CHAPTER 95 Intradiscal Steroids and Prolotherapy: Clinical Relevance, Outcomes and Efficacy
Internal disc disruption treatments are evolving. This chapter focuses on alternative intradiscal treatments distinct from the well-recognized ones (i.e. electrothermal annuloplasty, nucleoplasty, chemonucleolysis) discussed elsewhere in this book. In particular, this chapter focuses on intradiscal steroid injections and intradiscal prolotherapy. We discuss the rationale, efficacy, and potential therapeutic effects of these interventions based on a comprehensive literature review.
RATIONALE FOR INTRADISCAL STEROID INJECTIONS
Inflammatory processes theoretically contribute to discogenic pain. Nucleus pulposus material leaks along radial tears into or through the annular fibers causing a local inflammatory response with associated pain. Studies have shown the presence of both inflammatory mediators1 and inflammatory cells2–4 within herniated nuclear material. The high-intensity zone, often seen in symptomatic individuals, may represent inflamed grade 3 to 5 annular fissures with neovascularization.5–7
Corticosteroid administration has been used since the 1950s to treat symptomatic degenerative intervertebral discs. However, its efficacy and mechanism of action remained controversial. Feffer8 first described using intradiscal hydrocortisone injections for its antiinflammatory properties, attempting to reverse the degenerative process. He also suggested that it had a polymerizing effect and could thus heal annular tears and restore the disc’s biomechanical load-bearing properties. He proposed this hypothesis after observing that rheumatoid arthritis patients’ synovial fluid viscosity increased after intra-articular hydrocortisone injections. This was attributed to polymerization of the hyaluronic acid’s polysaccharide component. The synovial fluid’s depolymerized hyaluronic acid is replaced by fluid with normal viscosity within 4 days.9 Leao stated that in degenerative processes, the interfibrillar substance’s mucopolysaccharide can have an abnormal sulfuric chondroitin cleavage. The polymerization caused by hydrocortisone could repair the connection.10 Based on findings of accelerated disc degeneration following intradiscal Depo-Medrol administration, some11 have proposed that this agent may exert its therapeutic effect by reduction of disc bulging or protrusion.
INTRADISCAL STEROID INJECTION TECHNIQUE
The intradiscal steroid injection’s disc access and technique is essentially the same as that used for provocation discography.12–15 When indicated, the steroids are administered into the symptomatic level immediately after positive diagnostic disc stimulation using the same spinal needles. However, the discography’s contrast volume and the disc’s capacity may limit this technique. Intranuclear injection should distribute medication into contiguous radial fissures and annular tears.
INTRADISCAL STEROID INJECTION EFFICACY
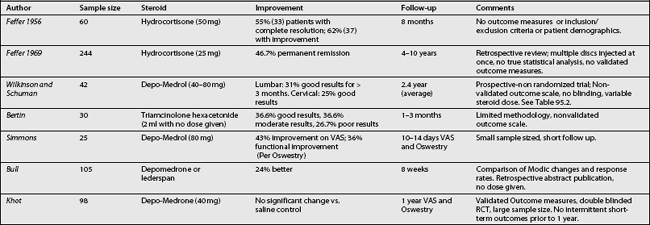
Table 95.1 summarizes this section’s studies. In 1956, Feffer described using intradiscal steroids for low back and sciatic pain.16 He injected a hydrocortisone and iodopyracet solution during a single-level discography procedure using a modified Erlacher technique. The injected solution included 3 cc of 35% iodopyracet and 1 cc of 50 mg hydrocortisone. The total injectate volume varied with the patient’s intradiscal capacity The two lowest lumbar discs were routinely injected with a few days between injections. Occasionally, he injected more cephalad levels, depending on the patient’s clinical scenario. If the first injection provided adequate relief, another level was not injected.
In 1969, Feffer published a retrospective review in which he evaluated 244 patients who had undergone therapeutic intradiscal hydrocortisone injection.8 Discography was performed using a posterolateral approach with an injectate composed of 25 mg hydrocortisone per 1.5 cc contrast dye. Initially, the contrast agent Diodrast was used but was subsequently replaced with Hypaque due to the ‘better contrast’ obtained on radiographic imaging. Feffer stated that, ‘In most cases, two interspaces were injected, although a conscientious effort was made to correlate the levels treated with the clinical picture.’ At an average follow-up of 7.3 years (range 4–10 years), 46.7% had ‘permanent remission’ while 53.3 % had response failure defined as either no initial response to injection or relapse of symptoms. They reported complications on both their study population as well as all other discograms performed in their center over the previous 4 years. These included postprocedural spinal headaches, one case of disc infection requiring interbody fusion and a missed intrathecal meningioma which was previously misdiagnosed for lack of a prediscography myelogram. Radiographs obtained routinely 2 years after discography did not reveal accelerated disc degeneration.
Older patients or those with primarily back symptoms responded better to intradiscal steroids while gender and neurologic deficit did not affect results. Disc characteristics in patients with positive results were analyzed. Patients with ‘posterior degeneration only’ also had more favorable responses. This was defined by discographic results demonstrating an intact anulus anteriorly and laterally, without hypertrophic or bony changes. The degree or direction of the disc protrusion did not affect prognosis.
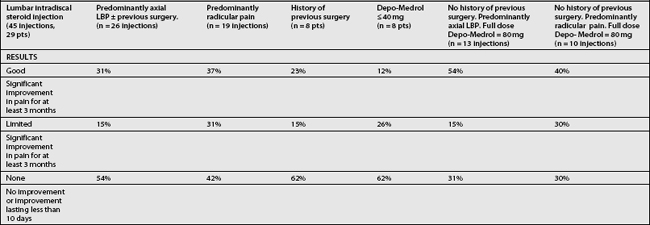
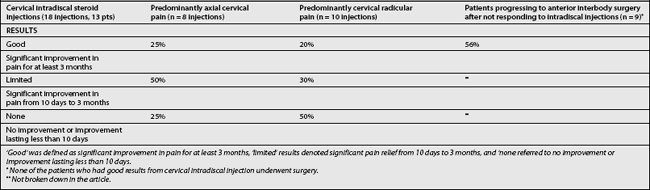
In 1980, Wilkinson and Schuman15 performed a prospective, nonrandomized intradiscal Depo-Medrol study investigating degeneratively mediated lumbar and cervical axial pain. Inclusion criteria required greater than 6 months’ symptom duration despite aggressive noninvasive therapy which was not defined. No patient was considered an ideal surgical candidate since they lacked any neurologic deficits. The study included 29 lumbar and 13 cervical patients. Myelography was reportedly normal in almost all patients except for degenerative changes. ‘Contrast and/or anesthesia discography’ was performed prior to the initial therapeutic intradiscal injection. Nearly all patients had pathology, most having a single-level abnormal disc. The study protocol changed after the first eight lumbar injections: Depo-Medrol increased from 30–40 mg to a dose of 60–80 mg into one or two discs. Each subject in the cervical group received 40–80 mg of Depo-Medrol. Average follow-up was 2.4 years with a 1-year minimum. This assessment was either a clinical examination or simply a referring orthopedist report. Outcomes were documented using a three-point Likert scale. ‘Good’ was defined as significant pain improvement for at least 3 months, ‘limited’ results denoted significant pain relief from 10 days to 3 months, and ‘none’ referred to no improvement or improvement lasting less than 10 days (Tables 95.2 and 95.3)
For the 45 intradiscal injections in the 29 patients with lumbar disc disease, including those with previous lumbar surgery, and mainly axial low back pain with little or no lower limb radicular pain, 31% had good results lasting more than 3 months, 15% had limited relief, and 54% responded poorly (see Table 95.2). In patients with predominantly radicular pain, 37% had good results, 31% had limited relief, while 42% responded poorly.
Eighteen injections in 13 patients with cervical disc disease were also studied (see Table 95.3). None had previous cervical surgery and all received 60–80 mg of Depo-Medrol (80 mg/mL). For those with mainly axial neck pain, 25% had good results, 50% had limited relief, and 25% did poorly. For those with predominantly cervical radicular symptoms, 20% had good results, 30% had limited relief, and 50% did poorly. Nine cervical patients subsequently underwent anterior interbody surgery with 5 (56%) having good results from surgery. None of the patients who had good results from cervical intradiscal injection underwent surgery. The only complications reported were occasional spinal headaches and minor menstrual irregularity. No disc infections or increased disc degeneration were encountered.
In 1990, Bertin et al.17 studied the effect of triamcinolone hexacetonide for acute, subacute, and chronic sciatica with a prospective, nonrandomized study. Each patient had sciatica with evidence of ‘disc protrusion,’ ‘discal hernia,’ or ‘epidural fibrosis’ by CT scan or ‘saccoradiculography’ (myelography). Operational definitions for disc protrusion, discal hernia, and sciatica were not given. The presenting sciatica symptoms were resistant to conservative care including rest, nonsteroidal antiinflammatory drugs, and, occasionally, epidural steroid injections. Each patient underwent discography followed by intradiscal injection of local anesthetic combined with 2 mL of triamcinolone hexacetonide. The exact dosage was not given. Follow-up occurred at 1 and 3 months following injection. There were 30 patients who had a mean age of 46 years (range 25–63 years) and mean duration of symptoms of 36 months (range 1 month to 10 years). Outcomes were categorized according to the authors’ idiosyncratic criteria. Good results were defined as return to work or normal activity, discontinuation of analgesics and/or antiinflammatory drugs, and absence of clinical signs of radiculopathy. Moderate results were defined as commencement of restricted occupational or recreational activity, ‘improvement but insufficient’ reduction of axial or appendicular pain, and continued use of antiinflammatories or analgesics. Poor results yielded no change in pain and no return to work.
The only two complications reported were one case of transient urinary retention and one case of foot dorsiflexion weakness that persisted at 1 year. Due to the small number of patients (n=30), Woolf’s G test was utilized. There was no significant difference between the results at 1 versus 3 months although there was a trend for diminished number of good results and an increase in poor results with the number of moderate results remaining relatively unchanged. After 3 months, 36.6% had good results, 36.6% had moderate results, and 26.7% had poor results. Essentially, one-third of patients had a good, moderate, or poor result. Duration of symptoms of less than 6 months and CT-scan appearance of disc herniation (p<0.001, g=11.65) or fibrosis (p<0.001, g=11.65) predicted a good prognosis whereas a poor prognosis was more likely when there was an antecedent occupational accident (0.025< p <0.05, g=4.76), symptom duration of greater than 6 months (0.01< p < 0.025, g=8.644), and a CT-scan appearance of disc protrusion (p<0.001, g=11.65). The authors’ distinction between disc protrusion and discal hernia was not defined. Factors that did not affect results were gender (g=6.9×104), age (g=0.149), spinal stiffness (g=0.8), presence of Lasegue’s sign (g=2.197), disc level (g=1.92), history of disc surgery (g=0.346), and zygapophyseal joint arthropathy (g=2.7). The authors suggested limiting the indication for intradiscal steroid injection to sciatica due to a disc protrusion when the symptoms were of less than 6 months duration. They also suggested symptomatic epidural fibrosis could constitute an indication, but were less demonstrative about this. The authors did not specify any criteria for diagnosing symptomatic epidural fibrosis. The methodology was limited, since it was nonrandomized and nonblinded, analyzed a small sample size, and used an outcome measure that had not been validated. Likewise, neither the discography technique nor the interpretation method was described. Finally, the operational definitions distinguishing ‘discal hernia’ and ‘disc protrusion’ were not described.
Simmons et al.14 evaluated the efficacy of intradiscal steroids (Depo-Medrol) in 25 patients, aged 18–50 years, who experienced low back pain due to single-level lumbar disc disease diagnosed using provocation discography. Other inclusion criteria included no prior surgery, 6 weeks of axial back pain that failed to improve with conservative care, and an MRI that did not reveal a sequestered fragment. Patients were then randomized to one of two study arms and prospectively assessed. The therapeutic group received an unreported volume of 80 mg/mL of Depo-Medrol and the control group was given 1.5 mL of 0.5% Marcaine. The Oswestry Pain Questionnaire, visual analogue scale (VAS) and pain diagram were evaluated. These were completed before and at 10–14 days following discography and intradiscal injection. The timing of intradiscal injection relative to discography was not specified but is implied to immediately follow the provocation discography. If no improvement was reported after 10–14 days, surgery was offered, when appropriate.
Bull retrospectively studied the efficacy of intradiscal depomedrone or lederspan administration during a discography procedure on degenerative lumbar discs in relation to Modic changes.18 Of 105 patients, 61 had no Modic changes, 20 had type I Modic changes, and 24 had type II Modic changes. At 8 weeks postinjection, patients were classified as better (complete resolution or significant improvement allowing return to normal activities), same, or worse. Worsening occurred temporarily in seven patients, four in the non-Modic group and three in the type I Modic group. No worsening occurred in the type II Modic group. In the non-Modic group, 8 (13%) were better and 49 (87%) were the same. In the Type I Modic group, 4 (20%) were better and 13 (80%) were the same. In the type II Modic group, 13 (54%) were better and 11 (46%) were the same. For statistical analysis with chi-square analysis with Yates correction, the seven patients with worsening were placed in the ‘same’ group. There was a significant difference between the type II Modic group and the non-Modic group (p<0.02). There was no significant difference between the type I Modic group and the non-Modic group (p>0.5). Based on these findings, the authors concluded that patients with MRI findings of type II Modic changes may have an inflammatory response and may, therefore, respond to intradiscal steroid injection. This study was limited in that it was published in abstract form only, did not include dosages of medications, and was retrospective.
Khot et al.19 also produced a randomized, controlled trial comparing intradiscal injection of 1 cc of 40 mg Depo-Medrol to 1 cc of normal saline in a total of 98 patients (120 enrolled, 98 completed) with chronic axial low back pain without radicular pain who had failed at least 6 weeks of conservative care. All patients had concordant pain generation of a degenerate disc on provocation discography and were given the intradiscal injection postdiscography. Sixty patients were randomized into each group. Of these, 46 in the Depo-Medrol group and 52 in the saline group completed the trial. The patients were prospectively followed in clinic and by postal questionnaire at 1 year with a visual analogue score for pain and an Oswestry Disability Index.
This study’s strengths were its use of validated outcome measures, larger sample size than previous studies and the fact that it was a double-blinded, randomized, controlled trial. Unfortunately, outcomes were only assessed at 1 year without regard to the intervening time periods such as 1–2 weeks, 4–6 weeks, 3 months, and 6 months. It is possible that the therapeutic time period was missed. Additionally, in 1980, the study by Wilkinson and Schuman15 suggested that 80 mg of Depo-Medrol provided better results than 40 mg of Depo-Medrol. Thus, Khot et al. may not have used an adequate dose of methylprednisolone acetate or Depo-Medrol. Additionally, the study conclusions may not be applicable to other corticosteroids.
There has been one coccygeal intradiscal steroid injection investigation evaluating coccydynia symptom relief.20 Radiographs were obtained in two positions: (1) the lateral standing position after standing 5–10 minutes, thus allowing the coccyx to regain a neutral position, and (2) a dynamic film taken laterally after 1 minute of sitting on a hard stool with the back slightly extended in a position where the patients experienced the most pain. Measurement changes in sagittal angulation and displacement in 91 patients with chronic coccydynia and 25 volunteers without low back or coccygeal pain were compared. Based on these comparisons, patients with coccydynia were classified into three categories based on the dynamic coccygeal motion or angulation amount: (1) normal, (2) hypermobile if there was more than 25° flexion, and (3) luxation if there was more than 25% slippage. In the control group, the mean mobility ranged from 0 to 70 degrees with a mean of 9.3±5.7 degrees. Only two control patients had less than 20% luxation. In the symptomatic group, 28.6% had luxation, 19.8 % were hypermobile, and 51.6% had normal coccygeal mobility.
In 86 patients, coccygeal discography was performed to inject prednisolone acetate into the involved articulation, which could exist as disc, synovial joint, or as intermediate structure. The researchers used Maigne’s previously described technique for coccygeal discography.21 The sacrococcygeal or intercoccygeal disc was entered from a midline posterior approach with the patient in a lateral decubitus position using an image intensifier. The dosage of steroid was not detailed. At a follow-up of approximately 2 months postprocedure, improvement was reported in 50% of the patients with luxation or hypermobility whereas only 27.5% of the symptomatic patients with normal coccygeal motion improved with a statistical difference between groups (p=0.033). Unfortunately, the outcome measurement method was not described.
In summary, intradiscal corticosteroid injection efficacy studies have methodologic flaws but demonstrate the technique is relatively safe and provides modest clinical discogenic pain improvement for selected patients. Older patients with predominantly axial pain have better outcomes8,15 and the response appears dose-dependent. All investigations used only one agent and therefore the results may not be applicable to other corticosteroids. Each injectate may have unique characteristics such as solubility, duration of action, and extent of accelerated disc degeneration. The supposed inactive ingredients contained in the corticosteroid preparation may also need to be considered.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree