Abstract
The objective of this work was to analyze the inter-observer reproducibility of an upright posture designed to bring out the thoracic humps by folding the upper limbs. The effect of this posture on back surface parameters was also compared with two standard radiological postures. A back surface topography was performed on 46 patients (40 girls and 6 boys) with a minimum of 15° Cobb angle on coronal spinal radiographs. Inter-observer reliability was evaluated using the typical error measurement (TEM) and Intraclass Correlation Coefficient (ICC). Variations between postures were assessed using a Student’s t test. The inter-observer reproducibility is good enough for the three postures. The proposed posture leads to significant changes in the sagittal plane as well as in the identification of thoracic humps. This study shows the reproducibility of the proposed posture in order to explore the thoracic humps and highlights its relevance to explore scoliosis with back surface topography systems.
Résumé
L’objectif de ce travail était d’analyser la reproductibilité inter-observateur d’une posture debout permettant de visualiser les gibbosités thoraciques par un enroulement antérieur des bras (position « enroulée ») et de comparer l’effet de cette position sur les paramètres surfaciques habituellement mesurés dans deux positions radiologiques standards. Une analyse topographique de la surface du dos a été réalisée sur 46 patients (40 filles et 6 garçons) présentant un angle de Cobb d’au moins 15° sur des grands clichés du rachis de face. La reproductibilité des mesures inter-examinateurs a été évaluée à l’aide de l’erreur technique de mesure (ETM) et du coefficient de corrélation intraclasse (CCI). Les variations entre les positions étaient comparées par un test de Student. Nos résultats montrent que la reproductibilité inter-observateur des mesures semble de qualité suffisante dans les trois positions étudiées. La position « enroulée » entraînait des modifications significatives dans le plan sagittal ainsi que pour l’identification des gibbosités par rapport à celles observées dans les deux autres positions. Cette étude révèle la reproductibilité de la position « enroulée » et sa complémentarité vis-à-vis des positions habituelles, permettant de mieux explorer les gibbosités thoraciques avec les outils de topographie de surface du dos.
1
English version
1.1
Introduction
Idiopathic scoliosis is a three-dimensional deformity of the spine. Its estimated frequency comes to around 3% of the population . In clinical practice, the existence of a gibbosity, also known as a hump or Kelso’s hunchback, can facilitate scoliosis diagnosis . Detection of the gibbosity is brought about with a scoliometer and the Adam’s test, which involves forward bending of the spine allowing for measurement of the gibbosity, while vertical suspension of the upper limbs will highlight the thoracic kyphosis.
In clinical practice, radiological follow-up plays a major role in treatment decisions on account of its reproducibility . However, X-ray exposure is not without risks, particularly in scoliotic girls . Numerous back surface topography systems have been developed in order to limit the number of X-rays taken. Originally, these systems were designed to replace mass screening for scoliosis by a non-ionizing and easily transportable tool . Following which, the main objective was to limit the number of X-rays carried out during therapeutic follow-up . An obstacle to further development of back surface topography consisted in a lack of adequate correlation between the surface measurements carried out in the usual postures and the Cobb angle measurements obtained with X-rays . And today, even though it remains uncertain that these systems can effectively reduce the number of X-rays taken , they aspire to preeminence in the management of young scoliosis patients.
In order to facilitate comparison with radiographic parameters, the acquisitions of back surface topography must come about in positions close to the radiographic positions of reference, that is to say principally the “clavical” and “straight out” postures .
The objective of this work was to analyze the reproducibility of an upright posture known as “folding”, which facilitates visualization of the thoracic gibbosity by partially flexing the arms, and to consider the effect of this position on the back surface parameters generally measured in the “clavical” and “straight out” positions.
1.2
Materials and methods
1.2.1
Subjects
This is a prospective study conducted in the medical orthopedics unit of the Bordeaux university hospital. In accordance with the Helsinki declaration, all of the subjects were recruited with their voluntary and informed consent. The inclusion criteria were issued from radiologic criteria corresponding to a Cobb angle of at least 15° on full frontal X-rays of the spine following possible correction of the unequal length of the lower limbs. The exclusion criteria consisted in the presence of clinical or radiological anomalies suggesting symptomatic scoliosis.
A back surface topography analysis was carried out on 46 patients (40 girls and 6 boys). Characterization of the scoliosis revealed: 36 (78.3%) double curvatures, 9 (19.6%) single curvatures and 1 (2.1%) triple curvatures. Maximum Cobb angles averaged 26.8 ± 10 degrees.
1.2.2
Instrumentation
Measurements were carried out with a BIOMOD TM L system (AXS MEDICAL SAS, Mérignac, France). This apparatus is a medical device authorized for use in clinical practice. It consists in a mobile optical data acquisition system applied to the surface of the back and in measurement processing software. The acquisition system includes a high-definition camera, inclinometers and a structured light projector. Deformation of the projected images provides 3D relief texture of the back surface. Acquisition time comes to 40 ms.
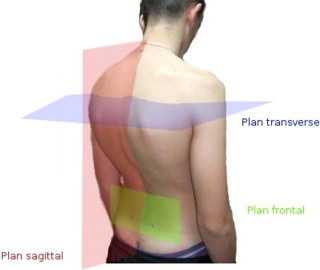
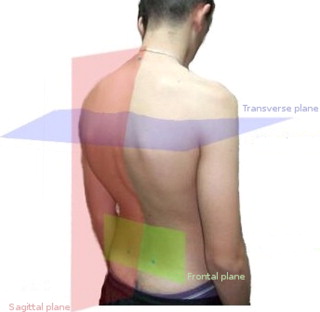
The 3D relief was processed on dedicated software to obtain clinical measurements. Automatic detection was carried out on the anatomical landmarks indicated by the operator. The landmarks included the spinous processes (from C7 to the top of the intergluteal cleft) as well as the “Michaelis” sacral dimples. The measurements were then performed in a reference system connected with the landmarks, and evaluated on 3 planes: the frontal plane, the sagittal plane and the transverse plane. The planes were defined as follows; the frontal plane was the vertical plane spanning the sacral dimples; the sagittal plane was the vertical plane perpendicular to the frontal plane; the transverse plane was the horizontal plane. The top of the intergluteal cleft defined by the examiner was the source of the landmark formed by the intersection of the three planes ( Fig. 1 ).
1.2.3
The acquisition protocol
Preliminarily to acquisition, the subjects were asked to strip down to their underwear and bare their feet. The examiner marked down the predefined anatomical points with a red pencil. The subject was positioned with his back to the apparatus and asked to maintain this posture, without moving, while the acquisition was taking place.
Two distinct examiners performed separate acquisition series and took immediate note of the parameters under analysis. Between the series, the marks were completely removed from the patients’ skin. Each acquisition series involved a preparation stage and three acquisitions in three different positions, also known as “postures” or “stances”, each of which was explained and shown by the examiner ( Fig. 2 ).

The “clavical” position is a validated radiologic position of reference . Standing and relaxed in what is also an anatomical position of reference, the patient was asked to bend his elbow, wrists and fingers so as to place the dorsal surface of the 2nd phalanges of the last two fingers in contact with the collarbones.
The “straight out” posture has likewise been radiologically validated . The patient was asked to bring his arms forward and to place his hands on a support in such a way that the forearms were horizontal.
The “folding” posture that constitutes the subject of this study was aimed at highlighting the thoracic gibbosities. The patient was asked to bend his shoulders, elbows and wrists so that the dorsal surface of the wrist would be in contact with the chin, while the ulnar sides of the forearms would be in contact with each other up to the elbows.
After each acquisition, the examiner validated the automatic location of the anatomical landmarks and the spinous processes. After validation, the different parameters were calculated automatically with the exception of the gibbosity measurements, which necessitated complementary manual intervention.
1.2.4
The parameters
Through use of the software, a large number of measurements can be carried out. For reasons of concision, however, only some of the measurements commonly found in the literature were taken into consideration for the purposes of this study.
1.2.4.1
On the frontal plane
Pelvic imbalance was the angle formed between the horizontal plane and the line spanning the sacral dimples ( Fig. 3 ).
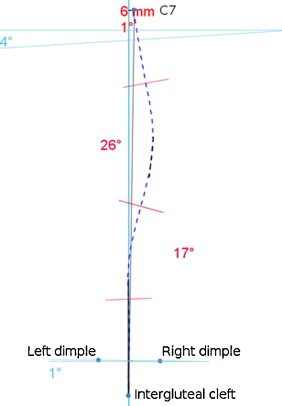
The C7 lateral deviation was the distance between the C7 spinous processes and the vertical plane spanning the top of the intergluteal cleft (positive on the right, negative on the left).
The spinal sinuosity angles, which correspond to the angles proposed by Stagnara , were the camber angles of the spinous processes situated between two inflection points of that line. Taking into account the height at which the angle is located, we have defined three zones: thoracic sinuosity, thoracolumbar sinuosity and lumbar sinuosity. Only angles equal to or greater than 10° were factored into the analysis.
1.2.4.2
On the sagittal plane
In order to avoid negative values, we have measured the plumb lines according to their clinical definition by means of the plumb line techniques spanning the most posterior point of the spinous processes ( Fig. 4 ). As a general rule, in lordotic back in antiflexion, the zero value of reference spanned the top of the intergluteal cleft; in the kyphotic back, the zero value of reference spanned the top of the kyphosis. Correspondingly, the C7 plumb line arrow was the distance from the C7 spinous processes relative to the vertical line spanning the most posterior point of those processes.
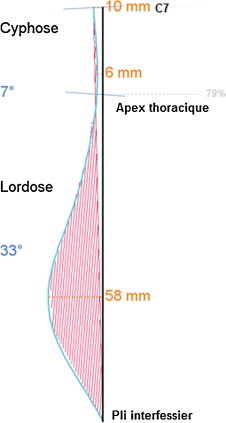
The thoracic arrow represented the distance between the most posterior point of the spinous processes at the level of the thoracic kyphosis relative to the vertical line spanning the most posterior segment of the processes.
The lumbar arrow represented the distance between the most anterior point of the spinous processes at the level of the lumbar lordosis relative to the vertical line spanning the most posterior segment of the processes.
The inflection point was the intersection point by the spinous processes and the segment consisting in C7 and the intergluteal cleft (0% corresponding to the top of the intergluteal cleft and 100% to the C7 spinal process).
The kyphotic angle was the angle formed by the perpendicular lines at the C7 spinal processes and at the inflection point.
The lordotic angle was the angle formed by the perpendicular lines at the spinal processes at the inflection point and at the top of the intergluteal cleft.
1.2.4.3
On the transverse plane
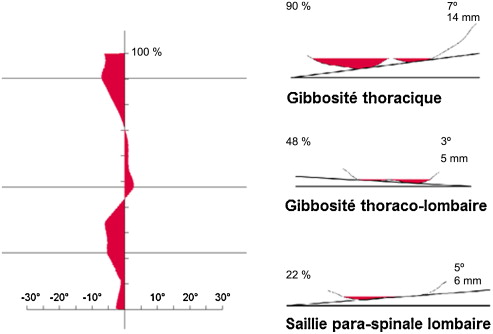
The software automatically exposed a diagram highlighting the size of the gibbosities or humps all along the top of the spinal axis ( Fig. 5 ). The examiner placed a marker on each upward convexity of the exposed curve and could thenceforth define three maximal deformities: thoracic gibbosity, thoracolumbar gibbosity and paraspinal or lumbar prominence. For each deformity, maximum rotation relative to the frontal plane and the height of the deformity relative to the C7-intergluteal cleft were recorded.
1.3
Statistical analysis of the data
Data collection and processing were carried in the form of an EXCEL ® table applying the advanced statistical functions of the software.
Reliability of the inter-examiner measurements was evaluated with Typical Error Measurement (TEM) and the intraclass correlation coefficient (ICC). TEM facilitates exposure of the variations of a measurement carried out repeatedly on an individual , while the ICC is a coefficient of reproducibility facilitating evaluation of the proportion of variations of a measurement carried out repeatedly, when the proportion is not due to an error of measurement . The relevant calculations were performed on the spreadsheets developed by Hopkins et al. . Using the indications existing in the literature as a basic reference, the ICC values were classified as follows: poor: ICC < 0.40; fair: 0.40 < ICC < 0.60; good: 0.60 < ICC < 0.80; excellent ICC > 0.80.
The variations in quantitative values between the different positions were compared by bilateral Student’s t test on matched data (significance threshold p < 0.05).
1.4
Results
1.4.1
Inter-observer reproducibility
1.4.1.1
On the transverse plane
In the three positions, the TEM values for the gibbosities and the paraspinal lumbar prominence showed amplitudes of variation lower than two degrees ( Table 1 ). The ICCs were good or excellent for all parameters in the “folding” posture. They were likewise good or excellent in the “clavical” posture and fair to excellent in the “straight out” posture.
| Parameter | “Clavical” position | “Folding” position | “Straight out” position | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M | ET | ETM | CCI | n | M | ET | ETM | CCI | n | M | ET | ETM | CCI | |
| Thoracic gibbosity (°) | 41 | 5.2 | 2.7 | 1.5 | 0.700 | 37 | 5.6 | 2.9 | 1.5 | 0.743 | 40 | 5.0 | 2.9 | 1.9 | 0.591 |
| Thoracic height (%) | 41 | 74.3 | 11.3 | 4.9 | 0.819 | 37 | 76.3 | 9.6 | 4.0 | 0.835 | 40 | 75.0 | 10.8 | 4.2 | 0.859 |
| Thoracolumbar gibbosity (°) | 38 | 4.7 | 3.1 | 1.5 | 0.782 | 29 | 6.0 | 3.3 | 1.8 | 0.699 | 34 | 5.1 | 3.2 | 1.4 | 0.824 |
| Thoracolumbar height (%) | 38 | 50.5 | 10.2 | 3.7 | 0.875 | 29 | 51.0 | 11.1 | 1.6 | 0.980 | 34 | 51.1 | 11.1 | 3.0 | 0.933 |
| Paraspinal lumbar prominence (°) | 36 | 4.7 | 3.5 | 1.4 | 0.843 | 37 | 5.2 | 3.9 | 1.4 | 0.871 | 35 | 5.3 | 4.0 | 1.1 | 0.934 |
| Lumbar height (%) | 36 | 30.6 | 7.2 | 3.2 | 0.806 | 37 | 30.5 | 6.8 | 2.4 | 0.883 | 35 | 31.6 | 7.3 | 2.0 | 0.932 |
As for the thoracic and thoracolumbar sinuosity, inter-observer reproducibility qualities were classified as excellent in the “folding” positions and in the other two positions, as well. Evaluation of the reproducibility quality of pelvic balance was classified as good in the “folding” and “clavical” postures and fair in the “straight out” stance. On the other hand, the ICCs of the lumbar sinuosity angle were not statistically significant in any of the positions; this was due to the low number of patients presenting with this deformity ( n < 9).
1.4.1.2
On the frontal plane
As regards the thoracic sinuosity and thoracolumbar angles, the inter-observer reproducibility qualities were classified as excellent in the “folding” posture, as well as the other two positions. Evaluation of the reproducibility quality of pelvic balance was classified as good in the “folding” and “clavical” positions and as fair in the “straight out” position. On the other hand, the ICCs of the lumbar sinuosity angle were not statistically significant in any of the positions; this was due to the low number of patients presenting with this deformity ( n < 9) ( Table 2 ).
| Parameter | “Clavical” position | “Folding” position | “Straight out” position | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M | ET | ETM | CCI | n | M | ET | ETM | CCI | n | M | ET | ETM | CCI | |
| Lateral deviation of C7 (mm) | 46 | −5.9 | 14.6 | 5.2 | 0.875 | 46 | −4.0 | 16.4 | 5.4 | 0.897 | 46 | −5.8 | 16.4 | 4.5 | 0.927 |
| Pelvic imbalance (°) | 46 | 2.1 | 2.4 | 1.3 | 0.693 | 46 | 2.1 | 2.5 | 1.6 | 0.611 | 46 | 1.9 | 2.4 | 1.7 | 0.515 |
| Thoracic sinuosity (°) | 29 | 11.5 | 18.2 | 3.8 | 0.960 | 30 | 12.0 | 19.1 | 3.7 | 0.965 | 29 | 13.4 | 18.0 | 4.2 | 0.950 |
| Thoracolumbar sinuosity (°) | 32 | −8.3 | 16.2 | 3.4 | 0.958 | 32 | −8.6 | 16.4 | 4.6 | 0.926 | 33 | −9.2 | 15.7 | 4.8 | 0.910 |
| Lumbar sinuosity (°) | 7 | −12.8 | 13.8 | 13.0 | 0.134 | 8 | −10.1 | 14.2 | 9.7 | 0.610 | 8 | −13.6 | 8.6 | 6.8 | 0.444 |
1.4.1.3
On the sagittal plane
The reproducibility qualities of the sagittal parameters measured in the “folding” posture were consistently classified as good or excellent. They tended to vary from good to excellent in the “clavical” posture, and from fair to excellent in the “straight out” posture ( Table 3 ).
| Parameter | “Clavical” position | “Folding” position | “Straight out” position | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M | ET | ETM | CCI | n | M | ET | ETM | CCI | n | M | ET | ETM | CCI | |
| C7 arrow (mm) | 46 | 38.3 | 20.2 | 7.1 | 0.882 | 46 | 33.3 | 20.5 | 9.3 | 0.801 | 46 | 35.8 | 19.4 | 6.1 | 0.906 |
| Thoracic arrow (mm) | 46 | 7.3 | 9.7 | 4.5 | 0.794 | 46 | 4.1 | 11.0 | 5.0 | 0.804 | 46 | 4.5 | 6.9 | 3.3 | 0.775 |
| Lumbar arrow (mm) | 46 | 46.1 | 9.7 | 6.0 | 0.628 | 46 | 50.4 | 12.3 | 6.2 | 0.755 | 46 | 47.3 | 10.8 | 5.3 | 0.772 |
| Height of inflection point (%) | 46 | 49.8 | 10.8 | 3.8 | 0.878 | 46 | 48.7 | 13.5 | 4.5 | 0.895 | 46 | 49.0 | 12.5 | 5.8 | 0.790 |
| Kyphotic angle (°) | 46 | 29.9 | 11.0 | 4.3 | 0.853 | 46 | 32.1 | 11.1 | 4.3 | 0.855 | 46 | 31.5 | 11.4 | 3.0 | 0.932 |
| Lordotic angle (°) | 46 | 36.0 | 6.8 | 2.8 | 0.833 | 46 | 37.3 | 7.0 | 2.7 | 0.857 | 46 | 37.1 | 7.0 | 4.5 | 0.599 |
1.4.2
Comparison of the “folding”, “clavical” and “straight out” positions
For the sake of readability we are limiting the information reported in this chapter to statistically significant differences. For details on the values of each parameter, the reader may refer to Table 4 .
| “Clavical” vs. “Folding” | “Clavical” vs. “Straight out” | “Folding” vs. “Straight out” | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | p | Ddiff | n | p | Diff | n | p | Diff | |
| Frontal plane parameters | |||||||||
| C7 lateral deviation (mm) | 92 | 0.042 | * | 92 | 0.873 | – | 92 | 0.042 | * |
| Pelvic imbalance (°) | 92 | 0.725 | – | 92 | 0.417 | – | 92 | 1.000 | – |
| Thoracic sinuosity angle (°) | 59 | 0.282 | – | 58 | 0.053 | – | 58 | 0.697 | – |
| Thoracolumbar sinuosity angle (°) | 64 | 0.314 | – | 63 | 0.520 | – | 64 | 0.377 | – |
| Lumbar sinuosity angle (°) | 15 | 0.516 | – | 15 | 0.785 | – | 16 | 0.428 | – |
| Sagittal plane parameters | |||||||||
| C7 arrow (mm) | 92 | 0.003 | ** | 92 | 0.060 | – | 92 | 0.048 | * |
| Thoracic arrow (mm) | 92 | 0.031 | * | 92 | 0.003 | ** | 92 | 0.740 | – |
| Lumbar arrow (mm) | 92 | 0.000 | ** | 92 | 0.206 | – | 92 | 0.008 | ** |
| Height of inflection point (%) | 92 | 0.196 | – | 92 | 0.213 | – | 92 | 0.796 | – |
| Kyphotic angle (°) | 92 | 0.003 | ** | 92 | 0.015 | * | 92 | 0.423 | – |
| Lordotic angle (°) | 92 | 0.011 | * | 92 | 0.072 | – | 92 | 0.661 | – |
| Transverse plane parameters | |||||||||
| Thoracic gibbosity (°) | 73 | 0.208 | – | 74 | 0.450 | – | 69 | 0.101 | – |
| Thoracic height (%) | 73 | 0.051 | – | 74 | 0.820 | – | 69 | 0.080 | – |
| Thoracolumbar gibbosity (°) | 61 | 0.003 | ** | 66 | 0.811 | – | 56 | 0.001 | ** |
| Thoracolumbar height (%) | 61 | 0.014 | * | 66 | 0.030 | * | 56 | 0.567 | – |
| Paraspinal lumbar prominence (°) | 73 | 0.048 | * | 67 | 0.171 | – | 67 | 0.368 | – |
| Lumbar height (%) | 73 | 0.822 | – | 67 | 0.134 | – | 67 | 0.076 | – |
On the frontal plane, we apprised ourselves of a statistically significant difference between C7 lateral deviation in the “folding” position when compared with the two usual postures.
On the sagittal plane, the “folding” position entailed significant modifications. We apprised ourselves of a significant variation of the C7 plumb and the lumbar arrow in comparison with the two usual postures, a significant variation of the lordotic angle relative to the “clavical” position and a significant variation of the kyphotic angle relative to the “straight out” position. Moreover, the “clavical” position entailed a significant variation of the thoracic arrow and the kyphotic angle relative to the “straight out” position.
On the transverse plane, identification and measurement of the thoracolumbar gibbosity present a statistically significant difference of the “folding” in comparison with the “clavical” and “straight out” positions. A difference has also been noted between the “folding” and “clavical” positions relative to measurement of the lumbar prominence.
1.5
Discussion
The results highlight the fact that the “folding” position that we are proposing affords a quality of inter-observer reproducibility similar to the two usual postures, and that it provides higher thoracic gibbosity values than those calculated in the other two positions.
In the folding position, the flexing of the arms imposes a rotational or “back swing” movement of the scapula, which limits its interposition between the ribs and the skin. The statistically significant increase of thoracic gibbosity values in the “folding” position in comparison with those observed in the other two positions lead us to suppose that the interposition of the scapula (see, for example, the “winged scapula” phenomena), which is more pronounced in the two postures usually proposed, can diminish perception of costal dissymmetry through systems of back surface topography, in an upright position. However, changes in arm positioning can modify radiologic sagittal parameters, particularly as regards the cervical arrow . Our results are in concordance with these studies as we observe similar modifications induced by the “clavical” and “folding” positions in which the hands are raised at the level of the scapular girdle. The thoracic curve significantly diminishes in the “clavical” position in comparison with the “straight out” position, and this is highly likely to augment the impression of “flat back” in scoliosis. Conversely, the “folding” position, which facilitates highlighting of the gibbosities on the transverse plane, also appears to augment spinal kyphosis and lordosis in comparison with the kyphosis and lordosis observed in the two more usual postures.
Several positions have been studied in view of finding the best compromise between the natural posture of the arm along the body and postures modifying the positioning of the arm yet allowing for high-quality radiological measurements . Our results show that inter-observer reproducibility with regard to the measurements appears to be of high-enough quality in the three positions having been studied. This type of inter-observer reproducibility quality presents an interest in current practice insofar as the examinations and their analyses are not systematically carried out by the same person. And it is quite possible that the reproducibility is associated with the painstaking care with which the requested postures have been described. As is the case in radiography, this observation underscores the interest of recalling the carefulness with which the different stances should be explained in everyday practice, thereby ensuring respect for the validated conditions of measurement .
On an overall basis, our TEM are comparable to those observed in other studies of back surface topography, regardless of the posture or the recording technique chosen. All in all, they remain a few mm lower for the plumb lines and a few degrees lower for the angles . For example, the C7 sagittal arrow appears to be the parameter offering the most variation. Its variation remains lower than 10 mm in our study as well as in the preceding series.
On the transverse plane, the reproducibility qualities of the gibbosities were limited to “fair” for the worst of the three postures. However, analysis of the amplitudes of variations of the gibbosities and the paraspinal lumbar prominence showed that they remain lower than the threshold of clinical relevance, that is to say lower than two degrees . Even though the software helps to objectify the highest segments of the “gibbosity” deformities, measurement reproducibility quality was certainly impacted by the fact that the operator had to define the levels of interest. In accordance with the observations of SOSORT , we think that these measurements should be calculated automatically.
In the “straight out” posture, which is considered to be the closest of the three to the natural stance, the arms rest on a support. In this position, the parameters evaluating the upper part of the trunk (lateral C7 deviation and sagittal C7 arrow) present higher reproducibility than the other two postures, in which the hands rest on the upper part of the trunk. This finding would suggest that in cases where analysis of overall sagittal balance is primordial, as in the study of postural lumbago , it would be interesting when taking measurements to pay particular attention to the “straight out” position.
1.6
Conclusion
This study reveals the reproducibility of the “folding” position and thereby favors exploration of thoracic gibbosities or “humps” while highlighting the complementarity of three postures in evaluation of scoliosis deformities by means of back surface topography tools.
Disclosure of interest
Tiana Randriaminahisoa presently holds, in the framework of a CIFRE study and thesis preparation grant, a position of engineer in the AXS medical companies, which are commercializing the Biomod L system. The other authors have no conflict of interest.
2
Version française
2.1
Introduction
La scoliose idiopathique est une déformation tridimensionnelle du rachis. Sa fréquence est estimée à environ 3 % de la population . En pratique clinique, la présence d’une gibbosité peut permettre de diagnostiquer une scoliose . La détection d’une gibbosité est réalisée à l’aide d’un scoliomètre et du test d’Adam. Ce test impose une antéflexion du rachis pour mesurer la gibbosité et de laisser pendre verticalement les membres supérieurs pour dégager les gibbosités thoraciques.
En pratique clinique, le suivi radiologique influe beaucoup sur les décisions thérapeutiques en raison de sa reproductibilité . Cependant, l’exposition aux rayons X n’est pas dénuée de risques, spécialement pour les jeunes filles scoliotiques . De nombreux systèmes de topographie de surface du dos ont donc été développés dans l’objectif de restreindre le nombre de radiographies effectuées. Dans un premier temps, les systèmes de topographie de surface du dos ont été développés pour remplacer les radiographies dans le dépistage de masse des scolioses par un outil non ionisant et plus facilement ambulatoire . Dans un deuxième temps, l’objectif de ces systèmes a été de limiter le nombre de radiographies effectuées au cours du suivi thérapeutique . Un obstacle à ce développement s’est révélé être un manque de corrélation suffisante entre les mesures surfaciques faites dans les positions habituelles et les mesures de l’angle de Cobb faites sur les radiographies . Ainsi bien qu’il soit encore incertain que ces systèmes puissent réellement permettre de réduire le nombre de radiographies effectuées , ils ambitionnent de s’imposer dans la prise en charge moderne des jeunes scoliotiques.
Afin de faciliter la comparaison avec les paramètres radiographiques, les acquisitions de la topographie de surface du dos doivent être réalisées dans des positions proches des positions radiologiques de références. Il s’agit principalement des positions dites position « clavicule » et position « en appui » .
L’objectif de ce travail était d’analyser la reproductibilité d’une posture debout dite « enroulée » permettant de visualiser les gibbosités thoraciques grâce à un enroulement antérieur des bras et de comparer l’effet de cette position sur les paramètres surfaciques habituellement mesurés dans les deux positions radiologiques.
2.2
Matériels et méthodes
2.2.1
Sujets
Il s’agit d’une étude prospective menée au sein de l’unité de médecine orthopédique du CHU de Bordeaux. Conformément à la déclaration d’Helsinki, tous les sujets ont été recrutés sur la base d’un consentement volontaire propre. Les critères d’inclusion reposaient sur des critères radiologiques correspondant à un angle de Cobb d’au moins 15° sur des grands clichés du rachis entier de face après correction éventuelle d’une inégalité de longueur des membres inférieurs. Les critères d’exclusion étaient la présence d’anomalies cliniques ou radiologiques faisant évoquer la possibilité d’une scoliose symptomatique.
Une analyse topographique de la surface du dos a été réalisée sur 46 patients (40 filles et 6 garçons). La caractérisation des scolioses montrait : 36 (78,3 %) doubles courbures, 9 (19,6 %) simples courbures, et 1 (2,1 %) triple courbures. La moyenne des angles de Cobb maximaux était égale à 26,8 ± 10 degrés.
2.2.2
Instrumentation
Les mesures ont été réalisées à l’aide du système BIOMOD TM L (AXS MEDICAL SAS, Mérignac, France). Cet appareil est un dispositif médical autorisé en pratique clinique. Il est constitué d’une colonne mobile d’acquisition de la surface du dos et d’un logiciel de traitement des mesures. La colonne d’acquisition comprend une caméra haute définition, des inclinomètres, et un projecteur de lumière structurée. La déformation des images projetées permet de remonter au relief 3D texturé de la surface du dos. Le temps d’acquisition était égal à 40 ms.
Le relief 3D était traité sur un logiciel dédié afin d’obtenir des mesures cliniques. Une détection automatique était effectuée sur des repères anatomiques marqués par l’opérateur. Ces repères incluaient la ligne des épineuses (en partant de C7 jusqu’au sommet du pli inter-fessier) ainsi que les fossettes de Michaelis. Les mesures étaient alors effectuées dans un système de référence lié à ce repérage, et évaluées dans 3 plans d’analyse : plan frontal, plan sagittal, plan transverse. Ils étaient définis comme suit : le plan frontal était le plan de la verticale et passant par les fossettes de Michaelis ; le plan sagittal était le plan de la verticale perpendiculaire au plan frontal ; le plan transverse était le plan horizontal. Le sommet du pli inter-fessier défini par l’examinateur était l’origine du repère formé par l’intersection de ces 3 plans ( Fig. 1 ).