23. Infections of the heart
Endocarditis
Clinical features
Patients with infective endocarditis present with non-specific symptoms such as fever, night sweats, arthralgias and usually a murmur. Infected valvular vegetations result in local tissue destruction, embolic events and formation of immune complexes. Valve destruction may present as new regurgitation or conduction block. Embolic events lead to the characteristic splinter haemorrhages (Fig. 3.23.1), Janeway lesions and cerebral and pulmonary infarcts. Immunological phenomena comprise painful Osler nodes on fingers, arthritis and glomerulonephritis.
Diagnosis
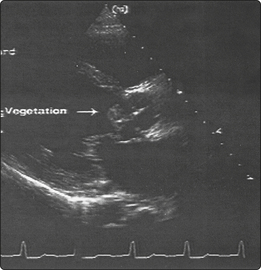
Echocardiography (Fig. 3.23.2) is the mainstay of diagnosis. Transthoracic echocardiography (TTE) is less sensitive (70%) than transoesophageal echocardiography (TOE), but more readily availabe in hospitals. Patients with abnormal native valves, prosthetic valves or calcification require TOE for imaging of vegetation or abscesses. Three to six blood cultures should be collected from different venepuncture sites within 24 h (spaced at least 1 h apart) before commencing antibiotic therapy. For the diagnosis of microorganisms that usually do not grow in blood cultures (Coxiella burnetii, Bartonella spp. and Chlamydophila psitacii), serological investigations should be performed. As symptoms are non-specific (Fig. 3.23.3), modified Dukes criteria have been developed to improve the diagnosis by weighting clinical symptoms. Division is made into whether a native or prosthetic valve is involved and the latter by time of onset: early (within 2 months of surgery) or late.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree