7 Infections of bone and joints
INFECTIONS OF BONE
Infection of bone by pyogenic organisms is termed osteomyelitis.1 It occurs in acute and chronic forms. The only other infections of bone with which the student in Western countries need concern himself are tuberculous infections, although syphilitic infections and fungal infections may still occur occasionally in other parts of the world.
ACUTE OSTEOMYELITIS (Acute pyogenic infection of bone; acute osteitis)
Two distinct types of acute osteomyelitis must be considered:
The two types are sufficiently distinct to require separate descriptions.
ACUTE HAEMATOGENOUS OSTEOMYELITIS
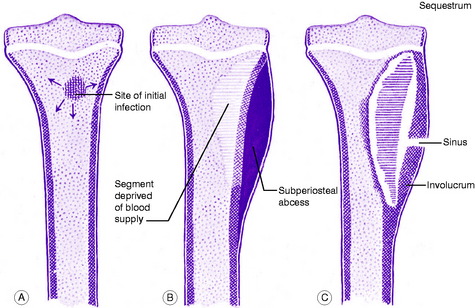
In the usual childhood manifestation, the infection begins in the metaphysis of a long bone, which must be presumed to form a productive medium for bacterial growth (Fig. 7.1A); thence it may spread to involve a large part of the bone. The organisms induce an acute inflammatory reaction, but the marshalling of the body’s defensive forces is greatly handicapped in bone because its rigid structure does not allow swelling. Pus is formed and soon finds its way to the surface of the bone where it forms a subperiosteal abscess (Fig. 7.1B); later the abscess may burst into the soft tissues and may eventually reach the surface to form a sinus.
Often the blood supply to a part of the bone is cut off by septic thrombosis of the vessels (Fig. 7.1B). The ischaemic bone dies and eventually separates from the surrounding living bone as a sequestrum (Fig. 7.1C). Meanwhile new bone is laid down beneath the stripped-up periosteum, forming an investing layer known as the involucrum (Fig. 7.1C).
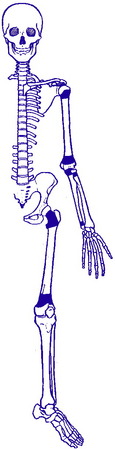
The epiphysial cartilage plate is a barrier to the spread of infection, but if the affected metaphysis lies partly within a joint cavity the joint is liable to become infected (acute pyogenic arthritis). Metaphyses that lie wholly or partly within a joint cavity include the upper metaphysis of the humerus, all the metaphyses at the elbow, and the upper and lower metaphyses of the femur (Fig. 7.2). Even when the joint is not infected it may swell from an effusion of clear fluid (sympathetic effusion).
Clinical features. Except for rare exceptions acute haematogenous osteomyelitis is confined to children, especially boys. The bones most commonly affected are the tibia, the femur and the humerus. The onset is rapid. The child complains of feeling ill, and of severe pain over the affected bone. There may be a history of recent boils or of a minor injury.
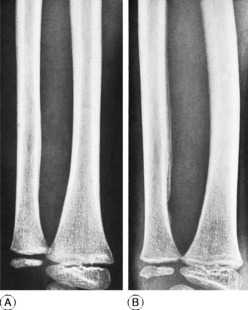
Imaging. Radiographic examination in the early stage does not show any alteration from the normal (Fig. 7.3A). Only after two or three weeks do visible changes appear, and they may never do so if efficient treatment is started very early. The important changes are diffuse rarefaction of the metaphysial area and new bone outlining the raised periosteum (Figs 7.3B and 7.4).
Radioisotope scanning with 99mtechnetium is reserved for the diagnosis of bone infection in the less clinically accessible sites such as the hip, pelvis and spine. Accumulation of isotope depends upon the rate of bone turnover and its vascularity, so that in the early stages of disease inadequate blood supply may result in a ‘cold’ lesion. More commonly, within a few hours or days of the onset of symptoms there is an increased uptake of isotope, giving a ‘hot’ scan at the site of the bone lesion. In the more obscure low-grade infections associated with prostheses and other surgical implants in bone, scanning with re-injected leucocytes labelled with 111mindium may provide improved diagnostic accuracy.
Acute osteomyelitis may also be confused with rheumatic fever, and, in infants, with vitamin C deficiency (scurvy) (p. 80). Whenever possible the causative organism must be identified bacteriologically. It is important that blood for culture be taken before antibiotic therapy is commenced.
Complications. The important complications are:
Acute osteomyelitis often passes into a state of chronic infection.
Treatment. Efficient treatment must be begun at the earliest possible moment.
Local treatment. The question of operation and its timing is still controversial. Operation may be unnecessary if effective antibiotic treatment can be begun within 24 hours of the onset of symptoms, and this should always be the aim. But in practice diagnosis is not always so prompt, and in that event it seems wiser to undertake early operation, in order to release pus and to relieve pain, which is often severe. This should definitely be performed if there has not been a marked improvement to the antibiotic treatment within 48 hours. Release of pus may also reduce the risk of ischaemic bone necrosis; and furthermore it allows the organism to be identified and its sensitivity to antibiotics determined. An incision at the site of maximum tenderness is made down to the bone and subperiosteal pus is evacuated. It is advisable – though not always essential – to make one or two drill holes through the cortex to improve medullary drainage. In most cases the wound may safely be sutured. Thereafter the limb is splinted until the infection is overcome.