27. Infections of bone, joints and muscle
Osteomyelitis
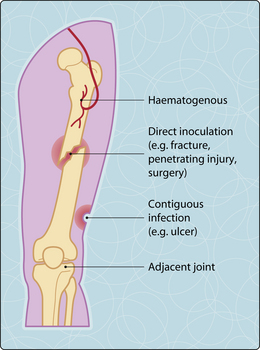
Infections of bone may arise from haematogenous and exogenous sources (Fig. 3.27.1). Bacteraemias in adults, particularly with Staphylococcus aureus and Brucella sp., may seed into adjacent vertebrae with their intervertebral disc (discitis). In prepubertal children, the metaphysis of tibia and femur may develop small post-traumatic haematomas under the growth plate, into which occult bacteraemia may nidulate. Patients with sickle cell disease are particularly at risk of salmonella osteomyelitis. In countries where tuberculosis is endemic, mycobacteria can settle in those niduses. Exogenous entry of bacteria occurs through open fractures, deep soft tissue defects (diabetic foot ulcers, decubital ulcers) or during surgical insertion of metal plates or prostheses. Prosthetic infections occur in less than 1% of elective total joint replacements; however, they are more common after hemiarthroplasties for traumatic fractures of the neck of femur.
Clinical features and diagnosis
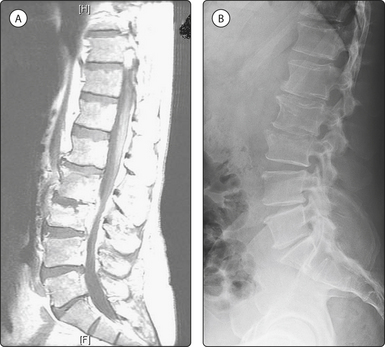
Haematogenous infections ususally present with fever and localized bone pain, whereas exogenous infections may have a more insidious onset, show chronic low-grade pain and may lead to mechanical loosening of the prosthesis or the metal plates. In over 50% of haematogenous infections, blood cultures may reveal the infectious agent. Magnetic resonance imaging can detect osteomyelitis earlier than radiography, which show bone destruction after a delay of 2–3 weeks (Fig. 3.27.2). Bone biopsy is useful for the aetiological diagnosis of the majority of exogenous infections, and joint aspirates may be contributory to the diagnosis of infected joint replacements.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree