Kyphectomy in Spina Bifida
Richard E. McCarthy
DEFINITION
Kyphosis in the patient with myelomeningocele can occur at the thoracolumbar junction, the midlumbar spine, or the lumbosacral junction.
The different types of kyphosis have some bearing on the treatment needed for the repair, but whether the origin is congenital, developmental, or paralytic, the consequences can be devastating for the child with this condition.
Skin breakdown over the apex of the kyphosis can cause deep wound infections and lead to central nervous system infections.
Secondary changes in other organ systems can create compromise in the gastrointestinal or genitourinary systems or even potentially disastrous kinking of the great vessels due to compromise in the abdominal height. Diminished absorption frequently occurs in the gastrointestinal tract, and renal calculi may develop from poor urinary drainage.
Secondary effects on the pulmonary capacity produce thoracic insufficiency syndrome because the abdominal contents are pushed into the thoracic cage. Further worsening the respiratory compromise is a thoracic lordosis cephalad to the kyphosis.
Bracing generally leads to problems from skin pressure and ultimately does not solve the problem.
ANATOMY
The kyphotic angle can be a gradual slope or an acute gibbus.
The paraspinal musculature is segmentally innervated, thus partially active in a flexion position lateral to the bony ridges owing to lack of posterior migration from an embryologic origin. In this position, they contribute to forward flexion of the spinal column.
The bony ridges laterally in the area of the diastasis leave meager bone for fusion mass on the posterior side of the vertebral column.
The midline defect from the original myelomeningocele characteristically is covered by a fragile dura separated from the overlying skin by a thin layer of subcutaneous tissue.
The soft tissue coverage is made worse by poorly vascularized scarred skin.
One of the most reliably formed vertebral structures is the sacral ala.
The great vessels generally do not follow the kyphotic contours into the kyphotic apex.
PATHOGENESIS
Embryologically, the notochord is covered dorsally by closure of the ectoderm, progressing in a cephalad to caudal direction. In myelomeningocele, the closure is incomplete, usually at the caudal end.
Less common types of myelomeningocele occur in the thoracic and cervical area. Thoracolumbar, lumbar, and lumbosacral kyphosis is the most commonly seen type and occurs because of lack of posterior migration of the ectoderm surrounding the notochord, leaving the neural placode in a vulnerable position resulting in an exposed myelomeningocele sac at birth.
Congenital bony defects occurring in this area lead to an early-onset kyphosis that can pose significant problems for the neurosurgeon’s closure at birth. This has led some experts to encourage neonatal correction of the kyphosis.
With further growth and an upright sitting posture, the paraspinal musculature, which has formed in a lateral and anterior position, pulls the upper torso into a more kyphotic position, both actively through muscle contracture and secondarily from gravity.
This can lead to further skin compromise and pressure in the soft tissues overlying the kyphosis.
Skin breakdown can be a serious problem over the apex of the kyphosis.
The C7 lateral plumb line shows the upper torso to be far out of balance in a forward-flexed posture, leading to thoracic insufficiency from the abdominal contents pressing under the diaphragm.
This can render the child a “functional quadriplegic” because he or she uses the upper extremities for balance and to unweight the diaphragm by pivoting on the extended arms for breathing purposes (marionette maneuver; FIG 1).
From a developmental standpoint, this can further limit the young child’s upper extremity interaction with his or her environment, which is essential for the development of normal intelligence.
NATURAL HISTORY
The natural history of unpublished cases of severe kyphosis is one of respiratory compromise from thoracic insufficiency syndrome, progressive decline in pulmonary capacity, and death.
PATIENT HISTORY AND PHYSICAL FINDINGS
A careful history and physical examination should elicit possible signs and symptoms of associated anomalies, including the following:
Chiari malformation
Tethered cord
Respiratory compromise
Gastrointestinal malabsorption
Urinary hydrostasis and lithiasis
Physical examination of the child should include flexibility tests of the curve by physically supporting the child under the armpits to suspend him or her against gravity. Bending back supine on the examining table can also indicate the extent of lumbar flexibility.
IMAGING AND OTHER DIAGNOSTIC STUDIES
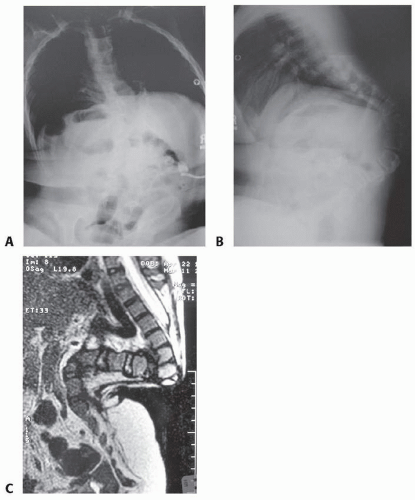
Standard radiographs, anteroposterior (AP) and lateral views of the full spine, in the upright sitting posture assess the effects of gravity on the curve (FIG 2A,B).
Supine radiographs are helpful for visualization of bony definition.
Flexibility films with traction, manual push, or back bending over a bolster with a shoot-through lateral film are helpful adjuncts.
Computed tomography (CT) scans, especially three-dimensional CT scans, offer the best delineation of the anatomy.
Magnetic resonance imaging (MRI) is critical for assessment of the intrathecal structures and assessing for Chiari malformation, syringomyelias, and tethering (FIG 2C).
DIFFERENTIAL DIAGNOSIS
Congenital versus developmental kyphosis
Sacral agenesis
Charcot joints secondary to vertebral column breakdown across the apex of the kyphosis
NONOPERATIVE MANAGEMENT
Bracing has no place in the treatment of this disorder.
Occasionally, traction is helpful to stretch the kyphosis, especially in a developmental type, to aid in correction at the time of surgery.
This can be done with cervical traction or halo traction, and some authors have promoted the use of this traction during surgery to aid in the correction.
SURGICAL MANAGEMENT
Preoperative Planning
Vascular monitoring devices are an important adjunct during surgery, and either arterial lines or pulse oximeters on both feet are important to monitor blood supply to the lower extremities at the time of correction.
A great deal of tension can come to bear on the aorta at the time of kyphosis realignment. Thus, arterial and central venous lines are necessary to monitor central pressure and allow for rapid administration of medication and fluids.
Areas of skin breakdown should be addressed prior to kyphectomy.
Preoperative planning may include consultation with a plastic surgeon and possible placement of tissue expanders in the posterolateral axillary margins to aid in skin closure at surgery (FIG 3).
As a part of the preoperative planning, all imaging studies are carefully reviewed to assess flexibility, the adequacy of the vertebral bodies to tolerate pedicle screws, and planning for which levels will need to be decancellized or removed.
It is recommended that these plans be recorded on a “blueprint” that can be placed on the operating room wall outlining the location of implants, osteotomies, and order of progression for the surgical plan.
Assessment by neurosurgery is necessary preoperatively regarding shunt functioning and review of the MRIs.
Preoperative antibiotics are essential, including gram-negative coverage for urinary pathogens. These are continued postoperatively for 6 to 12 weeks.
Nutritional status is maximized and may require hyperalimentation via a gastrostomy tube button months ahead of surgery to maximize postoperative healing.
 FIG 3 • Myelomeningocele in an 11-month-old child with tissue expanders placed bilaterally before delayed closure and kyphectomy.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|