Lateral Condyle Fractures
R. Dale Blasier
Lateral condyle fractures are relatively common in children and occur usually as a result of a fall. The extent of displacement depends on the energy of the injury.
INDICATIONS AND PREOPERATIVE PREPARATION
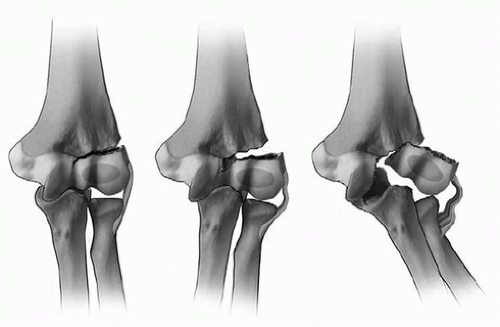
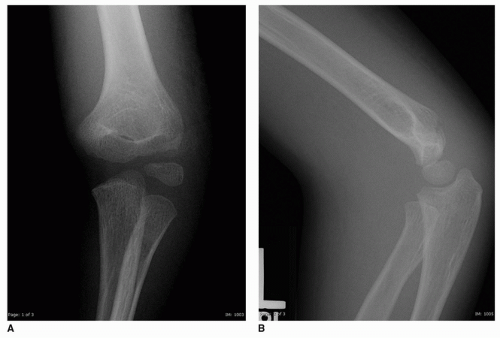
The need for surgery depends on the type of lateral condyle fracture and amount of displacement. The Los Angeles classification system predicts the need for treatment based on displacement of the fracture fragment (Fig. 2-1). The fracture is in an oblique plane, so internal rotation oblique x-rays often show the maximum amount of fracture displacement and should be ordered for all fractures that are not clearly displaced (Fig. 2-2A-C).
Fractures with less than 2 mm displacement generally can be treated by simple immobilization in an above-elbow cast for 4 to 6 weeks. X-rays should be obtained about 1 week after presentation to check for late fracture displacement. These may be done out of plaster and under fluoroscopy to best assess maximal displacement. If the fracture displacement worsens over time to greater than 2 mm, surgical treatment should be considered.
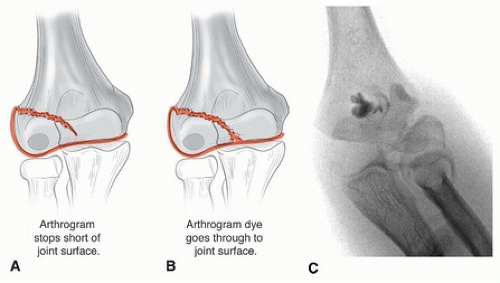
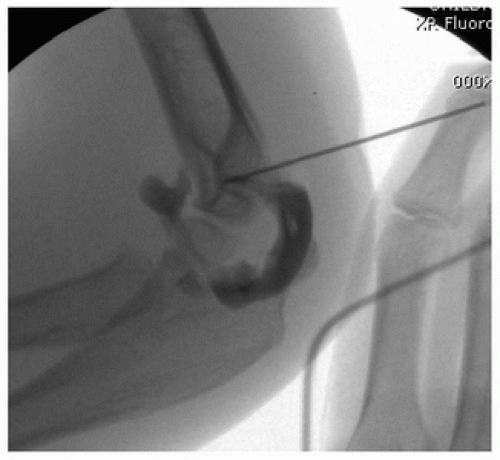
Fractures with 2 to 4 mm of displacement can be generally treated with closed pinning. These are most often hinged-type fractures with an intact cartilaginous joint surface. The presence of the hinge can be proven radiographically by magnetic resonance imaging (MRI), which is rarely indicated, or with arthrography (Fig. 2-3), which may be done intraoperatively just prior to pinning to confirm an intact joint surface. The fracture can be pinned percutaneously, with or without attempting to reduce the fracture by direct pressure over the lateral condyle. If there is any question about the reduction or stability, the fracture should be treated with open reduction and internal fixation. Fractures with over 4 mm of displacement require reduction and internal fixation to restore alignment of the growth plate and the articular surface.
Contraindications
In the past, it has been felt that surgery should be avoided in patients who present very late, although good results are possible by avoiding disruption of the posterior blood supply to the capitellum, use of rigid fixation with a screw, and relatively early motion.
Surgical Procedure
Some special operating room equipment is necessary. It is useful to have a radiolucent table or arm board to allow easy fluoroscopic access to the distal humerus. Fluoroscopy is required, and the monitor should be placed in a position easily visible to the surgeon to avoid having to turn away from the operative field to visualize images. A headlight is useful to visualize the joint surface. A tourniquet provides a bloodless field. A power drill is required to drill or place pins. A reduction clamp such as one resembling a towel clip is often useful. Fixation pins or screws will be required. After surgery, a splint or cast will be required. Preoperative prophylactic antibiotics are used. Muscle relaxation is not generally required.
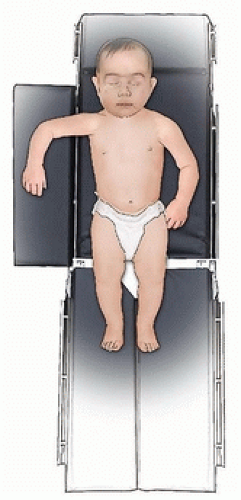
For surgery, the patient should be positioned supine on the operating table (Fig. 2-4). It is wise to ask the anesthesiologist to tape the endotracheal tube away from the side of the fracture. The arm should be abducted 90 degrees away from the trunk and internally rotated, giving clear access to the lateral condyle of the humerus. The surgeon should be aware that this position puts tension on the fracture fragment by the attached extensor muscles.
If the fracture is not completely displaced, an intraoperative arthrogram can help define if the joint surface is intact (Fig. 2-5). If it is intact (Fig. 2-3C), the fracture can be treated closed. The surgeon can try to reduce the metaphyseal fracture gap by direct pressure then and pin the fracture with K-wires. Screw fixation over a guidewire can be performed and is described in the following paragraphs.
 FIGURE 2-2 (Continued) C. Internal oblique view showing greater than 4 mm of displacement which requires ORIF. (Reproduced with permission of Children’s Orthopaedic Center, Los Angeles, CA.) |
 Get Clinical Tree app for offline access 
|