Intramedullary Nailing of Metaphyseal Proximal and Distal Fractures
Robert Ostrum
Michael Quackenbush
DEFINITION
A fracture of the proximal or distal tibial metaphysis can occur from a variety of high- and low-energy trauma.
Fractures may be confined to the metaphysis or extend into the articular surface.
Simple fractures suggest lower energy injuries, whereas comminution signifies a greater amount of energy and a higher velocity mechanism.
ANATOMY
PATHOGENESIS
Common causes of tibial fractures include high-energy collisions (pedestrian vs. car bumper) such as an automobile or motorcycle crash.

FIG 1 • A. AP view of synthetic tibia model. Shading of the proximal tibial metaphysis is shown. B. AP view of synthetic tibia model. Shading of the distal tibial metaphysis is shown.
Lower energy injuries, such as certain sports injuries or falls, can also cause fractures of both the proximal or distal tibial metaphysis.
NATURAL HISTORY
Fractures of the tibia can occur in all age groups and from a variety of mechanisms.
Goals of treatment should include restoration of length, rotation, and alignment of the tibia with a return to previous level of activity and function.
Recognition and treatment of associated injuries including those to nerves, blood vessels, or compartment syndrome should be an integral part of the assessment and treatment to prevent complications.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients will often present with a recent history of trauma.
Tibial fractures may present with a variety of findings:
Pain in the affected extremity with an inability to bear weight
Leg length inequality
Visual deformity including tenting of the skin
Contusions/abrasions
Nerve injury
Open fractures
Compartment syndrome
Sensory deficits in the foot (less common)
IMAGING AND OTHER DIAGNOSTIC STUDIES
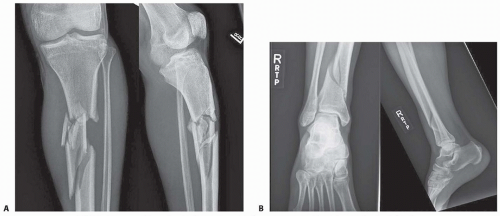
Diagnosis of a proximal or distal tibia (FIG 2A,B) fracture can usually be made with standard orthogonal anteroposterior (AP) and lateral x-rays.
Dedicated knee and ankle x-rays are necessary to decrease the chance of missing a fracture at the articular surface.
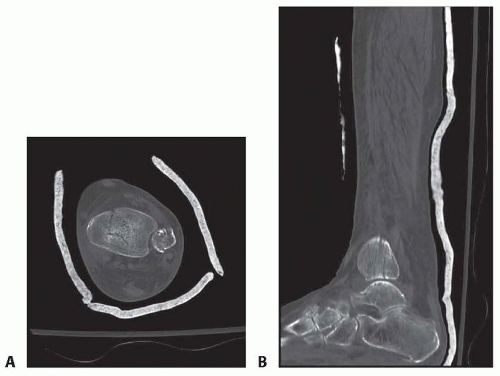
Fractures that extend proximally or distally into the articular surface may require a computed tomography (CT) scan to evaluate joint involvement and/or displacement to aid in preoperative planning (FIG 3A,B).
NONOPERATIVE MANAGEMENT
Nonoperative management is normally reserved for lower energy injuries with minimal or no displacement.
Patients with low functional demands (ie, paraplegic) or significant medical comorbidities can be successfully treated without surgical intervention.
Nonoperative management of the proximal or distal tibia often involves a long-leg splint with conversion to a long-leg cast once swelling has resolved.
Distal fractures may be converted to a short-leg cast or brace once there is radiographic evidence of healing.
Non-weight bearing for the first 6 weeks with progression to full weight bearing, with or without a brace, once there is physical evidence of healing (decrease in pain) and/or radiographic evidence of healing (callus formation)
SURGICAL MANAGEMENT
Proximal Tibia Fractures
The proximal tibia presents a challenge for intramedullary (IM) nailing due to deforming forces from the patella and the eccentric starting point for the IM nail.
Flexion of the knee past 60 degrees to allow access to the tibial nail starting point causes the quadriceps, patella, and patellar tendon to extend the proximal fracture fragment leading to an extreme procurvatum deformity.
In addition, starting the IM nail at the “usual” starting point, just medial to the lateral tibial spine, in the coronal plane will produce a valgus deformity. Techniques to prevent these deformities include the following:
Judicious use of blocking screws
Suprapatellar IM nailing
Semiextended IM nailing
Clamps, plates for reduction prior to IM nailing
Preoperative Planning
A review of all images will help to plan the surgical a pproach.
Fractures that extend into the proximal plateau or across the distal plafond may require closed or open reduction and fixation prior to IM nailing.
Cancellous screws (6.5 mm) placed posteriorly in the tibial plateau will be out of the way of the tibial nail and its entry site.
Depending on the fixation required, small fragment screws and/or plates should be readily available for distal fractures.
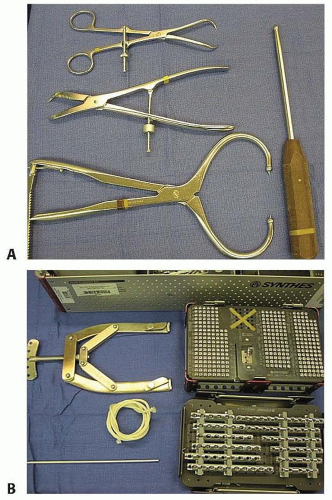
Obtaining and maintaining the reduction may require additional equipment. Planning ahead of time will avoid unnecessary delays in the operating room.
Some examples of other items you may wish to have available include (FIG 4A,B) the following:
Clamps, “spike” pushers, K-wires
Small fragment set (for provisional plate fixation)
Large fragment (6.5, 7.3 mm) cannulated cancellous screws
External fixator/universal distractor
Skeletal traction tray (calcaneal traction)
Positioning
Patients are positioned in the supine position on a radiolucent table. A bolster may be placed under the ipsilateral hip.
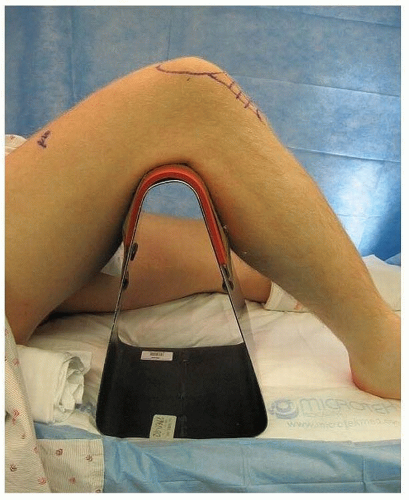 FIG 5 • Standard tibial nailing requires hyperflexion of the knee. Radiolucent triangles may help with positioning. |
Approach
Standard nailing uses an incision between the inferior pole of the patella and the tibial tubercle (FIG 7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree