Physical examination is crucial to correctly determine the level of SCI. Whereas bony vertebral column injury is diagnosed with radiographs (see
Chapter 28), SCI is diagnosed with physical examination and supplemented with magnetic resonance imaging. As stated in the preceding text, all patients with a suspected SCI should be immobilized with a rigid cervical collar and spinal backboard. Rigid longboards should be removed as soon as possible and hard surfaces should be padded during resuscitation and in the operating room. Keep in mind that although a patient may have ambulated at the scene of the accident, it does not mean that serious cord or potential cord injury is not present. Patients may have either a spinal column injury or an SCI and each is neither inclusive nor exclusive of the other.
As with all trauma patients, ATLS protocol should be followed. The patient’s airway must be secured, breathing must be adequate, and circulation intact. Full spinal immobilization is continued to prevent any further injury to the cord. Next, a thorough neurologic evaluation should be done. This evaluation should include a sensory and motor examination, a mental status examination, a reflex examination, and cranial nerve testing. The
mental status can quickly and efficiently be evaluated with the Glasgow Coma Scale (GCS). The motor score is the patient’s best movement of the upper extremity. If the patient is unable to move any extremity, but is following a command such as “stick out your tongue,” the GCS would be incomplete or guarded with further more exact description of the deficit needed. The vertebral column is palpated feeling for deformities and step-offs. If the patient is alert, tenderness at a particular segment can be indicative of injury. Each extremity should be evaluated individually and each neurologic level assessed. The motor strength should be recorded according to the American Spinal Injury Association/International Medical Society of Paraplegia (ASIA/IMSOP) scoring system. The scale is from 0 to 5. Normal strength is given 5 points whereas some movement against resistance is given 4. Only within the 4 level of strength should a + or – be used to indicate near-normal strength or only slightly more resistance than gravity, respectively. Movement against gravity but not resistance receives 3 points and movement with gravity being eliminated is given 2. Finally, being able to feel muscle twitching is given 1 point and no movement is given 0 points.
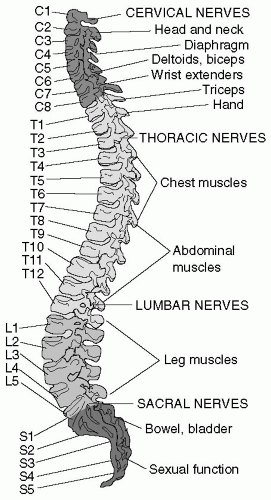
13 Some key muscle groups can be quickly tested to determine the level of injury; C5 elbow flexors, C6 wrist extensors, C7 elbow extensors, C8 finger extensors, T1 small finger abductors, L2 hip flexors, L3 knee extensors, L4 ankle dorsiflexion, L5 long toe extensors, and S1 ankle plantar flexors (see
Table 1).
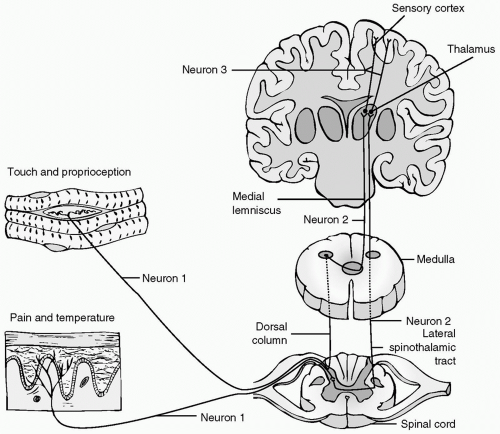
14 Sensory testing is somewhat subjective. The scale is 0 to 2 with intact sensation being 2, decreased or hyperesthetic being 1 and no sensation being 0. The location of the dermatomes is shown in
Fig. 3. A rectal examination is also a crucial part in evaluating the integrity of the spinal cord. The examination is done for two reasons. The first is to determine motor function of the sphincter muscle. The second is to determine perianal sensation. Presence of either of these demonstrates that there is sacral sparing, which indicates
that there is at least some integrity of the spinal cord because the sacral fibers travel along the periphery of the cord.