on the digit in an attempt to subluxate the MTP joint (Fig. 7-27). Even if the toe is not subluxed, the eliciting of pain with this maneuver is indicative of an intraarticular or periarticular abnormality. (See further discussion under subluxation second MTP joint.) Although the evaluation of a hammer toe deformity may be seen as relatively simple, certain factors must be carefully considered to fully appreciate the nature of the deformity. These include the rigidity of the toe contractures (Fig. 7-28), the position of the MTP joint (Fig. 7-29A), and Achilles tendon tightness with the patient both sitting and standing. Tightness of the flexor digitorum longus tendon must be assessed along with examination of all of the lesser toes. Also, it is important to determine whether there is sufficient space for the involved toe when it is reduced to a normal position. The presence of prior surgical scars can influence the planned surgical exposure. Figure 7-28 A hammer toe deformity is inspected to determine its flexibility. A, Fixed deformity. B, Flexible deformity. Although a physical examination is necessary to define the extent of a lesser toe deformity, radiographic examination is necessary to evaluate the magnitude of the bone deformity (Fig. 7-29B). On an anteroposterior (AP) projection, a severe hammer toe deformity can have the appearance of a gun barrel deformity (Fig. 7-29C) when the proximal phalanx is seen end on. Assessment of the interphalangeal joints is difficult on this projection. Diminution of the MTP joint space can indicate subluxation, and overlap of the base of the proximal phalanx in relation to the metatarsal head can indicate dislocation of the MTP joint (Fig. 7-30). Medial or lateral deviation of the MTP joint can be determined as well. Subchondral erosion, flattening of the articular surfaces, or a Freiberg infraction can indicate the need for further radiographic or laboratory evaluation. A lateral radiograph may be helpful to assess the magnitude of contracture of the interphalangeal joints (see Fig. 7-29B). Stress radiographs can help to determine subluxability of the MTP joint (see Fig. 7-27). Bone scans, computed tomography (CT), and magnetic resonance imaging (MRI) evaluation may also be used to increase information of both osseous and soft tissue abnormalties (Fig. 7-31). A hammer toe deformity may be flexible, semiflexible, or rigid.* If the deformity is flexible, the toe may be passively corrected to a neutral position. However, if the deformity is rigid, joint contractures preclude passive correction. The rigidity of the deformity determines whether conservative or surgical treatment is indicated, as well as the specific surgical procedure that should be performed. The position of the MTP joint when the patient is standing must be carefully evaluated. If a hyperextension deformity is present, correction of only the hammer toe deformity will result in the toe sticking up in an extended position (Fig. 7-32), making shoe wearing difficult. If the MTP joint is subluxated or dislocated, this deformity should be corrected simultaneously with the hammer toe correction.43,72,133,141,179
Lesser Toe Deformities
![]() )
)
![]() )
)
![]() )
)
![]() )
)
![]() )
)
Lesser Toe Deformities
Etiology
Mallet Toe
Hammer Toe
Claw Toe
Anatomy and Pathophysiology
Extensor Digitorum Longus Muscle and Tendon
Interosseous Tendons
Plantar Plate and Collateral Ligaments
Pathophysiology
Preoperative Evaluation
Physical Examination

Radiographic Examination
Fixed Hammer Toe Deformity
Preoperative Planning
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Lesser Toe Deformities