Injection of medications in proximity to nerves, muscles, and skeletal structures (bursae, joints, and tendons) provides an important intervention in the management of pain and dysfunction. These medications can provide analgesia, reduce inflammation of the affected structure, and promote tissue healing directly and indirectly through facilitation of rehabilitation. Commonly, local anesthetics are used for immediate anesthesia and analgesia, corticosteroids are used to control inflammation, radiopaque contrast is used to assist any fluoroscopic confirmation, and vasoconstrictors are used to prolong local anesthetic effects or warn of intravascular injection. Injection techniques constitute both diagnostic and therapeutic modalities in many settings. As in all patient care, the origin of pain or dysfunction involves careful history taking and a complete physical examination. The details of these techniques are addressed generally in
Chapter 2 with a specific focus in
Chapters 32,
33,
35,
49, and
68. This chapter first outlines the historical development and general principles of proper procedural techniques, including indications and contraindications. Significant side effects or complications and commonly used medications are reviewed. General techniques for nerve blocks and specific nerve blocks are then discussed.
HISTORICAL
Since antiquity, sharp objects have been used to inject various concoctions into the body as remedies for pain and dysfunction (
1). The tools of modern-day injection procedures include the hollow needle developed by Rynd in 1845 (
2) and the syringe developed by Pravaz in 1853 (
3) and Wood in 1855 (
4). Medications to inject for anesthesia were developed in the late 1800s, with extensive use of cocaine as a topical analgesic (
5) and as an injected analgesic (
6). The application of these devices and medications to achieve local anesthesia for relief of pain was described by Corning in 1894 (
7). Historical information on neural blockade has been reviewed in detail by Brown and Fink (
1).
Since the early 1900s, procaine had been injected into the synovium of inflamed joints for temporary relief of pain. In 1949, Hench (
8) introduced systemic corticosteroids to suppress the inflammatory changes in rheumatoid arthritis. However, large doses of corticosteroids given systemically resulted in complications. In 1951, Hollander (
9) introduced and reported on low-dose local (intraarticular and periarticular) injections of hydrocortisone acetate to control pain and inflammation caused by trauma and inflammatory joint disease. Historical information on intraarticular injection has been reviewed in detail by Hollander and colleagues (
10). Tender points in the muscle were identified in the 1800s by multiple investigators (
11,
12). Kraus in 1937 (
13) and Travell in 1942 (
14) introduced the treatment of myofascial pain by direct trigger point injection and use of vapocoolant spray and emphasized the importance of exercise in the treatment of patients with trigger point mediated pain. Historical information on myofascial pain has been reviewed in detail by Simons (
11).
GENERAL
The general principles for use of neural blockade were described in detail by Bonica in 1953 (
15). Injections of local anesthetic agents have been shown to be effective in managing patients with acute and chronic pain. The mechanism of action is the blockade of nociceptive input along the pathway of transmission (
16). Intraarticular and periarticular injections of corticosteroids have been shown to reduce inflammation and pain as well as to facilitate mobility and function (
17). Unfortunately, injection of medication is often used in isolation for the management of many pain problems. It is important to use injections as one component in a vast armamentarium of techniques that are often best used in concert with each other. An injection unaccompanied by physical therapy, exercise, stretching, behavior modification, and optimization of coexisting psychological disorders is often incomplete in alleviating pain or restoring function. This is best demonstrated by the “block clinics,” which were highly popular in the 1930s and 1940s but have since been superseded by multidisciplinary pain clinics. Injection procedures should be performed within the context of comprehensive rehabilitation.
Knowledge and Training
Using injection procedures requires sufficient knowledge to understand the diagnosis and treatment of pain syndromes. Limitations, complications, advantages, and disadvantages of each procedure and alternative treatments must be understood when choosing the best therapy or combination of therapies. The practitioner must be highly skilled in injection techniques based on education, training, and experience. This requires a
thorough knowledge of the anatomic basis of the procedure and the characteristics of the injectable medication, including expected side effects of the procedure as well as potential complications and their prevention and prompt treatment (
16).
Contraindications
Injection procedures encompass a wide variety of techniques, including epidural, caudal, nerve, motor point, joint, and muscle. Although relative advantages and disadvantages exist, certain conditions comprise contraindications to perform any injection technique. Certain medical conditions also may preclude an injection. For example, a patient with severe lung disease should not have a rib block with its attendant risk for pneumothorax.
Absolute Contraindications
Absolute contraindications for injection procedures include patient refusal, localized infection, dermatologic conditions that preclude adequate skin preparation, existence of a tumor at the injection site, history of allergy to local anesthetic agents, the presence of severe hypovolemia, gross coagulation defects, increased intracranial pressure (for epidural procedures), and septicemia.
Relative Contraindications
Among relative contraindications are the lack of education, training, and skill on the physician’s part. In addition, relative contraindications are the patient’s minor coagulation abnormalities or concurrent use of certain anticoagulants such as minidose heparin. Diabetes is a relative contraindication for injections with corticosteroids because of the possibility of hyperglycemia, glycosuria, electrolyte imbalance, and increased risk for infection.
Screening for Contraindications
Early in the interview process, the patient should be asked specific questions about conditions that would preclude the injection procedure. Firstly, anticoagulation issues must be addressed, and the patient should have been able to discontinue antiplatelet therapy (e.g., clopidogrel) or anticoagulation (e.g., unfractionated heparin or warfarin) for sufficient duration. The practitioners should be aware of current guidelines regarding anticoagulation and neuraxial procedures and have developed a standard practice ahead of time in regards to anticoagulation and injections. Secondly, the patient should have transportation and a responsible adult who can care for the patient after the procedure, especially if the injection has the potential to cause weakness or sedation. Thirdly, the patient should be appropriately fasted to reduce the chance of aspiration, particularly if he or she is likely to need sedation. Any allergies to the expected injection medications or to material such as latex should be documented and alternatives be used for the procedure.
Communication
Communication with the patient is essential at all steps involved in patient care, including injection. Providing the patient with a complete explanation of the procedure will result in the individual having increased confidence and reduced anxiety. During the procedure, the physician should continually inform and reassure the patient as to the progress of the procedure.
Informed Consent
Although state laws vary in terms of the documentation required, informed consent involves providing enough information about the injection procedure so that the patient can intelligently decide whether or not to proceed (without external coercion or manipulation). This involves a thorough discussion of the procedure with the patient, including the possible benefits, alternative treatments, common side effects, and risks of complications. The patient should be given the opportunity to ask questions about details of the injection. The patient should not receive medications that could significantly impair responses or judgment before the consent is given. Depending on state regulations, the patient may or may not be required to sign an informed consent form. Significant complications of injection procedures are provided in
Table 67-1.
Universal Precautions
Universal precautions are required for all injection techniques to reduce the incidence of transmission of infectious agents (
18). These include the use of gloves and protective eye wear. Possible transmission of blood-borne pathogens during medical procedures is a common concern among patients and health care workers, owing to its potentially devastating consequences. Although this concern has largely focused on the human immunodeficiency virus (HIV), other agents, particularly hepatitis B, C, and G viruses, are of significantly greater risk. The data show that the risk to health care workers from patients is far greater than the risk to patients from health care workers (
19). It is important that proper sharps disposal containers are maintained in all areas where needles are used. Hollow needle sticks pose the greatest risk for occupational transmission, with studies following health care workers after
such exposures finding the following seroconversion rates: hepatitis B, 5% to 37%; hepatitis C, 3% to 10%; and HIV, 0.2% to 0.8% (
19,
20,
21,
22,
23). Research shows that recapping a needle increases the risk for needle stick, hence needles should either be laid down in the sterile field or disposed uncapped in an appropriate container.
Positioning
Optimal results of any injection depend on proper positioning of the patient before, during, and after the injection procedure. The proper position should facilitate access to the injection site, with the patient and provider being as comfortable as possible. Bony prominences should be cushioned where needed to avoid discomfort from pressure. When possible, the recumbent position is used because it is usually the most comfortable for the patient. It also minimizes the incidence of orthostatic hypotension caused by vasovagal reaction during the procedure. Positioning to avoid ergonomic stress on the patient and physician is essential. Consideration should be made for access to special equipment such as a fluoroscopic C-arm or ultrasound machine.
Skin Preparation
Strict aseptic preparation is required in all injection procedures, as well as intact skin at the site of injection. Preparation of the injection site is undertaken in a standard aseptic fashion over an area large enough to allow palpation of landmarks and any potential extension of the injection site, and sterile technique is used throughout the procedure to minimize the risks. Most injection techniques described in this chapter do not require full surgical draping; however, the phrase “sterile technique is used throughout the procedure” indicates an increased risk for major infectious complications, including epidural abscess, meningitis, and adhesive arachnoiditis.
The injection site is prepared with an antiseptic to reduce cutaneous microorganisms to the lowest level. Commonly used agents include chlorhexidine (Hibiclens, Zeneca Pharmaceuticals, Wilmington, DE), iodophors (Betadine, Purdue Frederick, Norwalk, CT), and alcohol (
24). It is important for the clinician to wait about 2 minutes after the application of any of the above antiseptics to obtain maximal reduction in cutaneous bacteria. It is rarely justified to remove hair from the skin for an injection procedure (
25). In addition to skin preparation, some procedures such as intradiscal procedures or prolonged catheter trial probably warrant systemic intravenous antibiotics prior to needle insertion (
26). Many providers will wear a surgeon’s cap, filtration mask, and full surgical gown, although any differences in the rate of infections have been difficult to demonstrate.
General Procedural Sequence
Informed consent should be obtained from the patient, an intravenous catheter placed if sedation is to be used, and monitors applied (pulse oximeter, noninvasive blood pressure, and 3 to 5 lead EKG) if indicated based on use of sedation or on patient comorbidities. Resuscitation equipment, including oxygen source, mask and bag for ventilation, suction, code medications, and advanced airway equipment should be readily available. The patient should be properly positioned, and the injection site prepared and draped in standard aseptic fashion over an area large enough to allow palpation of landmarks. All medications, syringes, needles, and other equipment should be readily available. Syringes may vary from 3 to 12 mL. Needles may vary from as small as 1/2-in. (1-cm), 25-gauge needles to 31/2-in. (9-cm), 21-gauge spinal needles. For convenience, an 18-gauge needle should be available to draw medications from the vial. All caregivers participating in the injection procedure should be gloved and practicing universal precautions. An audible “time-out” involving confirmation of the correct patient, injection site, and injection side (if applicable) should be performed. Then, as the procedure is underway, there should be periodic communication with the patient to screen for any problems, such as severe pain from the needle, signs of local anesthetic toxicity, paresthesias, etc. After the injection is complete, the patient should be monitored afterward for any side effects, and reexamined to evaluate for proper distribution and efficacy of analgesia. Discharge instructions should be given to the patient including symptoms to expect, symptoms which warrant calling a nurse or physician, activity restriction (if any), follow-up scheduling, and personal log to record duration and intensity of pain relief.
Needle Insertion
To reduce pain of the initial needle insertion, the skin may be stretched while rapidly piercing the skin. Once the skin is pierced, the tension is released and the needle is advanced slowly. Rapid infusion of medication may result in tissue distention, causing pain. Other methods of reducing pain with initial needle insertion include the use of topical anesthetics and vapocoolant sprays.
Conscious Sedation
The procedures described in this chapter rarely require conscious sedation. In circumstances in which conscious sedation is used, monitoring should be applied to the patient as previously described, and advanced airway management tools should be readily available. Resuscitation equipment, medications, and personnel must be readily available. Any prior sedation records should be reviewed for previous sedation dose requirements and any anesthetic complications.
MEDICATIONS
Injection procedures use three primary classes of medication: local anesthetic agents, neurolytic agents, and corticosteroids. All of these medications have multiple clinical applications and are documented to be safe and effective when used appropriately. It is incumbent on the practitioner to understand the efficacy, complications, and common side effects of these agents.
Anesthetic Agents
The mechanism of local anesthetic action is a reversible block of ion flux through the axon’s sodium channels. By blocking transmission from the peripheral nerves, no input is detected at the central nervous system (CNS). The degree of neural blockade depends on the properties, absorption, amount, location, and other characteristics of the drug injected (
28,
29) (
Table 67-2). For purposes of attaining longer duration analgesia, agents such as bupivacaine or ropivacaine are acceptable and safe when used within the dosing guidelines. Anesthetic agents with fast onset, such as lidocaine, are useful particularly for skin infiltration prior to block insertion or for rapid diagnosis of the pain generator site. Local anesthetics should be chosen appropriately for both the purpose and the site of injection. For example, commercial preparations may come with preservatives, making them potentially neurotoxic if given intrathecally. Therefore, it is imperative to verify that the particular medication preparation is approved for the desired use. This information is available in many locations, including the package insert for the medication.
When higher doses of local anesthetics are used (i.e., near the upper limit of recommended dose), are injected near highly vascular structures (face, intercostals), or injected near the neuraxis (paravertebral, epidural, or intrathecal), monitoring of the patient is highly recommended. Verbal communication, constant screening for symptoms, and pulse oximetry can identify any CNS toxicity, while the electrocardiogram and blood pressure can identify any cardiovascular toxicity. If signs of toxicity or high spinal block are present, injection should be suspended and the patient closely evaluated and/or supported.
Neurolytic Agents
Neurolytic nerve blocks were popular in the early 1900s. However, improved use of analgesics, as well as the use of radiofrequency and cryoablative techniques, has replaced their use in most instances. Alcohol and phenol are the most widely used neurolytic agents in the United States. These agents indiscriminately affect motor and sensory nerves.
Phenol can be used intrathecally and epidurally, as well as for peripheral nerve and motor point blocks. It is poorly soluble in water and is often added to glycerin to achieve concentrations higher than 7%. It also can be added to radiographic contrast to allow fluoroscopic visualization of the spread during injection. Phenol has a local anesthetic effect, resulting in less pain after the injection. Because of this, long-term effects
of the block cannot be evaluated for 24 to 48 hours after the effects of the local anesthetic dissipate. Doses greater than 100 mg can result in serious toxicity (
30).
Alcohol is used primarily intrathecally for nerve roots and locally for sympathetic blockade. Patient positioning with intrathecal use is extremely important, because alcohol is hypobaric in cerebrospinal fluid (CSF). It is readily soluble in body tissues and produces intense burning on injection. It requires 12 to 24 hours before block effects can be determined.
Corticosteroids
Glucocorticosteroids are used in the injection treatment of inflammatory processes (
31) (
Table 67-3). Some of the commonly used forms of corticosteroid available for intraarticular injections are listed as follows:
Betamethasone sodium phosphate and acetate (Celestone Soluspan), 6 mg/mL
Methylprednisolone acetate (Depo-Medrol), 40 and 80 mg/mL
Prednisolone sodium phosphate (Hydeltrasol), 20 mg/mL
Prednisolone terbutate (Hydeltra-TBA), 20 mg/mL
Triamcinolone acetonide (Kenalog), 40 mg/mL
Triamcinolone hexacetonide (Aristospan) 20 mg/mL
These corticosteroids vary in strength, concentration, duration, and side effects, and all are effective. Triamcinolone hexacetonide has the longest duration of suppression of inflammatory activity. Fluorinated corticosteroids (e.g., triamcinolone) are rarely chosen for soft-tissue injection, because they are more likely to cause tissue atrophy. Prednisolone tebutate and methylprednisolone acetate are often used for soft-tissue injections because of their efficacy and cost.
SIDE EFFECTS AND COMPLICATIONS
The injection procedures described here are associated with various side effects, although the risk for significant complications is very low. The physician who performs injection procedures should have the training and education to recognize and treat a wide range of potential complications (
Table 67-4). Advanced cardiac life support (ACLS) protocols are used in airway management and cardiorespiratory resuscitation (
27).
Systemic Toxic Reaction
Various toxic reactions have been reported after use of local anesthetics, but with very low incidence. Local anesthetic agents are relatively lipid-soluble, low-molecular-weight compounds that readily cross the blood-brain barrier. As toxic levels are reached, disturbances of CNS function are observed initially, producing signs of CNS excitation. Early symptoms of overdose include headache, ringing in the ears, numbness in the tongue and mouth, twitching of facial muscles, and restlessness. As blood levels increase, generalized tonic-clonic seizures may occur. If sufficiently high blood levels are reached, the initial excitation is followed by generalized CNS depression. Respiratory depression and ultimately respiratory arrest may occur secondary to the toxic effect of the local anesthetic agent on the respiratory center in the medulla. Occasionally, the excitatory phase may not occur, and toxicity presents as CNS depression.
Cardiovascular system (CVS) effects either result indirectly from inhibition of autonomic pathways during regional anesthesia (as in high spinal or epidural block) or are directly due to depressant actions on the CVS. The CVS is generally
more resistant to toxicity than the CNS. The CVS-to-CNS toxicity ratio is lower for bupivacaine and etidocaine than for lidocaine. Convulsive activity may initially be associated with an increase in heart rate, blood pressure, and cardiac output. As the blood concentration of a local anesthetic agent increases further, CVS depression occurs, resulting in a decrease in blood pressure secondary to myocardial depression, impaired cardiac conduction, and eventual peripheral vasodilation. Ultimately, circulatory collapse and cardiac arrest may result. In addition, certain agents such as bupivacaine may cause ventricular arrhythmias and fatal ventricular fibrillation. The onset of CVS depression with bupivacaine may occur relatively early and be resistant to usual therapeutic modalities. The pregnant patient is more sensitive to the cardiotoxic effects of bupivacaine.
Systemic toxicity may be due to unintentional intravascular injection or drug overdose. Intravascular injection produces signs of toxicity (usually seizures) during the injection itself, especially if injected directly into blood vessels supplying to the brain (e.g., vertebral arteries). A relative overdose results in toxic reactions when peak blood levels are reached, about 20 to 30 minutes after the injection. Factors that affect the blood concentration (site of injection, drug, dosage, addition of vasoconstrictor, speed of injection) influence the potential for systemic toxic reactions to develop.
To minimize systemic reactions to local anesthetic agents, intravascular injection (the most common cause of seizures) should be avoided. Careful, intermittent aspiration should be used while injecting large quantities of local anesthetic agents. Patient complaints of metallic taste, numbness around the mouth, and ringing in the ears are suggestive of intravascular needle placement. Patients may be premedicated with midazolam or diazepam to raise the seizure threshold if necessary.
Systemic toxicity is treated with general supportive measures. If early signs of toxicity occur, constant verbal contact should be maintained, oxygen administered, breathing encouraged, and CVS function monitored. If seizure activity occurs, a clear airway should be maintained and oxygen administered by assisted or controlled ventilation. If seizures continue, thiopental (50 to 100 mg) or diazepam (5 to 10 mg) should be administered intravenously, avoiding large doses of thiopental, which may produce additional CVS or CNS depression. If airway maintenance is jeopardized, succinylcholine should be used to facilitate endotracheal intubation. Muscular convulsive activity is terminated with succinylcholine, but the seizure activity in the brain is not affected. If CVS depression occurs, hypotension should be treated by increasing intravenous fluids, positioning the patient properly (elevate the legs), and using vasopressors such as ephedrine or epinephrine (
Table 67-5).
Epinephrine Reaction
Reaction to epinephrine may sometimes be confused with local anesthetic overdose. Systemic absorption of epinephrine
produces palpitations and restlessness about 1 to 2 minutes after completion of the injection. Avoiding epinephrine should be considered in patients who are sensitivity prone (e.g., hypertensive, or hyperthyroid, arrhythmic patients). Epinephrine should not be used for blocks of the fingers, toes, or penis, owing to the possibility of localized vasoconstriction. An epinephrine reaction is treated with a small dose of fast-acting barbiturate to reduce blood pressure to within normal limits. If hypertension persists, a vasodilator may be required.
Vasovagal Reaction
Vasovagal reaction is a frequent response to injection procedures that is attributable to physiologic and psychological factors. This response may result in bradycardia, hypotension, and loss of consciousness. This usually occurs in the initial portion of the procedure when skin is penetrated before any medication is injected. Vasovagal reaction is often mislabeled as an allergic reaction to the medication. This response is often preceded by dizziness, faintness, sweating, and pallor. Vasovagal reaction is rapidly reversible by removing painful stimuli and placing the patient in a head down and legs up position to improve venous blood return to the heart. If this fails to relieve the symptoms, then treatment with general supportive measures is indicated, including airway maintenance, oxygen, intravenous fluids, anticholinergics such as atropine, and vasopressors such as ephedrine (see
Table 67-5).
Allergic Reaction
An allergic reaction to local anesthetic agents rarely occurs and in some instances may be confused with a vasovagal reaction or a reaction to epinephrine. Ester anesthetic agents (e.g., procaine, tetracaine) are more frequently associated with allergic reactions than amide anesthetic agents (e.g., lidocaine, ropivacaine), because esters are derivatives of paraaminobenzoic acid (PABA). However, the use of amides from multiple-dose vials may result in an allergic reaction secondary to the preservative methylparaben. Allergic reaction is treated with general supportive measures and the administration of fluids, antihistamine, steroids, and epinephrine (if warranted), as well as removal of any additional offending agent. The patient should be closely monitored for a clear airway.
Although this is a rare event, if there is a question of patient hypersensitivity to anesthetic agents, intradermal skin tests (injection with diluted [1:1,000] followed by undiluted local anesthetic) can be used successfully to diagnose adverse responses. However, false-positive results may occur. Anaphylactic shock is treated as systemic toxic reaction with attention to maintaining cardiovascular and ventilatory function (see
Table 67-5).
Accidental Spinal Block
Inadvertent subarachnoid or epidural blockade can occur with any injection that is performed close to the spine. These injections include intercostal nerve blocks, sympathetic blocks, and nerve root injections. Proper equipment and staff should always be available to treat any possible complication. This includes the ability to administer fluids and vasopressors if the patient develops hypotension from sympathetic blockade and to maintain ventilation with oxygen if the patient has impaired respiratory function.
Concurrent Medical Episode
Concurrent medical problems may be exacerbated by injection procedures. Hypotension will reduce myocardial profusion and may be a major factor for reinfarction in patients with ischemic heart disease. Patients with poorly treated hypertension risk developing hypertensive crisis, myocardial infarction, or stroke triggered by the stress of the procedure. Patients with chronic renal failure are more susceptible to toxicity from local anesthetics. Diabetic patients have an increased sensitivity to the effects of corticosteroid injection. Patients with liver disease may have reduced metabolism of local anesthetic medications resulting in an increased possibility of toxicity at standard doses. Other medical illnesses may decompensate clinically, owing to mild toxicity and changes in fluid and electrolyte balance. These risks are minimized
with appropriate monitoring and optimal medication regimes. Patients should be medically stable before undergoing elective injection procedures.
Infection
Although infectious complications rarely occur, cutaneous and joint infection, epidural abscess, bacterial meningitis, and adhesive arachnoiditis have been associated with injection procedures. Epidural abscess may cause spinal cord compression. Signs and symptoms of epidural abscess are severe back pain, localized tenderness, fever, leukocytosis, cervical rigidity, increased protein and leukocytes in the cerebral spinal fluid, progressive neurologic symptoms, and abnormal imaging studies of the spine. Early diagnosis and prompt treatment are essential to avoid catastrophic complications. Meningitis and adhesive arachnoiditis are the result of the introduction of bacterial or irritating contaminants into the spinal fluid as well as trauma during the procedure.
Pneumothorax
Injections into the thoracic region have the potential to cause a pneumothorax. In procedures that put the patient at risk for needle penetration of the lung, less than 1% develop a pneumothorax (
32,
33). Most of these patients can be easily treated with administration of 100% oxygen, close monitoring (e.g., O
2 saturation, vital signs) of the patient, and, when necessary, needle aspiration of air. Only those pneumothoraces that result in significant dyspnea or those under tension require chest tube thoracostomy and vacuum drainage. Bilateral thoracic procedures should be undertaken with caution due to potential risk of bilateral pneumothorax.
Nerve Injury
Three major factors contribute to nerve injury during injections: trauma, toxicity, and ischemia, with all three contributing to most nerve injuries. Nerve blocks are the result of infiltration of anesthetic agents around the nerve, not directly into the neural tissue. Intraneural injections directly injure nerve fibers and cause a breakdown in the blood-nerve barrier. The use of short, beveled needles has significantly reduced nerve injuries from injections. Intense pain in the nerve distribution and high resistance upon injection are often the result of intraneural needle placement and necessitate immediate cessation of the injection and repositioning of the needle.
Other Complications
Local anesthetic agents used in recommended clinical concentrations have minimal irritating effects on the nerves, skin, and subcutaneous tissue. Complete recovery of function occurs after regional blocks. The administration of large doses of prilocaine may lead to methemoglobinemia, owing to the accumulation of a metabolite (OH-toluidine) that can convert hemoglobin to methemoglobin. It may be treated with intravenous methylene blue.
Hypotension may result from sympathetic blockade. This commonly occurs in patients who are hypovolemic and receive a spinal or epidural block involving a large portion of the sympathetic chain ganglia. Hypotension is treated with general supportive measures, including administration of intravenous fluids, vasopressors such as epinephrine to maintain blood pressure within normal limits, and proper positioning (elevating the legs). Bradycardia from blockade of sympathetic outflow from T1-4 may require prompt treatment.
Bleeding at the site of injection occurs commonly at the surface. Hematoma at the site of injection is a possibility but usually not clinically significant. If arterial puncture occurs, prolonged direct pressure is usually adequate to prevent the development of a hematoma.
COMMON NERVE BLOCK TECHNIQUES
General
The placement of local anesthetics at various sites along the neural axis is an important tool in the diagnosis and treatment of a variety of pain disorders, such as complex regional pain syndrome and postherpetic neuralgia. Peripheral nerve blocks also can provide muscle relaxation and pain relief to facilitate an active physical therapy program.
When the point of injection has been determined, it is best marked with the tip of a retracted ballpoint pen or a needle hub by pressing the skin to produce a temporary indentation to mark the point of entry. The skin is then prepared in a standard sterile fashion, and sterile technique is used throughout the procedure. The skin and subcutaneous tissue at the injection site may be anesthetized by injecting 1% lidocaine with no epinephrine using a 25- to 30-gauge needle. Alternatively, a vapocoolant spray or analgesic cream applied to the skin surface may be used to provide adequate anesthesia.
Before injecting the medication, an attempt to aspirate should always be made to avoid accidental intravascular injection. After ensuring that the needle is in the joint space, the medication should be injected in a slow, steady fashion.
Indications for Nerve Blocks
Neural blockade may be used for the diagnosis, prognosis, and treatment of pain. Selective nerve blocks are indicated to determine the etiology of pain by isolation of specific anatomic structures. Selected nerve blockade is used to determine specific nociceptive pathways and other mechanisms involved in pain generation. Diagnostic blocks assist in narrowing the differential diagnosis of the site and cause of pain. Prognostic neural blockade is used to evaluate the possible outcome from neurolytic procedures. Therapeutic nerve blocks are indicated to decrease morbidity in acute postoperative pain, posttraumatic pain, and pain resulting from self-limiting conditions. Nerve blockade may provide rapid relief of pain and facilitate the patient’s participation in a comprehensive rehabilitation program. Therapeutic nerve
blocks may interrupt the pain cycle sufficiently to provide prolonged pain relief.
Contraindications for Nerve Blocks
Absolute contraindications for regional anesthesia include patient refusal, localized infection, a skin condition that prevents adequate skin preparation, the existence of a tumor at the injection site, a history of allergy to local anesthetics, the presence of severe hypovolemia (for blocks that could result in significant sympathetic blockade), gross coagulation defects, septicemia, and increased intracranial pressure (spinal, caudal, and epidural).
Prilocaine should not be used in doses greater than 600 mg, because significant methemoglobinemia may result. The use of corticosteroids with preservatives is contraindicated in epidural and subarachnoid techniques because the preservative may result in seizures and permanent CNS damage.
Relative contraindications include general medical conditions that would put the patient at increased risk. These include aortic stenosis, severe lung disease, sickle cell anemia, and preexisting neurologic diseases such as multiple sclerosis or amyotrophic lateral sclerosis, which could be worsened during regional anesthesia.
Complications
Complications common to nerve blocks include hypotension from sympathetic blockade. This usually occurs in patients who are hypovolemic and receive a block covering a large portion of the sympathetic chain ganglia, for example, during spinal or epidural blockade. Local anesthetic overdose or intravascular injection can result in CNS toxicity and, in some cases, pulmonary and cardiac arrest. Nerve injury from contact with the needle may occur but is rare, especially when a short, beveled needle is used. Other complications are dependent on the location of the block and are discussed separately.
Techniques
Before the injection, the appropriate landmarks are located and marked. The skin is scrubbed with antiseptic and allowed to dry for 2 minutes. The wearing of sterile gloves is required so that the bony landmarks in the sterile field may be palpated throughout the procedure. The standard sterile technique is required to minimize the risk for infection. It is preferable to use single-dose vials of the local anesthetic because this further reduces the risk for infection. A 25- to 27-gauge needle is used with 1% lidocaine with no epinephrine to raise a small skin wheal for skin anesthesia. Routinely a 11/2-in. (4-cm), 21- to 25-gauge needle transverses the skin, joint capsule, synovial lining and then slides smoothly into the joint cavity.
Aspiration is done to ensure there is no intravascular penetration. If penetration occurs, the needle should be repositioned and aspirated to ensure that blood vessels have been avoided; then the medication is slowly injected. After the medication has been injected, the needle should be cleared with a new syringe containing a small amount of lidocaine or saline. The needle is then withdrawn with pressure applied to minimize bleeding.
Nerve Stimulator
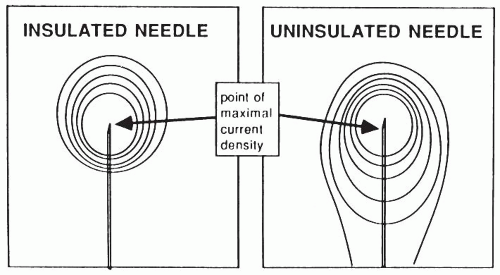
Peripheral nerves may be localized with a nerve stimulator using a small adjustable amount of electrical current to depolarize neural tissue in proximity to the needle. The cathode (negative) terminal is connected to the needle, and the anode (positive) terminal is connected to a grounding patch. The stimulator initially is set to deliver 10 to 20 mA of current to detect the general area of the nerve. The current is then reduced to further localize the nerve. The needle is positioned to produce the maximal twitch at the lowest stimulus. The needle is usually adjacent to the nerve when 0.5 to 0.1 mA produces motor stimulation with an insulated needle and 1 mA with an uninsulated needle (
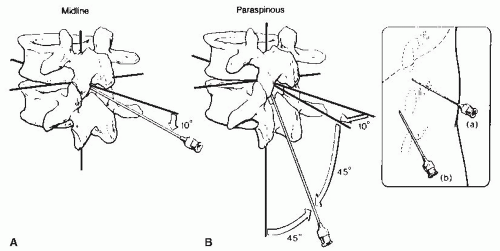
Fig. 67-1).
Nerve stimulators do not substitute for knowledge of anatomy and proper needle placement. Insulated needles increase the point of maximal current density at the needle tip and are used for precise localization of specific nerves. Uninsulated needles are often accurate enough for many nerve blocks; however, both the tip and shaft of the needle have sufficient current density to stimulate a nerve. Local muscle twitches from the shaft of the uninsulated needle should not be confused with the response from the nerve to be blocked (
Fig. 67-2).