CHAPTER 21 Injuries to the Triangular Fibrocartilage Complex
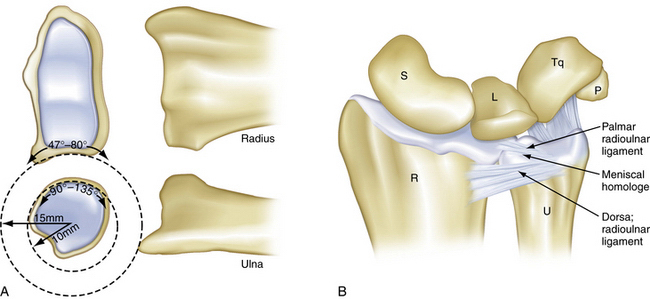
In 1981, Palmer and Werner used the term triangular fibrocartilage complex (TFCC) to describe the set of related structures at the distal ulnar aspect of the wrist.1 The TFCC physically separates the distal radioulnar joint (DRUJ) from the radiocarpal joint. The TFCC must be simultaneously robust and flexible. It must have the strength to transmit 20% of the load of the carpus to the ulna and to stabilize the DRUJ and ulnar carpus in conjunction with the bony architecture of the sigmoid notch. It is must also be supple enough to accommodate the significant, complex motion that occurs during forearm rotation. The motion of the DRUJ is a combination of approximately 150 degrees of rotation and sliding. This occurs because the radius of curvature is 50% larger on the radial side of the DRUJ (15 versus 10 mm) (Fig. 21-1A). The axis of rotation passes through the fovea of the ulnar head, which is a major attachment site for the TFCC.
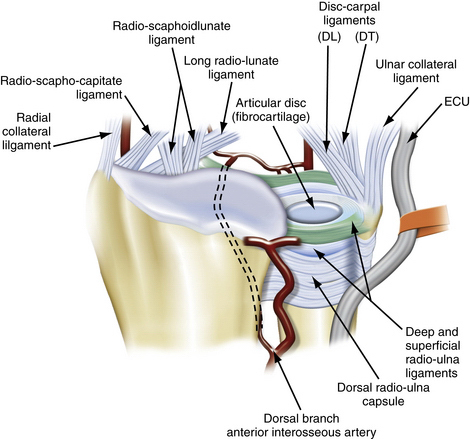
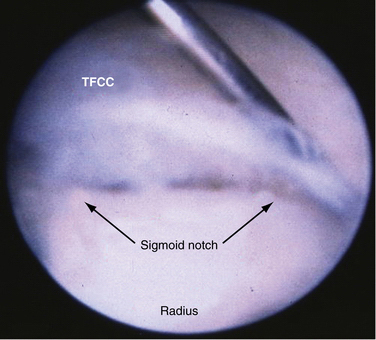
The five structures that comprise the TFCC are the articular disk, the distal radioulnar ligaments (palmar and dorsal), the meniscal homologue, and the extensor carpi ulnaris (ECU) subsheath, which is confluent with the (ulnocarpal collateral ligament (see Fig. 21-1B).2 The central portion of the complex consists of an articular disk called the triangular fibrocartilage (TFC). The disk is composed predominately of type II collagen, which is consistent with its role in distributing compressive forces. It lies in the axial plane and structurally represents an extension of the articular surface of the distal radius. Dorsally and palmarly, the TFC is surrounded by the radioulnar ligaments, which are transverse bands that derive their broad origin from the sigmoid notch of the distal radius and insert on the base of the ulnar styloid. The ulnotriquetral and ulnolunate ligaments form the palmar border of the TFCC, and, although Palmer and Werner did not include them in their original description of the TFCC, they serve an important role in the stability of the ulnar side of the wrist.
The blood supply of TFCC enters from the periphery (Fig. 21-2). Thiru and colleagues evaluated cadaveric specimens and identified three main branches of the TFCC.3 The ulnar periphery of the TFCC has the richest blood supply and, consequently, the greatest potential for healing. It is fed predominantly via the dorsal and palmar radiocarpal branches of the ulnar artery. Dorsal and palmar branches of the anterior interosseous artery supply the more radial part of the complex.
CLASSIFICATION OF TRIANGULAR FIBROCARTILAGE COMPLEX INJURIES
Palmer’s original classification divides injuries of the TFCC into degenerative and acute tears (Box 21-1).4 The classification is anatomically subdivided into radial, central, and ulnar tears. This classification bears consideration, because the vascular anatomy dictates the healing potential and therefore the treatment and prognosis for TFCC tears, similarly to tears of the knee’s meniscus.
Box 21-1 Classification of Triangular Fibrocartilage Complex Injury
From Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14:594.
Palmer class 1 injuries are acute, traumatic injuries. They are subdivided into four types, based on the site of injury (Fig. 21-3):
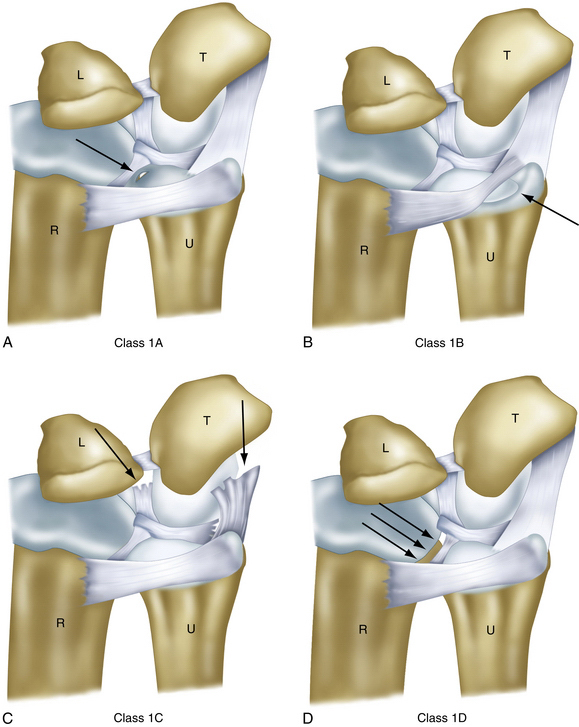
FIGURE 21-3 Four types of class 1 lesions of the triangular fibrocartilage complex. L, lunate; R, radius; T, triquetrum; U, ulna.
(Modified from Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14:594-606.)
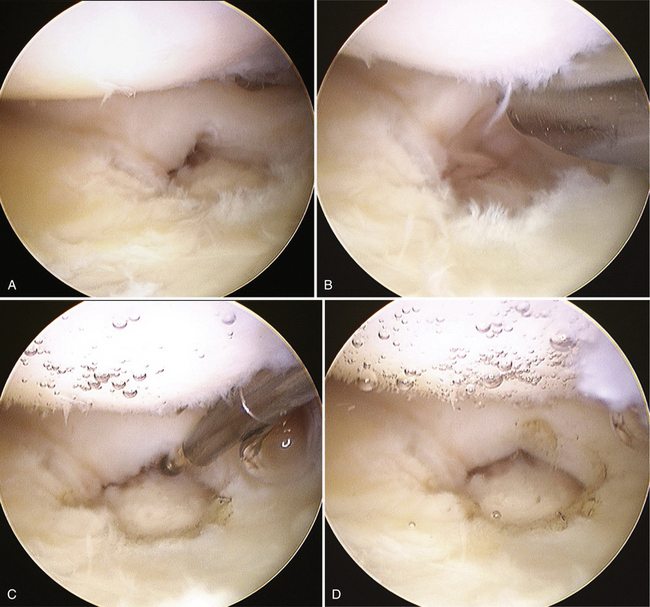
FIGURE 21-4 Arthroscopic treatment of type 1A lesions involving the central avascular portion requires débridement of the central tear to remove any flaps that may impede movement. A, Lesion in the central portion of the triangular fibrocartilage complex (TFCC). B, Central tear of the TFCC is débrided using a 2.5-mm arthroscopic shaver. C, Ablation at the edge of the lesion using a small joint radiofrequency probe. D, Smooth surface of the lesion after débridement.
Degenerative TFCC lesions (Palmer class 2) all involve the central portion and are staged from A to E, depending on the presence or absence of a TFCC perforation, lunate and ulnar chondromalacia, a lunotriquetral ligament perforation, or degenerative radiocarpal arthritis. These degenerative lesions usually arise from ulnar abutment. Class 2 lesions usually are not amenable to surgical repair and are treated with débridement.
TFCC tears can be further subdivided by their acuteness. The chronicity has prognostic implications, and addressing tears in the acute phase usually provides better results.5–7
The incidence of asymptomatic TFCC tears increases with age. Wright and coworkers, in a study of 62 wrists from cadavers of individuals whose average age at death was 78 years and found a tear of the TFCC in 33 wrists (11 lesions were central, and 21 were vertical radial).9–11 Mikic observed an age-related correlation with disk perforation in his cadaveric study of 180 wrists from fetuses to the elderly. He found the prevalence of perforations to be zero among patients younger than 20 years; 7.6% among those in the third decade; 18.1% in the fourth decade; 40.0% in the fifth decade; 42.8% in the sixth decade, and 53.1% (26 wrists) among patients older than 60 years.9 These degenerative changes correlated with magnetic resonance imaging (MRI) findings from healthy volunteers.12 This illustrates the necessity of correlating imaging with history and examination findings in these patients.
PATIENT EVALUATION
History, Signs, and Symptoms
Ulnar-sided wrist pain has been referred to as the low back pain of the hand surgeon. The multitude of structures and diagnoses that can contribute to a patient’s symptoms are often subtle and require precise physical examination and correlation with history and imaging. Causes of ulnar-sided wrist pain are listed in Box 21-2.
Box 21-2 Common Causes of Ulnar-Sided Wrist Pain
DRUJ, distal radioulnar joint; ECU, extensor carpi ulnaris; TFCC, triangular fibrocartilage complex.
Chronic attritional injuries and degenerative changes of the ulnocarpal joint, including the TFCC, result from repetitive overloading. Ulnar deviation of the wrist, along with forearm supination and power grasp, increase the damage from axial loads. Patients with acquired ulnar positive variance, discussed in greater detail later, are at higher risk for degenerative changes and recurrent injury from minor trauma.
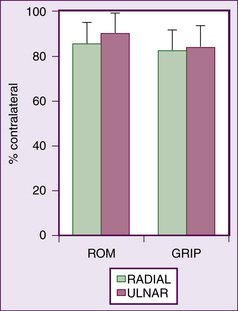
TFCC tears have been associated with distal radius fractures on imaging and direct arthroscopy. The incidence ranges between 13% and 60%.13–17 The literature does not clearly indicate, in the absence of frank DRUJ instability, which tears should be fixed and by which methods, in part because it is unclear how many of these tears become symptomatic. It is likely that many of these tears are effectively treated by treatment of the concomitant fracture.14 Nevertheless, several authors have endorsed the use of arthroscopy in the setting of distal radius fracture fixation to identify and treat concomitant soft tissue injuries. Varitimidis and associates reported that 60% of their patients with distal radius fracture had TFCC tears, half of which were ulnar sided.17 All TFCC tears underwent débridement; 20% (2 of 12) had arthroscopic repair, and 1 patient required open repair. The arthroscopic group demonstrated improved ROM and Mayo wrist scores, compared with those treated with traditional external fixation. In 2003, Ruch and colleagues demonstrated good or excellent results with acute repair of the TFCC at the time of distal radius operative treatment in 56 patients, with only 2 patients with transient ulnar dorsal sensory irritation, but they lacked a control group.18
Lindau and coworkers reported that 10 of 11 patients with a documented complete peripheral TFCC tear associated with a distal radius fracture exhibited DRUJ instability at a 1-year follow-up examination, compared with 22% of those with no peripheral tear or only a partial tear.19 This instability was correlated with worse clinical outcome.
Physical Examination
Patients with acute TFCC injuries frequently present with ulnar-sided wrist swelling that may reverse the normal convex shape of the ulnar wrist border. The soft, ballotable region between the ulnar styloid and the triquetrum can frequently be point tender (Fig. 21-7). Clicking can often be elicited with passive and active circumduction of the wrist. Specialized tests to distinguish TFCC injuries from other ulnar wrist injuries include the TFCC compression test, the ulnar impaction test, and the piano key test. Significant pain from axial loading of the TFCC, in conjunction with ulnar deviation, is a positive compression test. Similarly, pain with the combination of wrist hyperextension and the previous maneuvers indicates a positive ulnar impaction test.20 Comparison of any dorsal-volar plane instability of the DRUJ with the normal contralateral side is the piano key test (Fig. 21-8). This should be performed in neutral position, in supination, and in pronation. The DRUJ typically has the most anteroposterior translation in the neutral position. Volar subluxation of the distal ulna with wrist supination can be appreciated by dimpling of the skin of the dorsal ulnar border (Fig. 21-9). Lunotriquetral ballottement tests ligament stability (Fig. 21-10). Pisotriquetral manipulation should be performed to rule out arthrosis of this joint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree