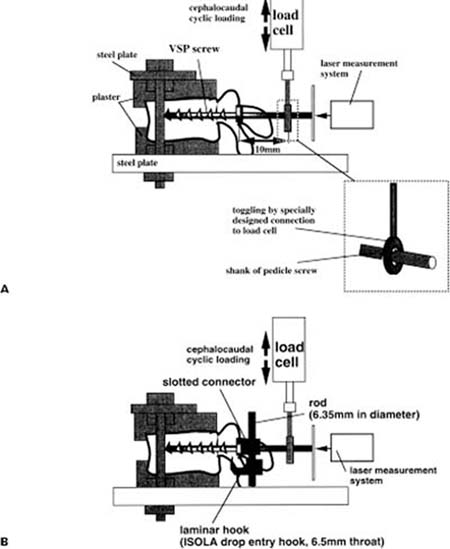
Chapter 9 As the life expectancy of the general population increases, there are increasing demands for the surgical treatment of various diseases in aged people. Tumor (primary as well as metastatic), trauma, infection, and degenerative disorders are common candidate diseases for spine surgery, and recent advances in the ability to support aged people by anesthesiologists and internists have decreased the risk of surgery. Spine surgery often requires fusion after decompression and/or correction of a deformity; therefore, some type of internal fixation is usually required. Although external immobilization, such as corset or brace, is an option, recent developments in internal fixation have greatly improved the outcome in correcting deformities, stabilizing the spine, maintaining alignment, and obtaining bony fusion. Internal fixation is also desirable for early mobilization without prolonged external immobilization, which is especially beneficial for decreasing complications in the elderly. Application of internal fixation, however, must be carefully considered in osteoporotic patients because of the higher rate of complications due to bone fragility.1 In this chapter, indications for internal fixation and recent advancements in spinal instrumentation (especially pedicle screwing and hook augmentation) are described. Fundamentally, the indication for internal fixation in osteoporotic conditions is not much different from that in cases of nonosteoporotic conditions. Although some investigators suggest that spinal instrumentation should not be used for severe osteoporotic conditions,2–4 it is mandatory in some cases with spinal instability. For example, a patient with reconstructive surgery of the vertebra after removal of spinal tumor is a definite candidate for the use of internal fixation. In many trauma cases, internal fixation is also essential for reduction and stabilization of the unstable and/or dislocated spine. Other than these conditions, the use of spinal instrumentation for degenerative disorders is rather controversial. Most degenerative disorders require decompression and/or fusion, but elderly people are usually less active and decompression alone without fusion might be sufficient for successful outcome. Among the several degenerative disorders, unstable degenerative kyphoscoliosis is an indication for the use of spinal instrumentation. Currently, there are several kinds of spinal instrumentation available. Anterior instrumentation consists of vertebral screws connected to rods or plates. Most of the posterior instrumentation methods are combinations of hooks, wires, and pedicle screws connected to rods or plates. The use of either anterior or posterior instrumentation should be based on the patient’s pathology. Although basic principles and techniques of spinal instrumentation in the osteoporotic spine do not differ much from those in the younger spine, surgeons should be more prudent to prevent complications. Recent advances in spinal instrumentation provide several augmentation methods, which might be useful to overcome the bone fragility in osteoporotic spine. There are roughly three types of augmentation methods to enhance the initial construct stiffness of spinal instrumentation. Several methods have been used to increase the implant-bone interface, especially with pedicle screws. The use of polymethylmethacrylate (PMMA) packed into the pedicle screw hole is the classic method to increase the screw pullout force. Zindrick et al5 reported that although unpressurized PMMA restored the pullout strength to within 5% of the original value, pressurized PMMA caused a twofold increase. A small amount of PMMA inserted in an unpressurized condition was reported to improve the pullout strength of a failed screw to approximately 1.5 times its original value.6 Soshi et al2 also investigated the effect of PMMA in pedicle screw pullout force and demonstrated that PMMA increases the pullout force in the moderate osteoporotic spine but failed to increase the pullout force in severe osteoporotic vertebra. Yamagata et al7 recommended the use of PMMA augmentation for pedicle screws in cases where the bone mineral density is less than 80 mg/cm2. Many ex vivo biomechanical studies support the use of PMMA in pedicle screw stability, but there are some potential adverse effects. Pressurization of PMMA into the pedicle screw hole can force the cement out of the pedicle, causing nerve root compression or irritation.8 PMMA evokes the formation of a membrane at the bone-cement interface, leading to bone resorption and resulting in loosening of the screw.9 Another concern is possible difficulty of screw removal or pedicle fracture during revision surgery. Although PMMA might enhance screw stability in severe osteoporotic spine, it should be used in an unpressurized manner, and surgeons should be aware of the possible complications regarding the use of PMMA. Recently, newly developed biocompatible and bioresorbable cements have been examined for potential use in increasing pedicle screw stability. Moore et al10 investigated the efficacy of calcium phosphate (Ca-P) cement for pedicle screw stability compared with PMMA in lumbar vertebrae of fresh human cadavers. They reported that both PMMA and Ca-P cement significantly increased pullout strength in revision screws by 147% and 102%, respectively. Most of the screws augmented with Ca-P cement were pulled out without causing any body fracture, whereas the pedicle fractured at or near its junction with the vertebral body in most of the screws augmented with PMMA. Lotz et al11 compared the pullout strength after cyclically loading with and without injectable biocompatible carbonated apatite cancellous bone cement (CBC). They reported a near doubling of the pullout strength with the use of CBC compared with controls. Yerby et al12 investigated the immediate effect of using hydroxyapatite cement (HAC) to augment revision pedicle screws after failure of the primary screw fixation. They demonstrated that the pullout strength of the 7 mm HAC-augmented screws was 325% of that of the 6 mm control screw, whereas the strength of the 7 mm nonaugmented screws was only 73% of that of the 6 mm control screws. Although these data suggest that the newly developed biocompatible and bioresorbable cements enhance immediate screw stability, there is little clinical data to support this method. Extending the fusion segment is the simplest way to increase the size of the anchor point. Gurr et al13 investigated the stability of spinal constructs with several types of instrumentation surgery after decompressive laminectomy. They reported that the flexion moment in the pedicle screw system with five levels was significantly superior (>1.5 times) compared with that in the same system with three levels. The long fusion, however, might result in greater exposure of the spine and a longer operative time, as well as the sacrifice of longer mobile segments. Ruland et al14 investigated the effects of a transverse plate (cross-link) connecting bilateral pedicle screws (Steffee VSP and CD). They concluded that even in osteoporotic spine CD and VSP screws with a transverse plate provided significantly greater fixation than the conventional pedicular or laminar hook-based systems. Dick et al15 also reported that the use of one cross-linkage increases torsional stiffness in a pedicle screw construct by 44% in a polyurethane spine model. Recently, several rod cross-linking systems were made available, and most were proven effective in clinical use. We have been trying to enhance initial stiffness of a spinal construct using a combination of the pedicle screw and laminar hook to the same vertebra in the osteoporotic spine. The pedicle screw-laminar “claw” is valuable and has been used clinically since 1990.16 Halvorson et al17 investigated the effects of using pedicle screws in conjunction with a laminar hook at one or two levels and evaluated the effect of bone mineral density on the quality of pedicle screw fixation. Although the results of their study were inconclusive because of the limited number of specimens used, the authors suggested that the use of pedicle screws in conjunction with a laminar hook at two levels improved pullout strength. Chiba et al18 investigated the effects of augmentation hooks applied from the supralaminar at T11 and infralaminar at L2 to standard short-segment pedicle instrumentation constructs in a L1 burst fracture model. The results clearly indicated that supplemental offset hooks significantly increased construct stiffness and absorbed some part of the construct strain. We conducted biomechanical testing to investigate whether adequate stiffness of short-segment instrumentation can be accomplished without invading the level adjacent to the instrumented vertebra in the osteoporotic spine. A laminar hook augmentation to the pedicle screw was used for this purpose. The effectiveness of a combination method of laminar hook and pedicle screw in comparison with that by pedicle screw alone in reference to bone mineral density of the vertebra under cephalocaudal cyclic loading were examined. Lumbar vertebrae were obtained from seven embalmed cadavers (average age ± SD = 73 ± 10.7, range 55 to 87 years). The embalming process affects the material properties of bone; however, all the vertebrae used in this experiment were fixed and preserved using the same procedure, and therefore the comparison made between the vertebrae was valid.19 Thirteen vertebrae, including one L1, two L2, seven L3, two L4, and one L5, with 26 pedicles, were available for this study. Bone mineral density (BMD) was measured using a dual-energy X-ray absorptiometer (DXA) in the anteroposterior direction. Both ends of a vertebra were placed in plaster to make the surfaces parallel. A pedicle screw was screwed into a vertebra. The vertebra was placed between two steel plates and fixed to an Instron-type testing machine. FIGURE 9–1
INTERNAL FIXATION OF
OSTEOPOROTIC SPINE
INDICATION FOR INTERNAL FIXATION
SPINAL INSTRUMENTATION AND THE AUGMENTATION METHOD FOR OSTEOPOROTIC SPINE
INCREASING THE STRENGTH OF THE IMPLANTBONE INTERFACE
INCREASING ANCHOR POINTS TO PREVENT STRESS CONCENTRATION
USE OF CROSS-LINKING TO INCREASE THE TORSIONAL STIFFNESS
COMBINATION METHOD OF PEDICLE SCREW AND LAMINAR HOOK
BASIC BIOMECHANICS
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree