Abstract
Objective
Functional capacity evaluation is commonly used to assess the abilities of patients to perform some tasks. Ergo-Kit ® is a validated tool assessing both functional capacities of patients and workplace demands. The objective of this study was to evaluate the relevance of the Ergo-Kit ® data for occupational physicians during the return-to-work process.
Methods
A retrospective and monocenter study was conducted on all patients included in a rehabilitation program and assessed with the Ergo-Kit ® tool between 2005 and 2014. Workplace demands and patients’ functional capacities were evaluated and confronted. Self-beliefs and perceived disability were also assessed and compared to the functional capacity evaluation.
Results
One hundred and forty-nine working-age patients (85 men, 64 women; 39 ± 12 years) suffering from musculoskeletal disorders or other diseases were included. Main causes of mismatch between workplace demands and functional capacities were manual handling of loads, postures with arms away from the body and repetitive motions at work; sitting posture was correlated with a lesser physical workload; and Oswestry score was correlated with functional capacities evaluated by the Ergo-Kit ® .
Conclusion
Ergo-Kit ® is a relevant tool to assess the multidimensional aspects of workplace demands and functional capacities. It could be very helpful for occupational physicians to manage return-to-work.
1
Introduction
Work capacity evaluation (WCE) is dedicated to assess work capacities of a person to perform a job. The WCE describes, analyzes tasks as well as workplace demands (WPD) according to different strategies and determines how the worker can face up to them . It is most often conducted in Physical Medicine and Rehabilitation Centers (PM&R). It contributes to the rehabilitation program organization, the return-to-work (RTW) prognosis, its implementation (safe and sustainable), even when necessary it may contribute to career change and can help determinate eventual rights to workers’ compensation . There are two WCE categories: evaluation in the workplace environment and Functional Capacity Evaluation (FCE) . There are job-specific FCEs that include real-life situations by simulating work tasks, as well as general FCEs.
Ergo-Kit ® (EK) marketed by “Ergo control” (Netherlands) is a validated tool to conduct FCEs and WPD evaluations. It consists in a battery of 55 standardized physical tests measuring a worker’s maximum capacities according to certain WPDs such as manual handling of loads (MHL), manual dexterity, ability to maintain demanding postures, etc. This assessment is conducted in a healthcare environment and the recommendation given afterwards is a presumption on the compatibility between the person’s functional status and general job tasks. A recommendation on the real-life compatibility can only be expressed after conducting a WCE in the workplace .
In the literature, FCE performance is influenced by physical factors (i.e. age, sex), type and duration of the disability, presence of associated pain and its intensity, as well as psychological factors (i.e. perception of the disability, anxiety-depression, self-assessment of functional capacities) .
The EK, marketed in The Netherlands since 1993, is available in three other European countries (Belgium, Luxemburg and France). The use of this tool requires a specific training delivered by the company manufacturing the EK. To our knowledge, no French study has evaluated the results of FCEs using the EK.
The RTW issue consists in evaluating a worker’s functional capacities (FC) in order to return to work to the same position or another one with no risk to the worker’s health. The main objective of this study was to conduct a synthesis of all elements yielded by the EK useful to healthcare professionals involved in the RTW process, especially the occupational physician (OP), about work conditions compatible with a safe RTW. The second objective was to evaluate associations between self-assessed disability indicators and FCE results, which can guide the decisions of the OP.
2
Material
This descriptive, retrospective monocenter study was conducted on all the medical charts of patients evaluated in the PM&R department of the Angers University Hospital in France from March 2005 to April 2014. Over this time period, 209 EK evaluations were conducted for a total of 185 patients, including 149 patients in RTW or stay-at-work situations (persons with job difficulties and/or on sick leave or out of a job or on disability leave). Patients were seen either as inpatients or outpatients in the Adult or Pediatric units of the PM&R department.
Study inclusion criteria were: being between 15 and 65 years of age, having one of the following work statuses: employee, employer with a salary, independent worker, apprentice, unemployed worker or worker on disability leave, being in RTW or stay-at-work situation, having signed the study’s participation consent form as well as parental consent form for minors. Exclusion criteria were: being a student, retired or with an unknown work status, having a contraindication to perform the EK assessment (usual contraindications related to intensive efforts, see Appendix 1 ).
The various EK tests follow a standardized protocol . A French adaptation of this protocol (Ergo-Kit ® manual) was conducted by the PM&R department and is used as a reference and basis for the EK trainings of the French-speaking teams; this protocol has not yet been validated. Two types of EK evaluations are possible:
- •
half-day assessment: pre-assessment interview and FCE;
- •
full-day assessment: pre-assessment interview, WPD evaluation and FCE.
The WPD evaluation is conducted in the context of stay-at-work conditions and when patients are able to describe their job tasks. However, a WPD evaluation can be necessary when the patient does not have a job (to help guide and promote the choice of a new professional orientation). The reason for conducting a WPD evaluation has to be validated by the PM&R physician who prescribed the evaluation.
These two types of evaluations generate a writing report using the Ergo Control software. All these evaluations were conducted by three occupational therapists from the PM&R department trained to conduct the EK protocol.
2.1
Pre-assessment interview
It consists in collecting the following elements:
- •
sociodemographic data: age, sex, type of evaluation and date of the evaluation;
- •
medical data: habits (tobacco and/or alcohol use), history of the disease, diagnosis, treatment, medical history and associated disorders, collected by the occupational therapist based on the information given by the patient as well as the evaluation request form filled out by prescribing physician;
- •
current sport practice;
- •
clinical data: height, weight, dominant hand, blood pressure and heart rate;
- •
social and occupational data: educational attainment, number of professional experience work years, position, length of service, being on sick leave or not, duration of professional inactivity and self-assessment on the ability to work;
- •
self-questionnaire on functional disability: the Oswestry pain & disability questionnaire translated and validated in French with the addition of an 11th question (“Are there any other housework or leisure activities you are not able to perform?”). The initial objective of the Oswestry low-back pain questionnaire was to measure the functional impact of low-back pain on activities of daily leaving . This score has a high validity and reliability . Results are expressed in disability percentages out of 100 and are analyzed as such: 0–20%: minimal disability; 21–40%: moderate disability; 41–60%: severe disability; 61–100%: extremely severe disability. The 11th open question was added in order to collect eventual missing data.
2.2
Functional capacity evaluation (FCE)
FCs are quantified according to the Department of Labor (DOL) USA system, allowing the analysis of physical characteristics of occupational activities grouped into the Dictionary of Occupational Titles 1991 (DOT) . The EK evaluates 27 functional abilities of the DOL system: 12 MHL abilities and 15 other abilities ( Appendix 2 ).
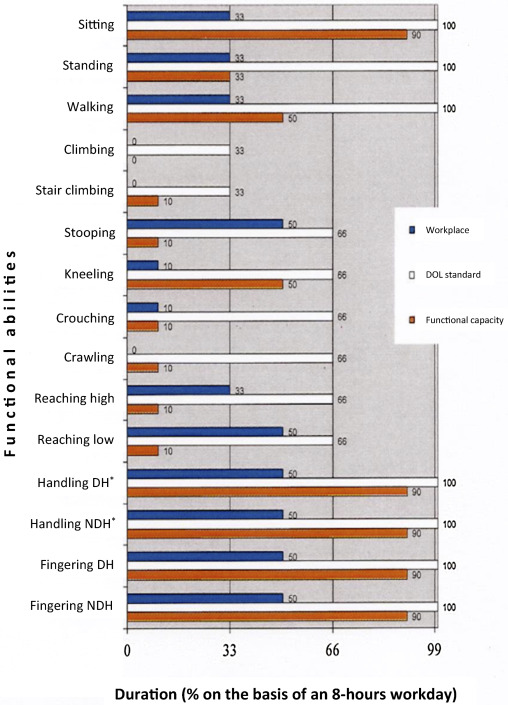
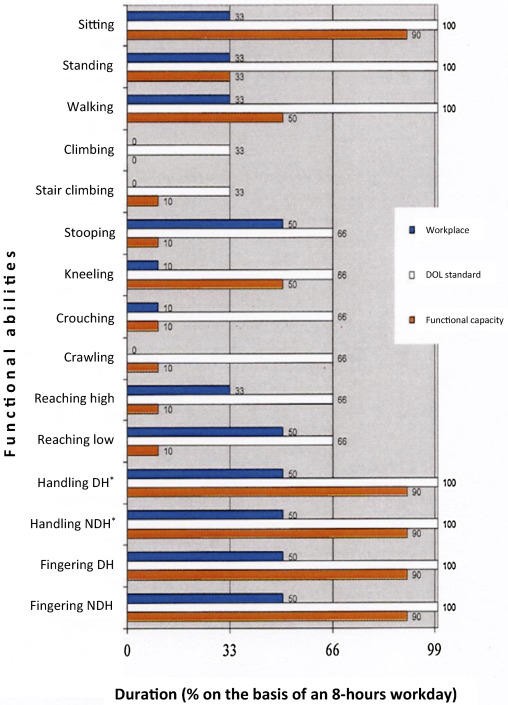
The FCE is entirely performed with the EK, which includes a Purdue Peg Board Test (neuropsychological test of manual dexterity and bimanual coordination), a Jamar manual dynamometer, a dynamometer platform, a column with adjustable elements and a step platform to conduct 55 physical tests ( Figs. 1 and 2 ). Each functional ability is assessed by the occupational therapist taking into account one or more of its related physical tests and following a reasoning and analytic protocol. The FCs belonging to the MHL category are estimated in maximal weight (kg) that can be lifted or moved for each time-period (in frequency) of the DOL system ( Appendix 2 , example: occasionally lowering 7.5 kg = the patient is able to lift a load of 7.5 kg, lowering from the floor to the waist up to 32 times a day). The other FCs are estimated in percentages of an 8-hour workday (example: sitting down 90% = the patient is able to sit down for up to 90% of the workday). The FCs are compared to the norms of the DOL system and the WPDs when available, within an analytic diagram ( Fig. 3 ). After the evaluation, a validity score from 1 to 5 is calculated comparing the results of different physical tests measuring similar abilities (for example: study on the coherence of the curves for the two Jamar dynamometer reproducibility tests). This score is able to determine if one can take into account all the results of the FCE for a given patient. The higher the score, the higher the tests’ validity.


2.3
Workplace demands (WPD) evaluation
A WPD evaluation is not systematic and depends on the EK indication. Three detailed self-questionnaires are mailed, prior to the evaluation, to the patient’s home:
- •
personal information questionnaire: sociodemographic data (useful during the preliminary interview);
- •
“work” questionnaire: type of work contract, work schedule, work rate, autonomy, opportunities for career development;
- •
“work actions” questionnaire: for each task the different actions are detailed.
The WPD evaluation corresponds to evaluating the physical constraints related to the job during an interview with the patient, after the preliminary interview and before the FCE. From the data in the “work actions” questionnaire, a total arduousness index score on 100 is computed from the arduousness indexes of each action. A “work abilities” form filled out by the occupational therapist helps quantify the WPDs according to the DOL system.
2
Material
This descriptive, retrospective monocenter study was conducted on all the medical charts of patients evaluated in the PM&R department of the Angers University Hospital in France from March 2005 to April 2014. Over this time period, 209 EK evaluations were conducted for a total of 185 patients, including 149 patients in RTW or stay-at-work situations (persons with job difficulties and/or on sick leave or out of a job or on disability leave). Patients were seen either as inpatients or outpatients in the Adult or Pediatric units of the PM&R department.
Study inclusion criteria were: being between 15 and 65 years of age, having one of the following work statuses: employee, employer with a salary, independent worker, apprentice, unemployed worker or worker on disability leave, being in RTW or stay-at-work situation, having signed the study’s participation consent form as well as parental consent form for minors. Exclusion criteria were: being a student, retired or with an unknown work status, having a contraindication to perform the EK assessment (usual contraindications related to intensive efforts, see Appendix 1 ).
The various EK tests follow a standardized protocol . A French adaptation of this protocol (Ergo-Kit ® manual) was conducted by the PM&R department and is used as a reference and basis for the EK trainings of the French-speaking teams; this protocol has not yet been validated. Two types of EK evaluations are possible:
- •
half-day assessment: pre-assessment interview and FCE;
- •
full-day assessment: pre-assessment interview, WPD evaluation and FCE.
The WPD evaluation is conducted in the context of stay-at-work conditions and when patients are able to describe their job tasks. However, a WPD evaluation can be necessary when the patient does not have a job (to help guide and promote the choice of a new professional orientation). The reason for conducting a WPD evaluation has to be validated by the PM&R physician who prescribed the evaluation.
These two types of evaluations generate a writing report using the Ergo Control software. All these evaluations were conducted by three occupational therapists from the PM&R department trained to conduct the EK protocol.
2.1
Pre-assessment interview
It consists in collecting the following elements:
- •
sociodemographic data: age, sex, type of evaluation and date of the evaluation;
- •
medical data: habits (tobacco and/or alcohol use), history of the disease, diagnosis, treatment, medical history and associated disorders, collected by the occupational therapist based on the information given by the patient as well as the evaluation request form filled out by prescribing physician;
- •
current sport practice;
- •
clinical data: height, weight, dominant hand, blood pressure and heart rate;
- •
social and occupational data: educational attainment, number of professional experience work years, position, length of service, being on sick leave or not, duration of professional inactivity and self-assessment on the ability to work;
- •
self-questionnaire on functional disability: the Oswestry pain & disability questionnaire translated and validated in French with the addition of an 11th question (“Are there any other housework or leisure activities you are not able to perform?”). The initial objective of the Oswestry low-back pain questionnaire was to measure the functional impact of low-back pain on activities of daily leaving . This score has a high validity and reliability . Results are expressed in disability percentages out of 100 and are analyzed as such: 0–20%: minimal disability; 21–40%: moderate disability; 41–60%: severe disability; 61–100%: extremely severe disability. The 11th open question was added in order to collect eventual missing data.
2.2
Functional capacity evaluation (FCE)
FCs are quantified according to the Department of Labor (DOL) USA system, allowing the analysis of physical characteristics of occupational activities grouped into the Dictionary of Occupational Titles 1991 (DOT) . The EK evaluates 27 functional abilities of the DOL system: 12 MHL abilities and 15 other abilities ( Appendix 2 ).
The FCE is entirely performed with the EK, which includes a Purdue Peg Board Test (neuropsychological test of manual dexterity and bimanual coordination), a Jamar manual dynamometer, a dynamometer platform, a column with adjustable elements and a step platform to conduct 55 physical tests ( Figs. 1 and 2 ). Each functional ability is assessed by the occupational therapist taking into account one or more of its related physical tests and following a reasoning and analytic protocol. The FCs belonging to the MHL category are estimated in maximal weight (kg) that can be lifted or moved for each time-period (in frequency) of the DOL system ( Appendix 2 , example: occasionally lowering 7.5 kg = the patient is able to lift a load of 7.5 kg, lowering from the floor to the waist up to 32 times a day). The other FCs are estimated in percentages of an 8-hour workday (example: sitting down 90% = the patient is able to sit down for up to 90% of the workday). The FCs are compared to the norms of the DOL system and the WPDs when available, within an analytic diagram ( Fig. 3 ). After the evaluation, a validity score from 1 to 5 is calculated comparing the results of different physical tests measuring similar abilities (for example: study on the coherence of the curves for the two Jamar dynamometer reproducibility tests). This score is able to determine if one can take into account all the results of the FCE for a given patient. The higher the score, the higher the tests’ validity.


2.3
Workplace demands (WPD) evaluation
A WPD evaluation is not systematic and depends on the EK indication. Three detailed self-questionnaires are mailed, prior to the evaluation, to the patient’s home:
- •
personal information questionnaire: sociodemographic data (useful during the preliminary interview);
- •
“work” questionnaire: type of work contract, work schedule, work rate, autonomy, opportunities for career development;
- •
“work actions” questionnaire: for each task the different actions are detailed.
The WPD evaluation corresponds to evaluating the physical constraints related to the job during an interview with the patient, after the preliminary interview and before the FCE. From the data in the “work actions” questionnaire, a total arduousness index score on 100 is computed from the arduousness indexes of each action. A “work abilities” form filled out by the occupational therapist helps quantify the WPDs according to the DOL system.
3
Methods
WPDs were compared to ( Table 1 ):
- •
MHL threshold values of the AFNOR NF X 35-109 norm to lift and move loads ;
- •
exposure durations defining arduous situations and constraining postures from the Summer 2003 study ;
- •
exposure durations described as specific risk factors for musculoskeletal disorders (MSD) of the upper limb ;
- •
DOL standards used in the EK protocol.
| Ability | SUMER 2003 study | MSD thresholds | Extrapolated values | DOL standards | ||
|---|---|---|---|---|---|---|
| hpw | % | hpd | % | % | % | |
| Sitting | 50 | |||||
| Standing | 20 | 50 | ||||
| Walking | 20 | 50 | ||||
| Climbing | 25 | 33 | ||||
| Stair climbing | 25 | 33 | ||||
| Stooping | 25 | 66 | ||||
| Kneeling | 25 | 66 | ||||
| Crouching | 25 | 66 | ||||
| Crawling | 25 | 66 | ||||
| Reaching high | 2 | 25 | 66 | |||
| Reaching low | 2 | 25 | 66 | |||
| Handling DH | 20 | 50 | 2 | 25 | ||
| Handling NDH | 20 | 50 | 2 | 25 | ||
| Fingering DH | 4 | 50 | ||||
| Fingering NDH | 4 | 50 | ||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






