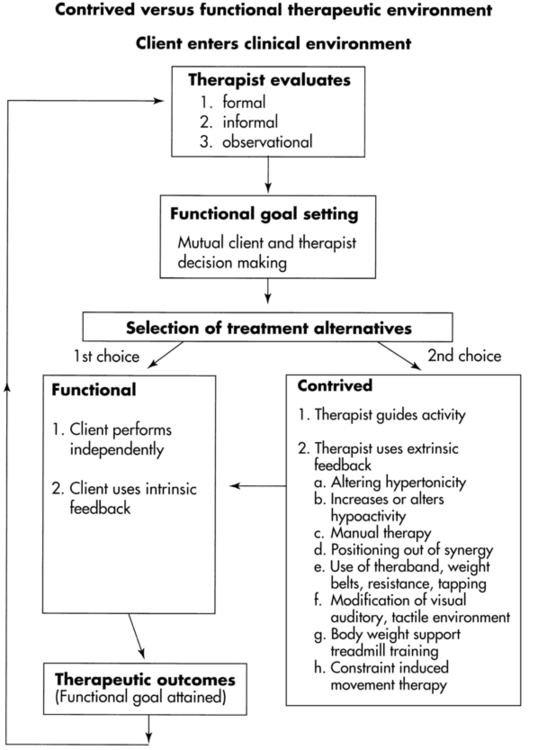
DARCY A. UMPHRED, PT, PhD, FAPTA, NANCY N. BYL, PT, MPH, PhD, FAPTA, ROLANDO T. LAZARO, PT, PhD, DPT, GCS and MARGARET L. ROLLER, PT, MS, DPT After reading this chapter the student or therapist will be able to: 1. Appreciate the complexity of motor responses, and discuss methods used to influence body systems and their effects on functional behaviors. 2. Outline the differences in recovery related to healing, compensation, substitution, habituation, and adaptation. 3. Analyze the similarities and differences among impairment training of specific body systems, functional training, augmented feedback training, and learning-based sensorimotor retraining. 4. Select appropriate intervention strategies to optimize desired outcomes. 5. Analyze variables that may both positively and negatively affect complex motor responses and a patient’s ability to participate in functional activities. 6. Identify procedures and sequences required to attain the most successful therapeutic outcome that best meets the needs and goals of the client and the family. 7. Consider the contribution of the client, the client’s support systems, research evidence, neurophysiology, and the best practice standards available to optimize outcomes. Before discussing therapeutic intervention procedures, the therapist must identify the learning environment within which the client will perform. As discussed in Chapter 1, that environment is made up of the therapist and the client, all internal body control mechanisms of the client, and the external restraints and demands of the world. Although this text focuses on relearning functional movement, the reader must always consider all aspects of the client including how other organs or body systems will be affected by or will affect the therapeutic outcome both during rehabilitation and in relation to long-term quality of life. An examination and evaluation (see Chapter 8) are performed before intervention to establish movement diagnoses. These examinations lead to movement diagnoses that must link to functional limitations or restrictions in activities and their causations (body system problems). Movement diagnoses and the degree and extent of the system or subsystem dysfunction or impairments determine prognosis of the outcomes on the basis of the client’s potential for functional improvement. Factors such as motivation, family support, financial support, and cultural biases must be considered as part of the prognosis.1 This process guides the selection of intervention strategies. Although it could be assumed that some of these impairments would be directly correlated to the central nervous system (CNS) trauma experienced by the client, it must also be determined whether some or most of these impairments have developed over a lifetime as a result of small traumas and adjustments to life. This insidious cause of impairments needs to be differentiated from acute causation of activity limitations because goal setting and expectations related to prognosis and recovery can be different. Both the American Occupational Therapy Association (AOTA) and the American Physical Therapy Association (APTA) have developed guides to practice that help to direct therapists entering the professions and should help to guide practice throughout their working lives.2,3 APTA, through the initiation of the California Physical Therapy Association, has been collecting and classifying evidence-based articles through the Hooked on Evidence project.4 Through the use of current evidence-based practice; sensorimotor processing, motor control, motor learning, and neuroplasticity theories (see Chapter 4); and body systems models, the therapist must determine the flexibility or inherent motor control the client demonstrates while executing functional activities and participating in life. This chapter or other chapters in the book cannot establish for the reader the exact treatment sequence that should be used for every patient, but an example of a decision-making pathway has been given in Box 9-1. Functional goals must be established that lead to the client’s ability to participate in life within his or her environment and whenever possible lead to or maintain the quality of life desired by the client. Similarly, the therapist must differentiate whether the observed motor problems are based on acute or longstanding impairments before establishing timelines for prognosis. Before beginning any intervention, the therapist must determine the treatment strategies that will be used to help the client attain the desired functional outcomes. The specific environment used by the therapist to optimize patient performance will depend on the functional level and amount of motor control exhibited by the patient. The following classifications can be used to document the specific role of the therapist within the training session (refer to Chapter 4 for additional detail): Functional training: Practice of a functional skill that is meaningful, goal directed, and task oriented. Patient will experience errors and self-correct as the program becomes more automatic and integrated. An example would be gait training on a tile surface, rugs, inclined surfaces, compliant surfaces such as grass, and so on to practice ambulation. Body system or impairment training: Treatment focus is on correcting a body system problem during an activity (e.g., pure muscle strengthening, stretching, sensory training, endurance training). Augmented feedback training: Patient needs external feedback (auditory, visual, kinesthetic) and control over the motor program running the target task. This will limit the response patterns (e.g., reducing degrees of freedom, reduction or enhancement of tone) for successful performance of the desired movement (e.g., handling techniques, body-supported treadmill training, constraint-induced training). Learning-based sensorimotor retraining: Treatment focus is placed on improving sensory discrimination dysfunction as a consequence of somatosensory, premotor, and motor cortical disorganization resulting from trauma, degeneration, or overuse. The reader must also remember that intervention encompasses multiple interactive environments where intervention decisions are often made moment by moment during any treatment period. The challenge to the educated clinical professional is to determine what is being done, why it is working, how to continue its effectiveness, and how to determine the progress of the successful intervention. The clinician must also determine how to empower the client (emotionally, cognitively, and motorically) to take over the intervention with inherent, automatic mechanisms that lead to fluid, flexible, functional outcomes independent of both the therapist and the environment within which the activity is occurring. It is not until clinicians can determine effective treatment outcomes from various interventions that efficacy within a research laboratory can be studied without speculation and hypothesis formation based on speculation.1 Effectiveness is the first way to determine evidence-based practice. Once effectiveness has been established through case studies and larger controlled studies within the clinical environment, researchers can begin to tease out separate variables and establish efficacy as part of evidence to justify clinical decision making. During the decade or two before the 1960s, some talented and intelligent clinicians began to question the traditional intervention strategies used by the OT and PT. These pioneers5–29 in neurological rehabilitation set the stage for the development of new concepts that allowed basic science to infiltrate the clinical arena. The intervention strategies of Jean Ayers, Berta Bobath, Signe Brunnstrom, Margaret Johnstone, Susanne Klein-Vogelbach, Margaret Knott, Dorothy Voss, Margaret Rood, and others became popular. Colleagues observed these master clinicians and could easily see that the “new” interventions were much more effective and provided better outcomes than previous interventions. Each approach focused on multisensory inputs introduced to the client in controlled and identified sequences. These sequences were based on the inherent nature of synergistic patterns5,21,30,31 and motor patterns observed in humans5,7,32 and lower-order animals33 or a combination of the two.19,21 Each method focused on the individual client, the specific clinical problems, and the availability of alternative treatment approaches within an established framework. Some of these approaches focused on specific neurological medical diagnoses. The treatment emphasis was then on specific patients and their related movement disorders. Children with cerebral palsy and head injuries7,23,28 and adults with hemiplegia8,9,21,32 were the three most frequently identified medical diagnostic categories. In 1968 at Northwestern University a large conference was held and laid the foundation for the first STEP conference (Northwest University Special Therapeutic Exercise Project [NUSTEP]). Most of these master clinicians, along with research scientists of the day, came together to try to (1) identify the commonalities and differences between these approaches, and (2) integrate and use the neuroscience of the day to explain why these approaches worked.34 Since the 1970s, substantial clinical attention has also been paid to children with learning and language difficulties.5,13,35 Now these concepts and treatment procedures have been applied across the age spectrum for all types of medically diagnosed neurological problems seen in the clinical setting (refer to Section II of this text). This expansion of the use of any of the methods for any pathological condition manifested by insults from disease, injury, or degeneration of the brain seems to be a natural evolution given the structure and function of the CNS and commonalities in system problems and activity limitations that take the individual away from participating in life. Fortunately, most dogmatism no longer persists with respect to territorial boundaries identified by clinicians using some specific intervention methods. A conference in 199036 played a significant role in challenging the relevance of these territorial boundaries and stressed the adoption of a systems model when looking at impairments, activity limitations, and participation in life interactions.37 As the boundaries for interventions began blurring, intervention approaches such as proprioceptive neuromuscular facilitation (PNF) were then integrated into the care of clients with orthopedic problems and patients with neurological impairments. Today, few universities within the United States teach separate sections or units on specific approaches, but rather teach students to identify problems, when they are occurring in functional programs, and what bodily systems might be the cause of those activity limitations. For example, assume that a client with hemiplegia exhibited signs of a hypertonic upper-extremity pattern of shoulder adduction, internal rotation, elbow flexion, and forearm pronation with wrist and finger flexion. Brunnstrom8 would have identified that pattern as the stronger of her two upper-extremity synergies. Michels,21 although using an explanation similar to Brunnstrom’s to describe the pattern, would have elaborated and described additional upper-extremity synergy patterns. Bobath would have asserted that the client was stuck in a mass-movement pattern resulting from abnormal postural reflex activity.30 Although the conceptualization of the problem certainly determined treatment protocols, the pattern all three clinicians would have worked toward was shoulder abduction, external rotation, elbow extension, forearm supination, and wrist and finger extension. The rationale for the use of this pattern within an intervention period would vary according to the philosophical approach. One clinician might describe the pattern as a reflex-inhibiting position (Bobath).31 Another would describe the pattern as the weakest component of the various synergies (Brunnstrom),8 whereas still another might identify the pattern as producing an extreme stretch and rotational element that inhibited the spastic pattern (Rood).25 How those master clinicians sequenced treatment from the original hypertonic pattern to the opposite pattern and then to the goal-directed functional pattern would vary. Some would facilitate push-pull patterns in the supine and side-lying positions and rolling. Others would look at propping patterns in sitting clients or at weight-bearing patterns of clients in the prone position, over a ball or bolster, or in partial kneeling. All have the potential of improving the functional pattern of the upper extremity and modifying the hypertonic pattern. One method may have been better than the others given a particular patient, but in truth improved patient performance may have stemmed not from the method itself, but rather from the preferential CNS biases of the client and the variability of application skills among the clinicians themselves. That is, when a therapist intentionally uses specific augmented feedback to modulate the motor system’s response to an environment but does not identify the other external feedback present within that environment (e.g., lighting, sound, touch, environmental constraints), therapeutic results will vary. Because of variance, efficacy of intervention is often questionable, although the effectiveness of that therapist may be easily recognized. Because of the overlap of treatment methods and the infiltration of therapeutic management into all avenues of neurological dysfunction, various multisensory models were developed during the early 1980s.13,38–41 These have continued to evolve into acceptable methods in today’s clinical arena. Although these models attempted to integrate existing techniques, in reality they have created a new set of holistic treatment approaches. In July 2005 the III STEP conference42 was held in Utah to again bring current theories and evidence-based practice into today’s clinical environment. The history of the three STEP conferences demonstrates the evolution of evidence-based practice from the first conference, where basic science was the only evidence to justify treatment, to the second conference, where evidence in motor learning and motor control began to bring efficacy to intervention. By the time the third conference was held, the research in neuro/movement science regarding true efficacy within practice and the reliability and validity of our examination tools set the stage for standards in practice.43 Where the next conference will take the professions and how soon that will occur is up to colleagues in the future. No proceedings from that third conference were published, but over the preceding years articles covering most of the presentations had been published in the Journal of Physical Therapy. The ultimate goal would be to develop one all-encompassing methodology that allows the clinician the freedom to use any method that is appropriate for the needs and individual learning styles of the client as well as to tap the unique individual differences of the clinician. Although intervention today is based on an integrated model, the influence of third-party payers, the need for efficacy of practice, and time constraints often factor into the therapist’s choice of intervention. Visionary and entrepreneurial practice ideas that have the potential to be effective will always be a challenge to future therapists. Those ideas generally originate within the clinical environment and not the research laboratory. For that reason, clinicians need to communicate ideas to the researcher, and then those researchers can develop research studies that test the established efficacy or refute that effectiveness. Few researchers are master clinicians, and few clinicians are master researchers; thus collaboration is needed as the professions move forward in establishing evidence-based practice. Today’s therapists have replaced many of the existing philosophical approaches with patient-centered therapeutic intervention. Patient performance, available evidence, and the expertise of the clinician often play a key role in the specific decision regarding an intervention. When confronted with an abnormal upper-extremity pattern, today’s therapist may choose to work on improving the movement pattern using a functional activity. Control of the combination of movement responses and modulation over specific central pattern generators or learned behavior programs will allow the patient opportunities to experience functional movement that is task oriented and environmentally specific. With goal-directed practice of the functional activity, neuroplastic changes, motor learning, and carryover can be achieved.44 With a better scientific basis for understanding the function of the human nervous system, how the motor system learns and is controlled, and how other body systems, both internal and external to the CNS, modulate response patterns, today’s clinicians have many additional options for selection of intervention strategies.45–54 Whether a patient would initially benefit best from neuromuscular retraining, functional retraining, or a more traditional augmented or contrived treatment environment is up to the clinician and is based on the specific needs identified during the examination and evaluation process. A problem-oriented approach to the treatment of any impairment or activity limitation implies that flexibility and neural adaptation are key elements in recovery. However, adaptation should not be random, disjointed, or non–goal oriented. It should be based on methods that provide the best combination of available treatment alternatives to meet the specific needs of the individual. Development of a clinical knowledge bank enables the therapist to match treatment alternatives with the patient’s impairments, activity limitations, objectives for improved function, and desired quality of life. A professionally educated therapist no longer bases treatment on identified approaches, although specific aspects of those approaches may be treatment tools that will meet the client’s needs and assist him or her in regaining functional control of movement. Treatment is based on an interaction among basic science, applied science, the therapist’s skills, and the client’s desired outcomes.49–52,55,56 In most cases, multiple intervention strategies must be included, but the therapist needs to be able to identify why those selected treatments will lead to system improvement as well as documenting those findings using reliable standardized and acceptable clinical methods and terminology. These intervention strategies must be dynamic yet also understandable and repeatable. As new scientific theories are discovered, new information must be integrated to continue to modify treatment approaches. In Chapter 8 the steps involved in the examination process are explained in detail. The intricate relationship of body system problems, impairments, and functional limitations that decrease participation in the rehabilitation process are discussed. Functional training can be implemented once the clinician has identified the client’s activity limitations. The clinician must first answer the questions “What can the client do?” “What limitations does the client have when engaging in functional activities?” “Are there motor programs that are being used to substitute for normal motor function?” and “Can the therapist use functional training to improve body system problems within the context of the functional skill?” Once the therapist has an understanding of the reasons for any activity limitation and can alleviate substitution and compensation for the deficit, functional tasks should be identified and practiced. An intervention approach in the early 1990s that evolved as an offshoot of functional training was labeled clinical pathways. These pathways were established by health care institutions to improve consistency of management of patients who met specific medical diagnostic criteria. It has been proven that the implementation of these pathways reduces variability in clinical practice and improves patient outcomes.67 Health care practitioners also became aware that some individuals do not fall into these pathways and need to be treated according to the specific clinical problems that the patients were presenting. One important variable that has clearly been identified with respect to functional training is “task specificity.”47,68–76 Although it is important that a patient be independent in as many ADLs as possible, often the therapist, the patient, and the family need to prioritize which activities are most important to the quality of life of the patient. If walking into the mountains to do “birdwatching” is one important goal to the patient, then creating an environment that would closely resemble the environment of that activity is crucial. Similarly, practice within that environment is a key to successful carryover (see Chapter 4). If the patient wants to walk into the mountains and the family expects the patient to walk into his or her old job, a therapist must accept that motivation will drive behavior and task specificity will drive learning. Carryover into any other functional activity such as walking into the office building in order to go back to work may not be the motivating factor that will guide that individual’s desire to perform that motor task. Whether the patient ever goes back to work is not the variable that should be used as part of the motivational environment for task-specific gait training geared to walking in the mountains and is not a decision for which the therapist is responsible. Therapists need to allow the patient to tell them what will be the most important task and the specificity of that task to optimize motor learning and functional recovery. As mentioned in Chapter 8, the therapeutic examination results in the identification of activity limitations and possible body system and subsystem impairments that are causing the functional movement disorders. Impairment training is another intervention strategy that involves the correction of impairments with the expectation that improving these impairments will result in a corresponding improvement in function. For example, when a client has the inability to stand up without assistance (activity limitation) and the clinician determines the cause to be lower-extremity weakness, an appropriate approach may be to strengthen the lower extremities (impairment training). Numerous studies have shown the effectiveness of impairment training in improving the functional performance of individuals with neurological conditions such as cerebral palsy,77,78 stroke,79–87 multiple sclerosis,88–93 Parkinson disease,94–98 and other neuromuscular diagnoses.99–110 The strengthening intervention selected should reflect the task and the environment within which the impairment was identified. The clinician should attempt to create a training situation so that the client may be able to run the necessary motor programs with all the required subsystems in place. For example, training sit to stand with weakness in the hip and knee extensors is much less likely to automatically result in the improvement of sit-to-stand function if the therapist begins the activity in sitting where generation of extension is most difficult, than if the strengthening training was performed with repetition of practice starting in standing and going to sit and back again to stand. By decreasing the degrees of freedom of the eccentric control of the hips and knees when going from stand to sit, the functional training activity has turned into specific impairment training. The therapist can ask the patient to eccentrically lengthen the extensors only in a limited range and then concentrically contract back to standing. As the power increases, the degrees of freedom can also be enlarged until the patient is able to complete the task of stand to sit while simultaneously regaining the sit to stand pattern. In pure impairment training a patient might also be asked to straighten the knee when sitting or to extend the hip when prone. These three exercises have the potential of training impaired strength, but only the first example forces the training within a functional pattern. Similarly, the therapist could train the sit-to-stand pattern using various seat heights that encompass many of the components that force the use of normal movement synergies and postural control, using the environment in which that activity is typically performed, versus performance of strengthening exercises against resistance in an open chain exercise program. These augmented techniques make up a large component of the therapist’s specific interventions tool box. The difference between augmented and functional training might be the need for the therapist or piece of equipment to be part of the client’s external environment for the client to succeed at the task. For example, in BWSTT a harness is used to take away the demand of gravity on the limbs during gait and the demand of the postural trunk and hip muscles for stability. Before the therapist or the patient can consider the movement as independent, those aspects must be removed from the environment. In the previous example, the individual needs to transition from maximal body weight support during ambulation to not needing any external support during ambulation. The client must assume total ownership of the functional responses. Then and only then has independence been achieved. At that time, functional retraining can be used with the intent of enlarging the environmental parameters to allow for maximal independence. Figure 9-1 illustrates this concept of functional versus contrived intervention, which must be constantly considered throughout any treatment session. Augmented techniques are often the early choices for treatment of patients who have neurological insults. It cannot be emphasized enough that once the client has the ability to perform without augmented methods and does so in functional, efficient ways, those augmented techniques need to be selectively eliminated.
Interventions for clients with movement limitations
History of development of interventions for neurological disabilities
Intervention strategies
Functional training
The effect of functional training on task performance and participation
Conclusion
Body system and impairment training
Augmented therapeutic intervention
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Interventions for clients with movement limitations
Only gold members can continue reading. Log In or Register to continue