Intertrochanteric Hip Fractures: Intramedullary Hip Screws
Michael R. Baumgaertner
Thomas Fishler
INTRODUCTION
The number of hip fractures in the United States is estimated to be approximately 400,000 per year and will increase 50% by the year 2025. These fractures typically occur in elderly osteoporotic females, with 90% of fractures occurring in patients older than 65 years of age (1). The cost burden exceeds 20 billion dollars annually, which does not include care beyond 1 year from injury. Approximately one in four hip fracture patients requires long-term placement in an assisted care environment, and nearly 50% of these patients do not regain preinjury levels of activity. The 1-year mortality following surgery for a hip fracture remains around 20%.
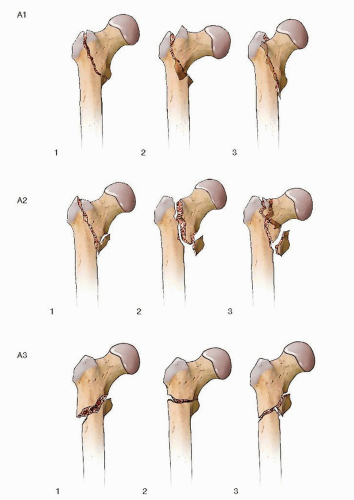
There are numerous classifications for hip fractures. All attempt to distinguish between stable and unstable fracture patterns. Unstable fracture patterns are marked by significant disruption of the posteromedial cortex, subtrochanteric extension, or reverse obliquity in the main fracture line. The AO/OTA classification of these fractures incorporates each of these features, classifying intertrochanteric fractures along a spectrum from most (31A1.1) to least (31A3.3) stable (Fig. 18.1).
Stable two-part and some three-part fractures, once reduced, will resist medial and compressive loads and can be treated with either a compression hip screw and side plate or an intramedullary nail. On the other hand, unstable three- and four-part intertrochanteric fractures invariably collapse into varus and shorten, and this is only partially prevented by a sliding hip screw. Even when healing is successfully achieved, limb shortening >2 cm and medialization of the shaft can lead to poor outcomes.
INDICATIONS AND CONTRAINDICATIONS
There are two broad categories of implants for the treatment of intertrochanteric hip fractures: a sliding hip screw and side plate and a cephalomedullary nail. A sliding hip screw and side plate remains the implant of first choice for stable two-part fractures, and multiple studies have shown no advantage with the use of an intramedullary device in this subgroup (2, 3, 4 and 5). Cephalomedullary nailing is indicated in unstable intertrochanteric hip fractures, particularly those with subtrochanteric extension and reverse oblique fracture patterns (AO/OTA 31A3). An additional indication for nailing is an impending or pathologic fracture of the proximal femur.
Contraindications to the use of a cephalomedullary nail include fractures of the femoral neck, deformities within the femoral shaft including preexisting implants, and hip ankylosis. A relative contraindication is the young trauma patient because of concerns regarding removing substantial bone from the trochanteric block in order to accommodate these large implants.
Cephalomedullary nails direct a screw(s) or a triflanged blade into the femoral neck and head through a variable length intramedullary nail. Implant insertion can be performed in a closed, percutaneous manner, minimizing surgical trauma at the fracture site, and reducing intraoperative blood loss. The device functions as an intramedullary buttress, maintaining length and alignment while restoring the mechanical support of the posteromedial cortex, preventing shaft medialization.
PREOPERATIVE PLANNING
History and Physical Examination
Elderly patients typically present after a mechanical ground level fall and are unable to stand or walk. It is important to obtain a thorough medical and social history, which includes associated medical history and the patient’s ambulatory status. On physical examination, the affected extremity is usually shortened and
externally rotated. There is exquisite tenderness to palpation around the hip and proximal thigh, and any movement in the extremity is painful. It is important to assess and to document the neurovascular examination as well as to rule out any associated injuries. Consultation with an internal medicine specialist is recommended to optimize the patient for surgery. Dehydration and associated metabolic abnormalities are common and should be corrected preoperatively. Diabetic patients must have good perioperative glucose control. Patients on anticoagulation therapy require temporary normalization of their clotting parameters prior to surgery. Prophylaxis against venous thromboembolism should take into account the relative risks of pulmonary embolism and bleeding complications. The choice of pharmacologic agent remains contoversial, but mechanical prophylaxis is indicated for all patients. Antiplatelet agents are usually stopped preoperatively but restarted shortly after surgery (6).
externally rotated. There is exquisite tenderness to palpation around the hip and proximal thigh, and any movement in the extremity is painful. It is important to assess and to document the neurovascular examination as well as to rule out any associated injuries. Consultation with an internal medicine specialist is recommended to optimize the patient for surgery. Dehydration and associated metabolic abnormalities are common and should be corrected preoperatively. Diabetic patients must have good perioperative glucose control. Patients on anticoagulation therapy require temporary normalization of their clotting parameters prior to surgery. Prophylaxis against venous thromboembolism should take into account the relative risks of pulmonary embolism and bleeding complications. The choice of pharmacologic agent remains contoversial, but mechanical prophylaxis is indicated for all patients. Antiplatelet agents are usually stopped preoperatively but restarted shortly after surgery (6).
Imaging Studies
The diagnosis of an intertrochanteric hip fracture is generally confirmed with standard anteroposterior (AP) and cross-table lateral radiographs of the hip. Additional x-rays, including an AP pelvis, centered over the pubic symphysis and full-length radiographs of the entire femur, should be obtained because deformities in the shaft may preclude the use of an intramedullary device. Internal rotation and traction radiographs are invaluable for understanding the fracture anatomy as well as the success of the anticipated closed reduction. Occasionally, x-rays of the unaffected hip and femur are useful for preoperative planning. Computed tomography is not usually necessary but is obtained in complex fractures on a case-by-case basis.
Timing of Surgery
In all cases, medical optimization should be expeditious, as mortality is increased when surgery is delayed beyond 48 to 72 hours from admission (7). Surgery is ideally performed during daylight hours with a rested team, 7 days a week. On the other hand, optimization efforts can and should be performed through the nighttime hours; as a result, we most commonly perform the procedure on the day following hospital admission. Occasionally, this timetable is altered by the need to correct coagulopathy or perform more involved preoperative medical studies.
Surgical Tactic
Careful examination of the preoperative radiographs as well as x-rays of the unaffected hip are important parts of the preoperative plan and help guide implant selection with respect to the neck-shaft angle, diameter, and screw length. The nail-screw angle of the device should match the neck-shaft angle of the desired reduction. The most common configuration is a 135-degree neck angle with a 95-mm lag screw. It is important to note that the nail is not designed to fill the canal. Although first-generation short-stem implants were associated with an unacceptably high rate of subsequent femoral fracture, a recent meta-analysis showed no increased relative risk for this complication when intramedullary devices were compared to side plates (8). We use a full-length intramedullary nail in pathologic fractures and in patients with subtrochanteric extension. For the majority of patients, we use a short nail that facilitates distal locking through a nail mounted jig. Other authors advocate the use a full-length implant to protect the entire femur for all cases.
Surgical Technique
Surgery is performed under a general or spinal anesthetic. While general anesthesia allows for complete muscle relaxation, it carries a higher risk of perioperative morbidity and mortality, particularly in the elderly hip fracture patient with multiple medical comorbidities. A decision on the method of anesthesia should be made in collaboration with the surgeon, anesthesiologist, and consulting internal medicine specialist. The preoperative prophylactic antibiotic of choice is a first-generation cephalosporin. In cases of penicillin allergy, a suitable alternative, typically vancomycin or clindamycin, is given.
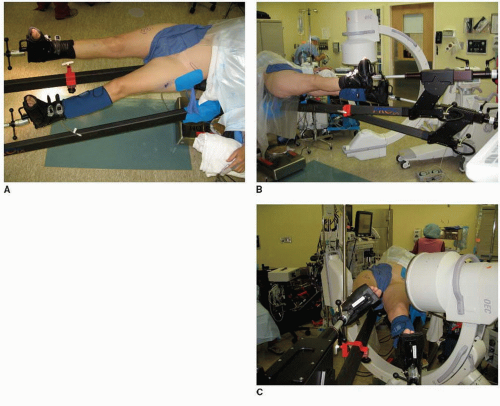
We prefer to use an orthopedic table that allows for balanced traction to be applied to both lower extremities, but a fracture table may be used as well. A well-padded post is placed in the perineum. Both lower extremities are secured to the table, and traction is applied. The operative side is adducted and slightly flexed at the hip and the unaffected leg abducted and extended to allow for lateral plane fluoroscopic imaging (Fig. 18.2B,C). “Scissoring” the extremities in such a way prevents the pelvis from rotating on the perineal post as traction is applied to the fractured limb, which can lead to a varus reduction (Fig. 18.3).
Once the patient has been securely positioned on the table, the fracture is reduced. There are two goals, the first of which is to gain access to the starting point in the proximal femur, the second being anatomic reduction of the fracture. Most stable fracture patterns will reduce with longitudinal traction and internal rotation of the limb. However, unstable intertrochanteric fractures may require different maneuvers, such as slight external rotation. A particularly troublesome deformity is subsidence of the proximal fragment into the intramedullary
canal of the distal fragment. The hallmark radiographic sign of a triangular double density, representing the overlap between the fragments, must be recognized, as this deformity is not reducible by manipulative means; here, a percutaneous intrafocal reduction aid as described by Carr is helpful (Fig. 18.4A-E) (9). Prior to prepping and draping the field, we confirm that we can see the following areas with fluoroscopy: the anterior cortex of the proximal femur, the fracture zone, the anterior neck, the entire circumference of the femoral head, the posterior neck, and the greater trochanter.
canal of the distal fragment. The hallmark radiographic sign of a triangular double density, representing the overlap between the fragments, must be recognized, as this deformity is not reducible by manipulative means; here, a percutaneous intrafocal reduction aid as described by Carr is helpful (Fig. 18.4A-E) (9). Prior to prepping and draping the field, we confirm that we can see the following areas with fluoroscopy: the anterior cortex of the proximal femur, the fracture zone, the anterior neck, the entire circumference of the femoral head, the posterior neck, and the greater trochanter.
In considering the reduction, we determine an acceptable neck-shaft angle to be 130 to 145 degrees. Increased valgus is permissible because it reduces the bending forces on the implant and may offset limb shortening that occurs with fragment impaction. Loss or gain of femoral anteversion >15 degrees, as seen on the lateral view, is unacceptable.
Once a provisional reduction has been achieved, the surgical field is prepped and draped in a standard sterile fashion. It is important to prep below the level of the knee in the event that a long nail is used that requires a distal interlocking screw. We use a sterile shower-curtain-type drape but add an extra sterile layer proximally to protect against puncture hole contamination from the instruments. If the closed reduction is inadequate, a number of percutaneous maneuvers may be attempted, utilizing such tools as the ball spike pusher, collinear clamp, and cerclage wire to improve the reduction (Fig. 18.5A-C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree