Insertional Achilles Tendinopathy
Mark E. Easley
Matthew J. DeOrio
DEFINITION
Insertional Achilles tendinopathy is posterior heel pain at the insertion of the Achilles tendon.
The clinical diagnosis is acute and chronic pathology of the Achilles tendon insertion and its surrounding tissues.
ANATOMY
The Achilles tendon, the condensation of the gastrocnemius and soleus tendons, inserts on the posterior calcaneal tuberosity.
The insertion is not only posterior but also on the medial and lateral aspects of the calcaneus.
A dorsal posterior calcaneal prominence is most obvious on a lateral radiograph. The Achilles tendon inserts distal to this, directly posterior on the calcaneus.
Between the distal Achilles tendon and the dorsal posterior calcaneal prominence, immediately proximal to the Achilles insertion, is the retrocalcaneal bursa.
A pre-Achilles bursa is superficial to the distal Achilles tendon.
PATHOGENESIS
Although not fully understood, repetitive microtrauma to the Achilles tendon insertion is thought to be the cause.
Most likely, some initial injury occurs, followed by multiple minor reinjuries that lead to chronic symptoms.
In the acute phase, the process may have some inflammatory characteristics; however, the chronic process is degenerative, with a relative paucity of inflammatory tissue.
Without histologic confirmation, the diagnosis of Achilles tendinitis or tendinosis cannot be made; therefore, the pathologic process at the Achilles tendon insertion is viewed as “tendinopathy” without tissue confirmation.
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient may recall an inciting event but typically reports chronic activity-related aching or even sharp pain at the posterior heel.
In addition, the patient notes a progressively enlarging prominence on the posterior heel.
This ache is usually accompanied by exquisite tenderness directly posteriorly on the calcaneus, at the Achilles tendon insertion, with manual pressure, on contact from the shoe’s heel counter, or when the posterior heel is rested on a hard surface.
Putting the Achilles tendon on stretch aggravates the symptoms, such as when the patient walks uphill.
Physical examination reveals the following:
A prominence is evident on the posterior heel at the Achilles tendon insertion (FIG 1).
Tenderness is felt directly on the posterior calcaneal prominence.
No tenderness is found in the Achilles tendon proximal to its insertion on the calcaneus.
Thompson test is negative.
IMAGING AND OTHER DIAGNOSTIC STUDIES
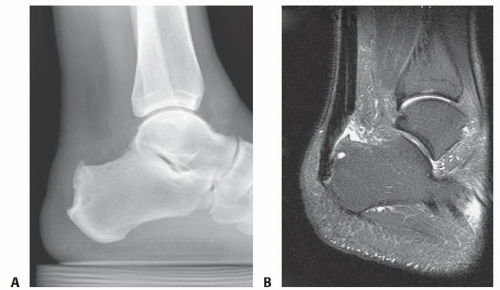
A lateral weight-bearing radiograph of the foot often demonstrates irregularities and calcifications at the Achilles tendon insertion on the posterior calcaneus (FIG 2A).
Although unnecessary to make the diagnosis, magnetic resonance imaging (MRI) defines the extent of tendon involvement at the insertion and the presence of retrocalcaneal and perhaps even pre-Achilles bursitis (FIG 2B).
DIFFERENTIAL DIAGNOSIS
Pre-Achilles bursitis
Retrocalcaneal bursitis
Calcaneal stress fracture
Haglund deformity (prominent dorsal posterior calcaneal tuberosity impinging on the Achilles tendon)
Calcaneal stress fracture
Posterior ankle impingement
Plantar fasciitis
Noninsertional Achilles tendinopathy
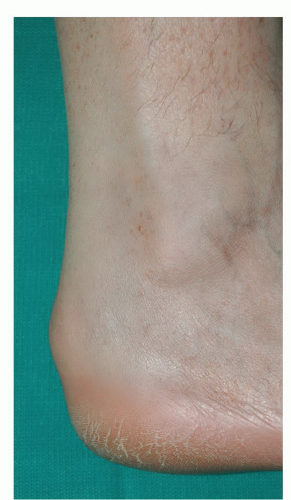 FIG 1 • Example of posterior calcaneal prominence characteristic of insertional Achilles tendinopathy. |
NONOPERATIVE MANAGEMENT
Activity modification (avoidance of activities that place the Achilles tendon on stretch)
Nonsteroidal anti-inflammatory agents
Heel lift or a shoe with a heel to unload the Achilles tendon
Open-backed shoe or a shoe with a soft heel counter
Physical therapy
Focus on eccentric strengthening exercises
In our experience, the common practice of aggressive Achilles stretching must be avoided as it will aggravate the symptoms.
Modalities: ultrasound, iontophoresis
Extracorporeal shockwave therapy may have some benefit but is largely unproven.
Corticosteroid injection may lead to Achilles rupture and is contraindicated unless the process is isolated to retrocalcaneal bursitis, in which case, a judicious injection of only the retrocalcaneal bursa can be performed.
SURGICAL MANAGEMENT
The primary surgical indication is nonoperative management.
Up to 50% of insertional Achilles tendinopathy can be successfully managed without surgery, even when there is a large posterior calcaneal prominence.
Insertional Achilles tendinopathy with central calcific tendinosis may be less amenable to nonoperative management.
Preoperative Planning
Preoperative medical clearance
Even in healthy patients, the thin skin on the posterior heel is at risk. Carefully inspect skin to be sure that the patient is a reasonable candidate for a posterior approach to the Achilles tendon insertion.
With extensive Achilles tendon degeneration (confirmed with preoperative MRI), an augmentation of the insertion may be warranted. Therefore, preoperative planning should include the anticipation that the flexor hallucis longus (FHL) tendon may need to be harvested and transferred to the posterior calcaneus. The FHL tendon lies immediately deep to the deep compartment fascia that is anterior to the Achilles tendon and can readily be harvested through the same approach.
As a rough estimate, we perform an FHL augmentation in less than 10% of cases but routinely have our preferred anchoring system available should the transfer be warranted.
We educate all of our patients undergoing surgical management for insertional Achilles tendinopathy that, based on our intraoperative findings, an FHL tendon transfer may be necessary.
The recovery following surgical management for insertional Achilles tendinopathy is prolonged and may take a full year before the patient returns to full activity. We educate our patients that the recovery is not rapid.
Positioning
The patient is placed prone on the operating table.
We routinely inflate the thigh tourniquet with the patient supine on the stretcher, then flip the patient to the prone position on the operating room table. This facilitates proper tourniquet position and avoids stressing the patient’s lumbar spine, which may be stressed when placing the tourniquet with the patient in the prone position.
The chest and pelvis are well padded.
The brachial plexuses and ulnar nerves at the elbows are protected and relaxed.
The genitalia are protected.
TECHNIQUES
▪ Exposure and Reflection of the Achilles Tendon Insertion
Approach
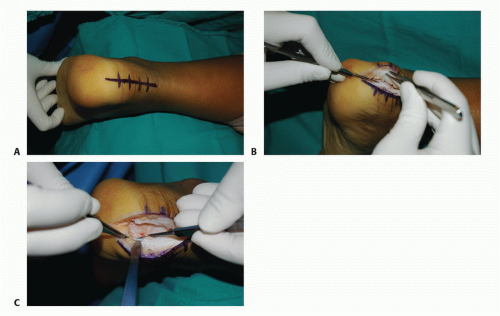
A central approach is undertaken, directly over Achilles tendon and posterior calcaneus (TECH FIG 1A).
The scalpel is moved through skin and into central portion of distal Achilles tendon. Deep incision is continued distally, directly to bone.
The goal is to avoid unnecessary delamination of the soft tissues and to elevate full-thickness flaps.
We then elevate medial and lateral slips of Achilles tendon from the calcaneus (TECH FIG 1B,C).
More than half of the Achilles tendon insertion can be elevated without compromising the integrity of the insertion. One study suggests that up to 75% can be released.
We elevate the Achilles tendon until all the diseased portion of tendon can be excised.
Another study suggests that the entire insertion of the Achilles tendon should be routinely elevated and excised to ensure that all diseased tissue is removed. Reattachment is facilitated by a proximal Achilles tendon lengthening that also serves to unload the Achilles tendon.
We do not routinely elevate the entire Achilles tendon, but should one or both of the Achilles tendon slips become detached, we have uniformly been able to reattach the tendon to the calcaneus with a successful outcome.
▪ Débridement of the Diseased Portion of Achilles Tendon
The diseased portion of tendon is gradually pared from the Achilles insertion, until only healthy fibers remain (TECH FIG 2A-C).
Healthy Achilles fibers have an organized, longitudinal pattern.
Degenerated Achilles tendon substance is unorganized and may be likened to crab meat (TECH FIG 2D,E).
Calcific tendinosis may be present, and all calcifications within the residual Achilles tendon must be excised (TECH FIG 2F).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree