Chapter 7 Internal Derangements
Ligaments and Tendons
Bursae
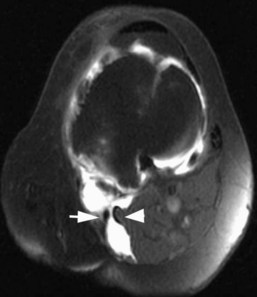
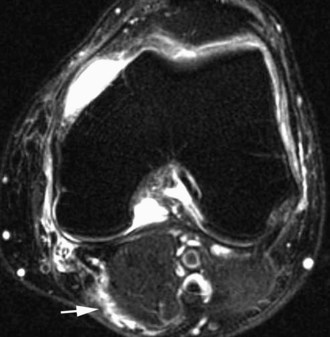
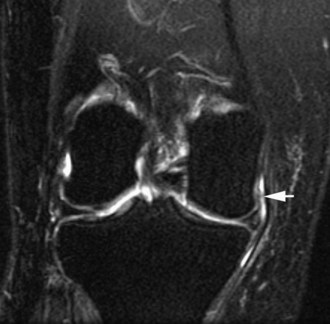
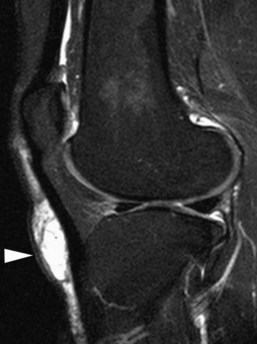
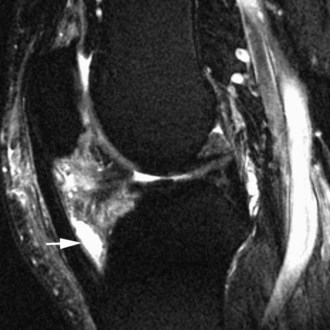
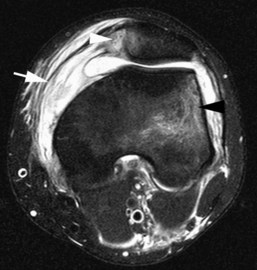
The medial gastrocnemius-semimembranosus bursa (Baker’s cyst) is commonly fluid-filled and is best demonstrated on an axial fluid-sensitive sequence, where it is seen as a comma-shaped structure between these two tendons (Fig. 7-1). It is the only knee bursa that consistently shows continuity with the joint space, and it has been associated with internal derangements such as meniscal tear, joint effusion, and degenerative joint disease. Rupture of a Baker’s cyst, a cause of acute knee pain and a mimic of deep venous thrombosis, is manifest by fluid signal tracking along the adjacent fascial planes, often into the midcalf (Fig. 7-2). Baker’s cysts can be a cause of refractory or recurrent posterior knee or calf pain, and they tend to recur after percutaneous aspiration. The semimembranosus–tibial collateral ligament bursa can be distinguished from a Baker’s cyst by its location medial to the semimembranosus tendon. The tibial collateral ligament bursa, or Voshell’s bursa, is located between its deep and superficial layers and can mimic medial meniscocapsular separation (Fig. 7-3).15 Pes anserinus bursitis manifests as fluid tracking along the pes anserinus tendons anteromedially at the knee joint line in an oblique plane (Fig. 7-4). The pes anserinus bursa is often contiguous with the tibial collateral bursa, and both can be contiguous with a Baker’s cyst. It is important to distinguish a primary bursitis in any of these locations from a parameniscal cyst, where fluid extends from a meniscal tear into one or more of these bursae.
Anteriorly, the prepatellar and infrapatellar bursae are best evaluated on sagittal sequences. Prepatellar bursitis, or housemaid’s knee, may be related to repetitive trauma such as kneeling (Fig. 7-5). As the name implies, it is located superficial to the mid extensor mechanism. Infrapatellar bursitis may involve the superficial or deep infrapatellar bursae. The superficial bursa is located between the skin and the tibial tuberosity and has been referred to as clergyman’s knee (Fig. 7-6). The deep infrapatellar bursa (Fig. 7-7), between the distal patellar tendon and the tibial tuberosity, may contain fluid in the setting of patellofemoral tracking syndromes or active Osgood-Schlatter disease.
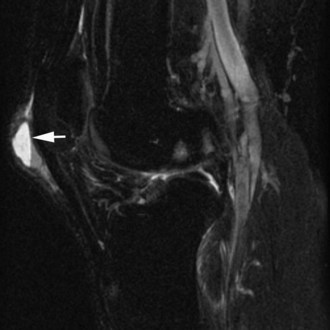
Laterally, the iliotibial band bursa is located between the tibia and the distal iliotibial band. Iliotibial band bursitis can manifest as anterolateral knee pain caused by overuse, often seen in runners. The fibular collateral ligament–biceps femoris bursa (Fig. 7-8) is lateral to the distal fibular collateral ligament, extending around the anterior and anteromedial aspects of the ligament. It extends proximally to where the biceps femoris crosses the fibular collateral ligament, and distally to the insertion of the fibular collateral ligament on the fibula.2
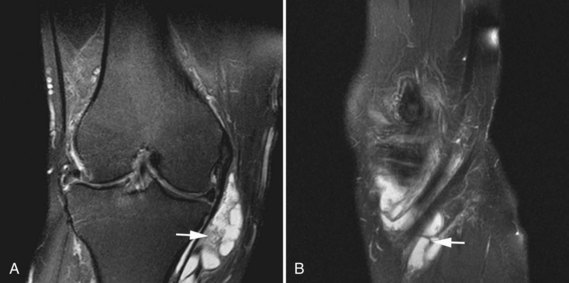
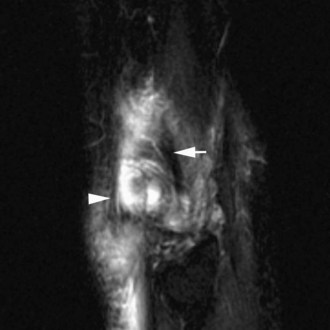
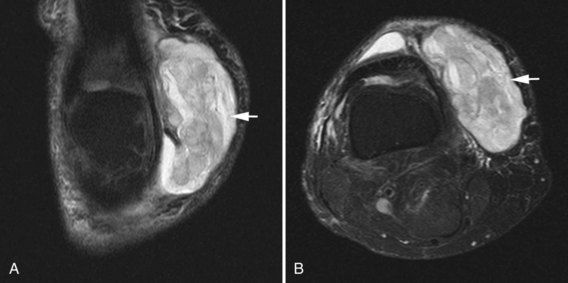
A posttraumatic Morel-Lavallee lesion may be mistaken as a bursitis on MRI (Fig. 7-9A and B). This closed degloving injury results from sudden severe trauma, often caused by motor vehicle accidents, that causes a shearing injury between the skin and subcutaneous fat and the underlying fascia. The perforating vessels and lymphatic channels are severed, resulting in a complex hematoma containing varying amounts of lymph and necrotic fat. On MRI, the lesion may show layering fluid levels related to layering blood products. A capsule may surround the mass and may be indicative of a lesion requiring surgical intervention; conservative treatments such as compression may be refractory.6
Bone Marrow Contusion Patterns
Careful observation and assessment of osseous contusions about the knee should serve as a guide for interrogation regarding suspect soft tissue structures likely to be injured based on specific mechanisms. Osseous contusion patterns often elucidate the mechanism of injury and guide the evaluation for subsequent pathology. Five dominant osseous contusion patterns described by Sanders and associates play a key role in diagnostic MRI interpretation of knee ligament trauma.18 These include pivot shift injury, dashboard injury, hyperextension injury, clip injury, and lateral patellar dislocation. MRI evaluation for osseous contusion is facilitated by the use of T2 fat-saturated sequences. Contusions appear as subcortical or subchondral regions of increased T2 signal and decreased T1 signal, often with a flame-shaped configuration, without a discrete fracture line.
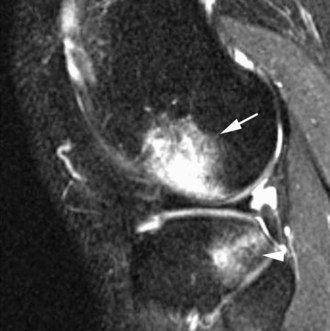
Following a pivot shift injury, osseous contusions most commonly involve the posterolateral tibial plateau and the lateral femoral condyle (Fig. 7-10). The presence of this contusion pattern indicates acute or chronic anterior cruciate ligament (ACL) disruption, as it is failure of this ligament that leads to tibial subluxation and impaction. Other associated pathology includes posterolateral corner injury and subsequent instability. Osseous contusion of the medial tibial plateau has also been described with a pivot shift mechanism of injury, present in approximately 20% of cases and associated with posteromedial peripheral tears of the medial meniscus.
The dashboard injury is related to a direct blow to the knee, often during an automobile accident. This mechanism manifests as contusions involving the anterior tibia and posterior, subchondral patella. Concomitant soft tissue injury with a dashboard contusion pattern often includes posterior cruciate ligament (PCL) and posterior capsule disruption. Hyperextension injury results in impaction of the anterior tibia and anterior femoral condyle, and subsequent osseous contusions (Fig. 7-11). Associated ligamentous pathology with this mechanism can include ACL or PCL injury.
A clip injury is related to valgus stress to the knee and results in a dominant contusion within the lateral femoral condyle from direct impaction, along with a smaller focus of bone marrow edema within the medial femoral condyle related to avulsive force at the origin of the medial collateral ligament. Injury to the medial collateral ligament is common with this mechanism, ranging from low-grade sprains to frank disruption. In addition, ACL injury and medial mensical injury have been described with clip injuries. Osseous contusions following lateral patellar dislocation involve the lateral, nonarticular portion of the lateral femoral condyle, as well as the medial patellar facet (Fig. 7-12). Associated soft tissue injuries include medial patellar retinaculum and medial patellofemoral ligament sprain or disruption. Cartilaginous injury has also been reported with transient lateral patellar dislocations, with delamination of cartilage at the medial patellar facet or at the anterolateral margin of the lateral femoral condyle, sometimes leading to intra-articular cartilaginous bodies.
Anterior Cruciate Ligament
On MRI, the ACL is low in signal relative to muscle on all sequences and parallels the intercondylar roof on sagittal images (Blumensaat’s line). The normal ligament may appear striated on sagittal images, presumably related to interposition of fat and synovium between the bundles, more commonly identified close to the tibial attachment.24 All three planes should be utilized for the most accurate assessment of the ACL. The sagittal sequence (Fig. 7-13) is most useful and can be performed in an oblique sagittal plane parallel to the orientation of the ACL as prescribed from an axial localizer image with 3 to 4 mm image thickness to decrease volume averaging. The axial and coronal images (Fig. 7-14) are useful in evaluating the ligamentous attachments and confirming abnormalities seen on the sagittal sequence. Axial images are particularly helpful for assessing the integrity of individual ACL bundles in the setting of sprain or partial tear.
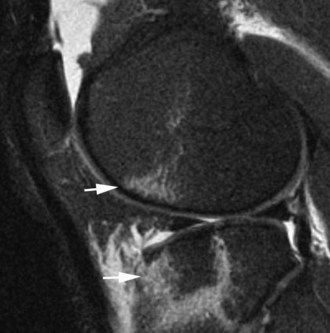
Both primary and secondary signs of ACL rupture have been seen on MRI. Primary signs of rupture include a discontinuous ligament or an abnormal course of the ligament, no longer paralleling Blumensaat’s line.24 With a discontinuous ligament, the fibers may appear wavy or horizontal in orientation (Fig. 7-15A). Often the ligament is replaced with amorphous increased signal related to edema and hemorrhage when tears are subacute; fibers appear as if they have been cut with scissors in more acute injuries (Fig. 7-15B). Secondary signs of ACL tear include buckling of the PCL, anterior translation of the tibia, uncovering of the posterior horn of the lateral meniscus, and characteristic osseous contusion patterns. Buckling of the PCL, uncovering of the posterior horn of the lateral meniscus, and anterior translation of the tibia are all related to anterior subluxation of the tibia relative to the femur secondary to ACL incompetence. Anterior translation of the tibia, referred to as the MRI equivalent of an anterior drawer sign, is assessed using the sagittal imaging plane (Fig. 7-16). The distance between the posterior tibia and the femoral condyle is measured using lines parallel to the long axis of the image. With this method, Vahey and colleagues demonstrated high specificity (93%) and positive predictive value (95%) of subluxation of 5 mm or more for ACL disruption. A 7 mm or greater subluxation had 100% specificity and positive predictive value.25 The characteristic osseous contusion pattern for ACL disruption involves the posterolateral tibial plateau and the lateral femoral condyle. Contusion may also be seen at the posteromedial tibial plateau. Complete rupture of the ACL is often accompanied by joint effusion and hemarthrosis. A fluid-fluid level representing layering blood products may be identified in the suprapatellar recess as related to patient positioning during the examination. In skeletally immature patients, ACL injury commonly manifests as an avulsion fracture at its insertion onto the tibia. MRI will demonstrate an intact ligament with an associated displaced osseous fragment at the medial tibial spine or the intercondylar tibial eminence (Fig. 7-17). Subchondral bone marrow edema may be seen within the proximal tibial epiphysis related to the fracture. With this injury, the immature epiphyseal bone is weaker than the mature ligament. Identification of the avulsed tibial fragment on radiography or MRI is essential, as treatment options differ considerably from those used with a traditional ACL rupture.
Partial tears of the ACL are more difficult to detect with MRI and are defined as abnormal intrasubstance signal within an otherwise intact ligament, or as discontinuity of some of the ligamentous fibers not involving the full width (Fig. 7-18). Commonly, the most proximal portion of the anterolateral bundle of the ACL is disrupted with an intact posteromedial bundle. Although this type of injury can be confidently called a partial ACL tear on MRI, ligamentous integrity is not easily established without a dedicated and properly performed physical examination. MRI is not a sensitive tool for determining the integrity of a partially torn ACL, although secondary signs such as pivot shift osseous contusions or an MRI anterior drawer can be helpful in suggesting ligamentous incompetence. In general, abnormal T2 hyperintense signal about or within a partially or completely intact ACL with a recent trauma history should be described as a partial tear of the ACL or low-grade ACL injury by MRI. This should be followed by a thorough description of the findings, the presence or lack of pivot shift contusions, and other findings that might suggest ligament incompetence.
ACL tears are often accompanied by other injuries of the ipsilateral knee. Medial collateral ligament sprain and meniscal tear are the most commonly associated injuries, with a particular prevalence of peripheral vertical tears in the posterior horn of either meniscus. Peripheral meniscus tears just above points of osseous contusion on the posterolateral or posteromedial tibial plateau are also commonly seen. Injuries to the posterolateral corner have been described in association with ACL disruption as well. The Segond fracture, an avulsion fracture from the lateral tibia at the lateral capsular ligament insertion, is an indicator of ACL disruption that can be seen on MRI, as well as on plain radiographs (Fig. 7-19).
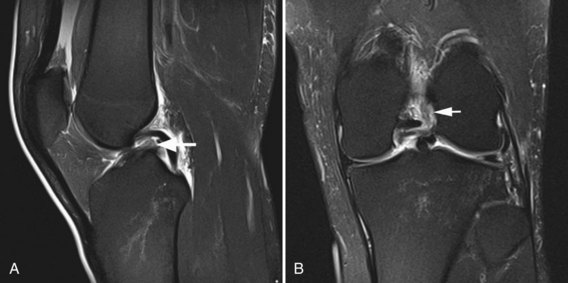
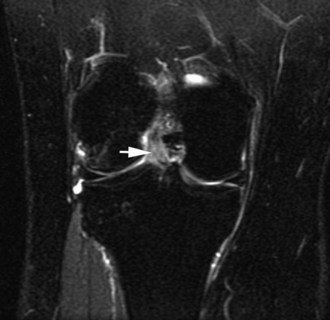
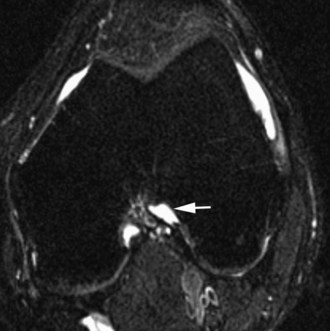
Nonvisualization of the ACL is the most common MRI presentation of a chronic tear. On axial images, fluid in the lateral intercondylar notch, where the normal ACL is found, described as the empty notch sign, can be seen in chronic ACL tears (Fig. 7-20). The ligament may be attenuated or residual fibers may have a horizontal orientation. The chronically torn ACL may scar and adhere to the PCL, and clinically may present with an endpoint on anterior drawer examination.24 Pivot shift contusions suggest ACL incompetence, but not necessarily an acute tear. A patient with a chronic and long-standing ACL tear can acutely pivot shift, leading to new contusions and a hemarthrosis, as well as injury to other ligamentous and cartilaginous structures. Therefore, pivot shift contusions and no visible ACL fibers at MRI should be interpreted as an age-indeterminate ACL tear, with a recent pivot shift injury. In contrast, mucoid degeneration of the ACL manifests as increased T2 signal, enlargement, and ill definition of an otherwise intact ligament. This pattern of ACL abnormality at MRI should not show a pivot shift contusion pattern and does not suggest the presence of acute ACL trauma, but more likely, chronic and repetitive abnormal ACL biomechanics related to meniscal tear or osteoarthritis. Mucoid degeneration of the ACL or PCL can be associated with osseous cystic formation at the cruciate attachments, distal more common than proximal. These intraosseous cruciate cysts are likely a variant of cruciate ganglion cysts, which show homogeneous increased T2 signal similar to that of fluid, insinuating between intact ligament bundles. They are loculated cysts often with lobulation and generally extending along the length of the ligament (Fig. 7-21).16
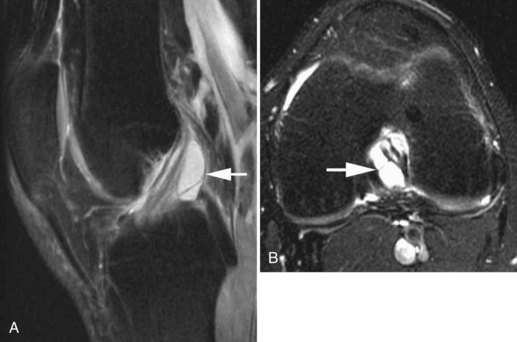
Interpretation of postoperative imaging of ACL grafts can be difficult, especially in the first 18 months to 2 years during graft neovascularization. Through this period, the graft can show increased T2 signal and may simulate acute ACL pathology, thereby decreasing MRI sensitivity for graft tear.23 Further, ACL reconstruction graft tears tend to manifest on MRI as focal signal heterogeneity or attenuation as opposed to the visible discontinuity seen with a native ACL tear. MRI evidence for a recent pivot shift mechanism or hemarthrosis is a useful tool in supporting the diagnosis of an ACL graft rupture or ACL graft incompetence. MRI in the postoperative setting is also appropriately used to evaluate graft impingement, tunnel placement, anterior arthrofibrosis, tunnel widening, and graft failure. With graft impingement related to an abnormally anteriorly placed tibial tunnel, the graft will show increased signal in the distal two thirds with visible deflection or angulation at the intercondylar roof on sagittal sequences acquired in near full knee extension (Fig. 7-22).8,24 Side wall impingement, related to a femoral tunnel low in the intercondylar notch, is best appreciated on coronal sequences. The graft will indent where it bends around the medial aspect of the lateral femoral condyle.24 Anterior arthrofibrosis, or cyclops lesion, can be a cause of limited knee extension and is easily identified on MRI. Tissue anterior to an ACL graft at the level of the joint line on sagittal imaging should follow the signal of fat on all sequences. A nodular mass of fibrous tissue anterior to the graft at the joint line and proximal to the tibial tunnel with intermediate to low in signal on T1- and T2-weighted images is typical for postoperative arthrofibrosis (Fig. 7-23).3,17 ACL graft tunnel widening or loosening will show as fluid signal surrounding the graft within the tunnel, tibial greater than femoral. MRI findings of graft tunnel widening are often present in conjunction with abnormal signal within the graft itself, indicating degeneration related to abnormal biomechanics. A bioabsorbable interference screw produces less susceptibility artifact than that seen with metal, so traditional noncontrast knee MRI protocols are generally diagnostic after ACL reconstruction. Intravenous contrast protocols can be useful for suspected postoperative synovitis or infection, but rarely provide much additional information in assessment of the graft itself. Lactide-glycolide screws may produce reactive edema, which is not seen with polylactic acid screws.26
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree