Implants
John V. Vanore
Joint implant arthroplasty may be used to correct deformity, to restore motion, or to eliminate pain. Over the last 4 decades, significant advances have been made in biomedical engineering, biomaterials and surgical techniques. Implant arthroplasty has evolved from the simple silicone hemiimplant, through an era of commonplace use of the silicone hinged implant, to hopeful total joint designs analogous to knee and hip replacement, and then back to simple metallic hemiimplants.
Many of the same problems that perplexed early pioneers of joint implant surgery continue to provide similar problems for today’s surgeons. The selection of biomaterials, the design of the joint implants, and the response of the body to these implanted devices remain as objects of study. These devices have been manufactured from a variety of materials or combination of materials. The implants have varied greatly from simple designs with basic concerns to implant systems that attempt to incorporate design parameters for the complex biomechanics of the first metatarsophalangeal joint (1, 2, 3). The most difficult conclusion that surgeons have come to appreciate may be that the simple designs offer advantages over the complex ones.
Few topics have sparked as much debate as that of first metatarsophalangeal joint implant arthroplasty. There are advocates and critics of the various implants and those who have completely abandoned or condemned the use of these devices (4). Surgeons’ views have evolved with the changing clinical and medicolegal situations. Yes, there have been failures for numerous reasons, from use in patients who were simply too active to use in patients who did not have sufficient joint disease to warrant a joint-destructive procedure (2,5). Biomechanical problems are often the most difficult to avoid, and this may simply be an error of patient selection by the surgeon or unrealistic expectations on the part of the patient (6).
EVOLUTION OF FIRST METATARSOPHALANGEAL JOINT IMPLANT ARTHROPLASTY
The reader is referred to earlier editions of this textbook for many of the historical details regarding first metatarso-phalangeal joint implant arthroplasty (7,8). Generally, there were some early total joint systems, for example, those devised by Weil and Smith (9) and the Johnson Mayo Clinic (10,11) designs for the first metatarsophalangeal joint, but once Swanson developed the silicone hemiimplants and later the double-stem hinged implants, this can be viewed as stimulation for the first widespread use of implantation in these joints.
Early on, clinicians were mistaken in their application of these devices. Several errors were noted. Implants were used in patients who did not have joint disease to warrant a joint-destructive procedure, and implants were used in young patients whose activity demands were more than the implant and reconstruction could withstand. Implants, specifically silicone hemiimplants, were used in situations in which complication were likely, for example, in patients generally too young and too active, although end-stage degenerative arthrosis may have been present (12).
Double-stem silicone implants were widely employed in the 1980s, initially with the Swanson design predominating, but numerous other double-stem hinge silicone implants were developed and were marketed through Sutter Biomedical (San Jose, CA). These later implants attempted to incorporate design modifications to improve the functional result. Most notable of these was the Lawrence design, which limited resection of the hallucal phalangeal base in an attempt to avoid detachment of the short flexor tendon (13). Later, with the introduction of titanium grommets, the Swanson design regained popularity because of the protective function provided by the grommets that improved the durability of the reconstruction (2,14).
In the late 1980s, the crisis surrounding silicone breast implants made the daily headlines, and people became aware of silicone as a biomaterial, be it good or bad. During this time, other implants similar in design to their silicone counterparts were developed, but they failed to achieve much clinical success, the most notable of these being pyrolytic carbon by Intermedics Orthopedics (15). Little clinical success
was noted with this implant, but it heralded the oncoming new generation of total joint systems. The development of the Biomet Total Toe (Biomet, Warsaw, IN) by Koenig and Dow Corning-Wright was the first of a group of true total joint systems offering various design characteristics (16). Although four additional total joint systems were eventually introduced, none achieved widespread usage (2). In fact, as each successive total joint system was devised, it incorporated various features for potential correction of deformity and restoration of normal anatomy and bony alignment. None of these joint systems was simple to insert, and most were extremely complex even for the experienced surgeon (2). Postoperatively, complications, not unlike those of prior implants, were noted, and the functional advantages that these implants were intended to produce did not materialize (6).
was noted with this implant, but it heralded the oncoming new generation of total joint systems. The development of the Biomet Total Toe (Biomet, Warsaw, IN) by Koenig and Dow Corning-Wright was the first of a group of true total joint systems offering various design characteristics (16). Although four additional total joint systems were eventually introduced, none achieved widespread usage (2). In fact, as each successive total joint system was devised, it incorporated various features for potential correction of deformity and restoration of normal anatomy and bony alignment. None of these joint systems was simple to insert, and most were extremely complex even for the experienced surgeon (2). Postoperatively, complications, not unlike those of prior implants, were noted, and the functional advantages that these implants were intended to produce did not materialize (6).
Out of the past came the introduction of an old concept, the hemiphalangeal metal implant. Townley had been using a thin metallic button with a small phalangeal stem for more than 40 years. In 1994, this device was reported in the literature, and his success attracted renewed interest in the concept of hemiarthroplasty (17). Swanson et al. had been using titanium small joint implants similar in design to his silicone devices since the middle 1980s (18), and they reported a good success rate in both the foot and hand. Unfortunately, Swanson did not change the basic design of the hemigreat toe when it was remanufactured of titanium. In 1998, Lawrence, an originator of several silicone implants, introduced a metallic phalangeal implant incorporating design features of both earlier silicone implants and Townley’s implant (19). Lawrence’s implant offers a thin articulating base whose geometry more closely matches the anatomy that it was intended to replace. It allows for limited resection of the phalangeal base, particularly plantarly.
Some surgeons continued to use hinged silicone implants in a discriminatory manner and to achieve good results with limited complications. During the late 1990s, several other double-stem silicone implants were introduced, including the GAIT (Sgarlato Labs, San Jose, CA) design by Sgarlato Labs and the Primus (Futura Biomedial, San Diego, CA) by Futura (20). Later, protective grommets were released for the Futura implant.
As yet, I have not achieved a totally satisfactory joint implant for the first metatarsophalangeal joint. Historically, total joint replacement has been difficult and has not achieved widespread usage, and failed total joint arthroplasty is extremely difficult to revise (21). The hemiimplant offers a design that is easy to insert, may be associated with less complications particularly with regard to durability and function, and is usually not too difficult to revise, if necessary.
BIOMATERIALS OF IMPLANT ARTHROPLASTY
Most materials chosen for joint implantation were considered because of expected inert qualities. In the modern era of joint replacement, metals have been the initial choice, as for example, in total joint replacement of the hip (22, 23, 24). So too in the foot, Swanson began with stainless steel to replace the first metatarsal head (2,25). Soon, total joint systems became a composite system of components of various materials generally incorporating a metallic convex component articulating with an ultrahigh-molecular-weight (UHMW) polyethylene concave component. Many different concepts regarding bonding or adherence of implant materials to bone have evolved. Initial implants for the hip, toe, and other areas were not cemented, but simply impacted or “press fit.” Failures were encountered as a result of resorption and loosening. Acrylic bone cement was used as a grouting agent that stabilized the implant by means of mechanical interlock. The phenomenon of biologic ingrowth of bone then heralded the next generation of implants with surface coatings to enhance biointegration, for example, plasma-sprayed titanium or hydroxyapatite. A major problem with revision was then encountered with loss of bone mass. Today, major joint replacement systems are combinations of components manufactured for biologic ingrowth, mechanical interlock, press fit, screw fixation, or cementing. In each area of the intended arthroplasty, the most beneficial interface between implant and biologic material is assessed and is implemented.
Metallic and nonmetallic materials are used in joint implant systems (Table 1). The body’s corrosive environment and its poor tolerance or toxicity to even trace amounts of many elements make only a few metals potentially useful (24,26).
Metals
Metals generally begin as a liquid, in a heated state, and as they cool, metals take on a crystalline form. During this process, grains develop, and the size of the grain, its uniformity, and its orientation contribute to the physical properties of the metal. The crystalline structure of pure metals is often manipulated with the forging process or inclusion of additional elements that thus form mixtures or alloys. Both alloys and pure metals are used in the formation of joint implants. Some of the major metals are discussed.
Stainless Steel
Stainless steels have long been the biomaterials of choice for fixation systems because of their combination of strength, machinability, and cost of production. Stainless steel is an iron-based alloy with a chromium content of between 11% and 30% that comes in many forms, although generally either type 316 or 317 low carbon varieties are used in orthopedic applications (27). Stainless steels are less likely to be used in the joint implant market, but they deserve mention. Stainless steels possess good physical properties (ultimate tensile strength) for tensile loading, which is useful in fixation implants. Stainless steels have poor wear characteristics as a force-bearing surface as well as corrosion deficiencies, and so in the modern age of joint implantation,
the use of stainless steels has essentially been abandoned (26,28).
the use of stainless steels has essentially been abandoned (26,28).
TABLE 1. Biomaterials in implant arthroplasty | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Cobalt Chromium
Cobalt chromium metals are alloys with cobalt as the dominant element with lesser degrees of chromium and nickel. Cobalt may be present in a weight percent basis of 50% to 60% with a 20% to 30% chromium content and additional elements of nickel, molybdenum, and tungsten varying mainly on wrought versus cast alloys. Tungsten is formulated in wrought alloys to provide ductility, the deformation of a material that includes both elastic and plastic strain. Cast alloys are manufactured through molds with liquid metals that solidify in the desired shape, whereas wrought alloys are heated and forged with application of “pressing” techniques. Chromium improves corrosion resistance and nickel adds strength, but it is a bioactive element and may elicit tissue reactions including hypersensitivity (29, 30, 31). Cobalt chrome alloys are often chosen for the metallic component in total joint systems because of their excellent corrosion resistance and wear properties with the articulated polymeric component, usually UHMW polyethylene (24,28). This alloy is generally heavy in overall weight but possess excellent strength in compression, a desirable characteristic for joint implants. The manufacturing process is also more involved with the use of cobalt chromium alloys and is more expensive, particularly for fabrication of small joint implants.
Vitallium is the trade name of a cobalt chromium that was used in the Seeburger implants. During the development of a Swanson metallic hemiimplant, Weil used a cobalt chromium version of his angled great toe implant, but clinical trials did not warrant further investigation (Weil, personal communication, 1987).
Titanium
Titanium may be used in either its pure metallic form or as an alloy with aluminum and vanadium. The alloy is substantially stronger and is more resistant to brittle fatigue than pure titanium (27). Both are extremely inert and resistant to corrosion and have similar elastic moduli (32,33). Titanium is light in weight compared with cobalt chrome and stainless steel and is generally considered to have excellent characteristics with regard to osseous compatibility and biointegration. Titanium and its alloys used for implantation are attempts at introducing materials with properties that more closely approximate the physical properties of biologic tissues intended for replacement or implantation, that is, bone.
Today, Wright Medical (Arlington, VA) manufactures the Swanson hemigreat toe implant, as well as the hinged great toe grommets of commercially pure titanium (34,35). Titanium is usually not considered for articulating systems because of its poor resistance to erosion and production of wear debris (32,36, 37, 38). Biomet initially produced their Total Toe implant with a titanium metatarsal component treated with ionized nitrogen to improve its wear characteristics. Questions were raised regarding the durability and longevity of this nitrogen coating. Subsequently, Biomet changed to a cobalt chromium metatarsal component.
Ceramics
Ceramics used for orthopedic purposes include the crystalline ceramics silica and alumina. Generally, two classes of bioceramics are used: the biostable or inert and the bioactive or degradable. The former group has application as a component of a joint system, whereas the latter is used as a coating to enhance osseous integration.
Although ceramics are extremely inert and possess a high resistance to wear and a low coefficient of friction, their initial use was limited by their brittle behavior and low resistance to crack propagation (36,38). Today, the improved properties of aluminum and zirconium oxide ceramics have revived the application of bioceramics for joint implant systems. Some of the newest developments are with magnesium stabilized ceramics that show superior properties of fatigue.
Ceramics are excellent materials for situations of compression loading and articulation as a load-bearing surface and are generally considered superior to even cobalt chromium as the convex or ball component of a low-friction arthroplasty. Ceramics are currently used in various large joint replacement arthroplasties, and a great toe version was investigated by Diebold in France.
Ceramics are excellent materials for situations of compression loading and articulation as a load-bearing surface and are generally considered superior to even cobalt chromium as the convex or ball component of a low-friction arthroplasty. Ceramics are currently used in various large joint replacement arthroplasties, and a great toe version was investigated by Diebold in France.
Carbon
Carbon is one of the most compatible materials for implantation, and several forms are under investigation. The pyrolytic form possesses mechanical properties superior to those of graphite. Pyrolytic carbon is a two-phase graphite composite formed by pyrolysis to produce silicon carbide whiskers within a pyrolytic graphite matrix. This material possesses a low elastic modulus, similar to bone, yet with good strength and easy machinability (15).
A pyrolytic carbon nonconstrained first metatarsophalangeal joint was developed by Intermedics in the 1980s. This two-component system with oval convex and concave surfaces corresponding to the metatarsal head and phalangeal base, respectively (39), underwent clinical trials by Kampner (3,15,40). Although advocated for its low coefficient of friction, problems encountered included squeaking of the device with joint movement (V. Hetherington, personal communication, 1989). No further developments in small joint orthopedics were pursued.
Polymers
Polymers are long-chain molecules made up of simple repetitive subunits. These include the carbon-based thermoplastics—polyethylene, polypropylene, polymethylmethacrylate—as well as the silicon-based elastomer, silicone rubber. Polymers often develop their physical characteristics from processes during synthesis, including use of catalysts, antioxidants, plasticizers, and lubricants. Additives may preclude biologic implantation because adverse reactions may occur with leaching of even trace amounts of these substances. Polymers are interesting materials in that their physical properties are more complex than their metal counterparts, with a viscoelastic nature that more closely approximates biologic tissues.
Ultrahigh-Molecular-Weight Polyethylene
UHMW polyethylene is a plastic with good bearing characteristics, that is, a low coefficient of friction when it is articulated with metals and ceramics, although it has been associated with cold flow deformation or creep (27). It is best used as the concave component of total joint systems in which it is implanted with a titanium tray to improve its physical characteristics and to minimize host reactions. Good success has been achieved with low-friction arthroplasty with convex cobalt chromium or ceramic convex components. Polyethylene is considered an inert biomaterial because it is physically and chemically stable in vivo with little degradation. However, UHMW polyethylene wear debris may incite host reactions. Specifically, UHMW polyethylene produces small particles that have been associated with osteolysis and granulomatous reactions (41, 42, 43). These types of reactions generally lead to failure of a total joint reconstruction, often with instability of the component implants.
Polymethylmethacrylate
Bone cement is a polymeric grouting agent often used during the implantation of total joint systems for “cementing” components into the respective bones of the joint arthroplasty. Polymerization is a highly exothermic reaction, and this may be responsible for cellular death of a thin layer of bone after implantation. Bone cement requires a nominal thickness for it to be effective as a grouting agent, and the bone cement interface is usually the weak link in the total joint arthroplasty. Polymethylmethacrylate self-polymerizes and early on possesses low viscosity to allow intrusion and molding to both the internal bone structure and the implant stem. Difficulty may be encountered in small joint orthopedics because of the limited size of the implant and the area of bone implanted. Loosening may be encountered and subsequently failure of the reconstruction.
Silicone Rubber
Silicone rubber is an elastomer with a low elastic modulus, and thus it is a soft material. Clinically, this means that when subjected to loads within a functional range, the implant would deform, but on release, the implant would return to its original configuration (44, 45, 46, 47, 48). The low elastic modulus would also allow for the material to act as a shock absorber, not unlike the function of articular cartilage and subchondral bone (1). Therefore, the physical properties of silicone rubber are such that it would be unlikely to cause resorption of adjacent bone, as was seen with metallic cup arthroplasty.
Swanson championed flexible implant arthroplasty with silicone rubber devices. Instead of fibrous tissue coating a device and heralding loosening, his nonporous interpositional material encouraged fibrous tissue production to augment resection arthroplasty with newfound connective tissue stability (45,49). This is the basis for Swanson’s concept of “fixation by encapsulation.”
Metallurgists manipulate alloys or the manufacturing process to design the properties of implanted materials, rather than simply selecting from a limited group of materials. Compounds that may have once been discarded because of their brittleness or inadequate strength may now be manipulated to give the desired or even superior properties, such as magnesium-stabilized ceramics. Biomaterials are currently under development today, but because of the responsibility
of manufacturers, medical professionals, and government to our human implantees, a great deal of study and research must be done before new materials are available for general use. One of the other concerns in today’s society is the realization of the potential liability with human implantation. Manufacturers who once may have supplied basic biomaterials to the implant manufacturing companies now may be reluctant to do so in light of threats such as the silicone beast implant crisis, wherein not only was the implant manufacturer held responsible, but also the supplier of the silicone rubber. Dow Chemical and DuPont have discontinued the supply of several materials used for medical implants including polyester, silicone, Teflon, Dacron, and polyurethane. Montell/North America, a supplier of UHMW polyethylene, informed medical device manufacturers that they would no longer supply the raw material for surgical implants out of fear of litigation. This leaves only Hoechst Celanese Corporation, a German company, as the remaining supplier of UHMW polyethylene.
of manufacturers, medical professionals, and government to our human implantees, a great deal of study and research must be done before new materials are available for general use. One of the other concerns in today’s society is the realization of the potential liability with human implantation. Manufacturers who once may have supplied basic biomaterials to the implant manufacturing companies now may be reluctant to do so in light of threats such as the silicone beast implant crisis, wherein not only was the implant manufacturer held responsible, but also the supplier of the silicone rubber. Dow Chemical and DuPont have discontinued the supply of several materials used for medical implants including polyester, silicone, Teflon, Dacron, and polyurethane. Montell/North America, a supplier of UHMW polyethylene, informed medical device manufacturers that they would no longer supply the raw material for surgical implants out of fear of litigation. This leaves only Hoechst Celanese Corporation, a German company, as the remaining supplier of UHMW polyethylene.
IMPLANT DESIGN AND FUNCTION
A synovial joint is a system that allows movement between connecting osseous lever arms, allows smooth transmission of forces, and does so with an incredible efficiency and a minimum of wear (50). It is when a joint deteriorates that reconstruction is necessary. Reconstruction of the first metatarsophalangeal joint is the focus of this chapter and discussion.
Normally, during the stance phase of gait, the intrinsic musculature stabilizes the hallucal proximal phalanx against the ground and the metatarsal (51). From the time of heel off to the end of stance, the first metatarsal is moving relative to the phalanx. Sagittal plane motion predominates, although a small degree of frontal plane inversion occurs (52, 53, 54, 55, 56). The motion of the first metatarsal and first ray allows for weight transmission through the foot, medial column, and finally the hallux before toe off and the repetition of the cycle (44,57,58).
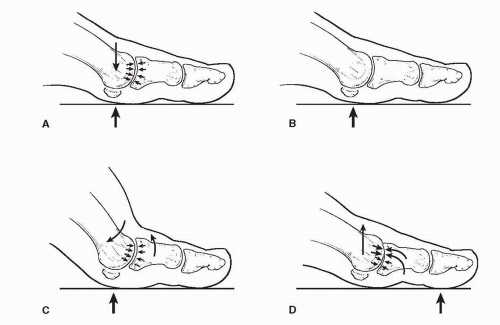
In the pronated foot, or with first ray hypermobility, instead of stabilizing the hallux, the musculature contributes to subluxation at the first metatarsophalangeal joint (52,59). This situation eventually leads to either transverse plane or sagittal plane deformities, hallux abducto valgus or hallux rigidus, respectively. Deterioration of the joint usually occurs with end-stage hallux valgus deformities, as a result of progressive joint subluxation, or in the case of hallux rigidus, the arthrosis occurs more rapidly because of pathologic joint abutment (Fig. 1). Arthritic joint changes are degenerative and are associated with a limitation of motion and with pain (60,61). Trauma, whether it be a previous injury or surgery,
usually leads to a much more rapid progression of joint arthrosis (62).
usually leads to a much more rapid progression of joint arthrosis (62).
The most important attribute of a diarthrodial articulation is the integrity of its joint space. Joint movement depends on maintenance of a joint space. Unfortunately, this ultralow friction system undergoes narrowing and or disruption during aging or as a result of arthritic conditions (63,64). Surgical reconstruction of arthritic joints is predicated on the reestablishment of the joint space to provide normal joint mechanics.
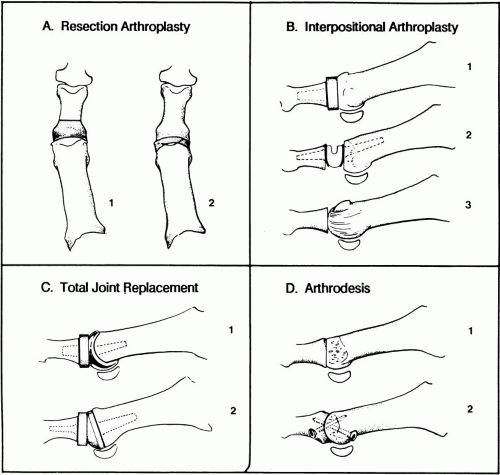
Instability or joint deformity is addressed with bone resection and soft tissue release (Fig. 2). Reestablishment of the joint space also depends on bone resection. In the case of the first metatarsophalangeal joint, resection arthroplasty, particularly on the phalangeal side of the joint, is a wellaccepted technique (65, 66, 67, 68, 69). An interesting development has been advocated that uses external fixation placed across a joint in tension mode to open up a joint space gradually and thereby to reestablish joint motion (70).
Interpositional arthroplasty uses soft tissue or artificial materials to maintain the joint space after osseous resection (23,45,49,71,72). With total replacement arthroplasty, both sides of the joint are replaced with an articulation that will conform to or maintain contact with the opposite side and allow for movement (73). Difficulties arise because of differences in mechanical properties, limited areas of contact, and wear in the artificial system.
Implant arthroplasty of the first metatarsophalangeal joint can be viewed as two categories: interpositional arthroplasty and total joint replacement. The former was much more widely performed and can also be divided into two types, hemiimplant and flexible hinge. Numerous designs of each are available.
Interpositional Implants
Interpositional joint implants are an adjunct to resection arthroplasty. The intention was that the implant would improve short and long-term alignment and movement, and overall would yield a cosmetically superior reconstruction compared with resection arthroplasty alone. Interpositional devices are generally either of the concave cap with an intramedullary stem or a convex ball type of design also with an intramedullary stem. The former is best illustrated by the Swanson type great toe hemiimplant, and the latter is best illustrated by the ulnar head design or the original Swanson design for the first metatarsal. Interpositional devices are also fabricated as double-stem hinge implants. These designs generally only allow motion in one plane, that is, perpendicular to the hinge.
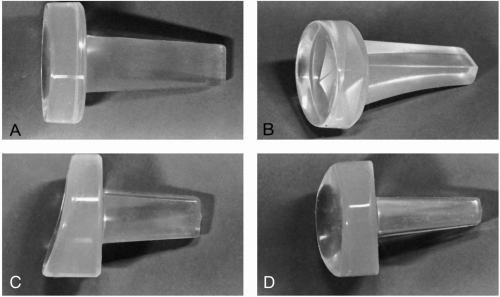
The early silicone implants were probably the best example of hemiimplants (Fig. 3). The standard great toe or hemiimplant was designed by Alfred Swanson after analysis of the normal proximal phalanx (71,74). He introduced the implant as an interpositional spacer to maintain the joint space of resection arthroplasty. He described the process of reparative fibrosis or encapsulation as an intimate component of flexible implant arthroplasty wherein he believed that the implant acted as an internal mold for development of a new capsuloligamentous system. His concept of implant
arthroplasty was summarized by the equation: “bone resection + implant + encapsulation = new joint” (45,74).
arthroplasty was summarized by the equation: “bone resection + implant + encapsulation = new joint” (45,74).
Swanson’s original great toe implant can be described as a base or collar with a medullary stem. The base represents the resected portion of the phalanx and is ovoid, being wider from medial to lateral than its height from dorsal to plantar. The articulating portion of the base possesses a shallow concavity corresponding to the convex shape of the first metatarsal head. This can actually be defined by separate dorsal to plantar and medial to lateral arcs, each with a defined radius (75). The stem possesses a certain overall length and is rectangular at the end while being square at the juncture with the base. Because the phalanx was concave plantarly, Swanson incorporated this into the design of the stem (74). Most of the initial medullary stems of the hemiimplants were large and required significant reaming of the respective phalanx.
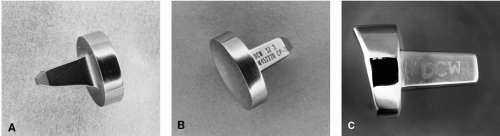
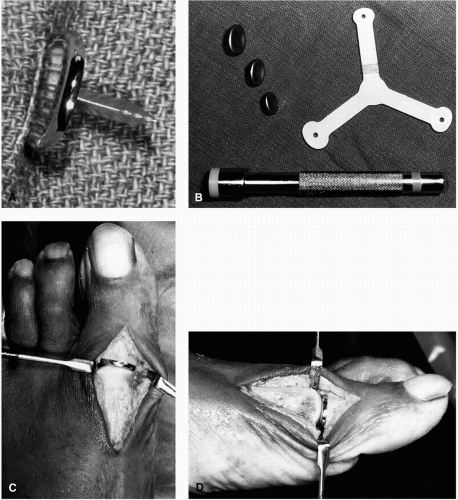
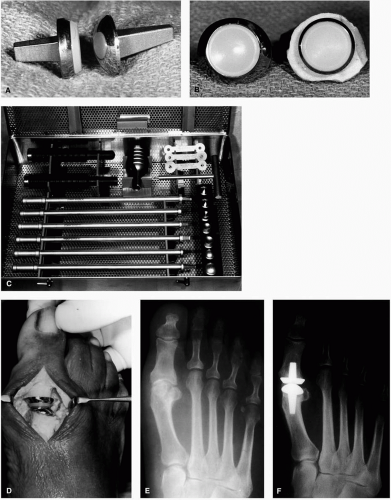
Later, Swanson and Weil each designed analogous metallic versions of their original hemiimplants (Fig. 4). The design
of Townley (Fig. 5) incorporated two unique differences. The first was a small stem that did not require reaming of the proximal phalanx, and the other was a thin articular base. Because Townley’s implant was manufactured from metal, cobalt chromium, he realized that the base could be reduced to a nominal thickness and still provide superior physical properties (17). This design allowed for limited resection of the phalangeal base, better quality of remaining bone, and limited loss of soft tissue attachment to the base of the proximal phalanx. In fact, it eliminated the requirement for reaming of the phalanx by introducing a thin, swordlike stem.
of Townley (Fig. 5) incorporated two unique differences. The first was a small stem that did not require reaming of the proximal phalanx, and the other was a thin articular base. Because Townley’s implant was manufactured from metal, cobalt chromium, he realized that the base could be reduced to a nominal thickness and still provide superior physical properties (17). This design allowed for limited resection of the phalangeal base, better quality of remaining bone, and limited loss of soft tissue attachment to the base of the proximal phalanx. In fact, it eliminated the requirement for reaming of the phalanx by introducing a thin, swordlike stem.
More recently, Futura Biomedical also released a metallic hemiimplant (Fig. 6), which may be considered a hybrid between the Swanson and Townley designs. This implant has a thin base but incorporates a plantar angulatory resection of the phalangeal base as noted on the Lawrence hinged silicone implant (19). In addition, the medullary stem is significantly reduced in size from the Swanson implant but still is more of a traditional medullary stem than that of the Townley design.
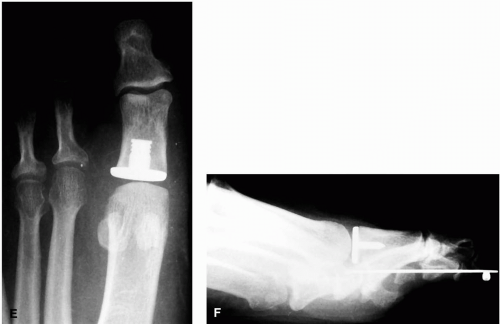
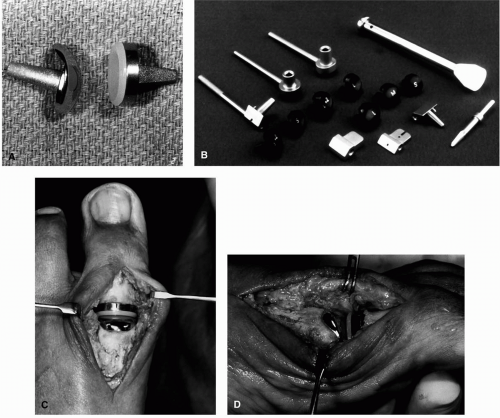
Several double-stem silicone implants are available for interpositional arthroplasty (Fig. 7). The two earliest designs were the Swanson flexible hinge and the Cutter hinged implants. Later, variations of the theme were introduced by Sutter, Sgarlato, and Futura Biomedical.
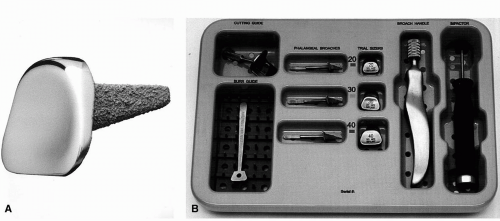 FIG. 6. A: The Futura design (Futura Biomedical, San Diego, CA) is a hybrid of the older-model Swanson-like hemiimplant and the Townley design. B: Instrumentation allows for ease of insertion. |
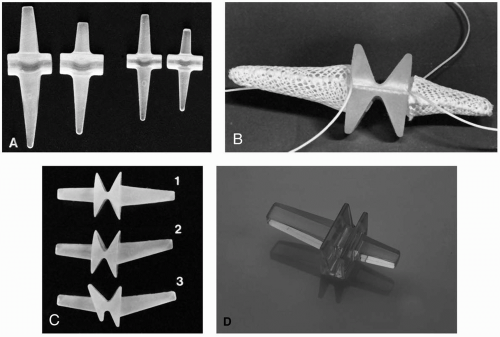 FIG. 7. First metatarsophalangeal joint: double-stem hinged silicone implants. A: Swanson’s original great toe hinged implant was later modified as a short stem version. B: Sutter (Sutter Biomedical, San Jose, CA) had an early design with a barrel-like stem, whereas later modifications (C) by LaPorta (1) and (2) and Lawrence (3) attempted to increase implant hinge motion and more accurately to replicate normal anatomy. D: Sgarlato later introduced his design as the “GAIT” implant. |
The Swanson design was available in seven anatomic sizes (76). A central hinge in a U-shaped configuration allows for dorsiflexion. An intramedullary stem on either side stabilizes the implant within the phalanx and metatarsal. This hinge has been criticized for not allowing a physiologic amount of motion (77). The stems are a square, tapered configuration, with the phalangeal side shorter and narrower. There is no angulation of the stems in the sagittal or transverse plane. With the original design, it was often necessary for the surgeon to shorten the phalangeal implant stem. In an effort to avoid any tampering or modification of the implant, Dow Corning-Wright introduced a short-stem variation of the double-stem design that quickly supplanted most use of the original design. This implant is manufactured in six sizes: 0S, 1S, 2S, 3S, 4S, and 5S (76).
Wright Medical, which later manufactured the Swanson design Silastic implants, introduced titanium grommets for the double-stem implant (35) (Fig. 8). These grommets were designed as a protective interface between the cut surface of bone and the implant hinge (14,78). The grommets were press fit into the respective medullary canals before insertion of the implant.
Sutter Biomedical introduced several designs of a hinged great toe metatarsophalangeal implant, the LaPorta (79) and the Lawrence (80), and these devices are now manufactured by Futura Biomedical. Both designs incorporate the more stable design of rectangular tapered stems. The proximal stem is slightly larger and longer than the distal and is angled 15 degrees dorsally in the sagittal plane. This feature was incorporated into the design to allow for the declination of the first metatarsal without compromising the excursion of sagittal plane motion inherent to the hinge. This design characteristic also limited tensile strain on the implant that results from dorsiflexion of the toe.
The LaPorta implant comes in a right, left, and neutral design, terms referring to the deviation of the stems in the transverse plane (79). The neutral design possesses the stems at 180 degrees from each other, whereas the right and left varieties possess a 10-degree angulation lateralward in the transverse plane. The Lawrence implant is neutral (80).
The hinge of both Sutter implants is an hourglass-type design with flexion occurring at the central juncture. The LaPorta design is symmetric from dorsal to plantar and is designed to allow 60 degrees of motion in the hinge alone (81). Either side of the hinge proximal and distal is flat to allow flush apposition with the resected joint surfaces.
The Lawrence hinge differs in that the hinge is elongated dorsally and is angled inferiorward (80). The hinge design
functionally has several advantages. It was designed to allow 85 degrees of dorsiflexion (82). The plantar angulation on the phalangeal side of the hinge ideally reduces the degree of basal resection of the phalanx and thereby maximizes hallucal stability through maintaining intrinsic tendon insertions. Lawrence also recommended angulating the metatarsal osteotomy, in an effort to preserve length and stability, as well as the metatarsal articulation with the sesamoids (13).
functionally has several advantages. It was designed to allow 85 degrees of dorsiflexion (82). The plantar angulation on the phalangeal side of the hinge ideally reduces the degree of basal resection of the phalanx and thereby maximizes hallucal stability through maintaining intrinsic tendon insertions. Lawrence also recommended angulating the metatarsal osteotomy, in an effort to preserve length and stability, as well as the metatarsal articulation with the sesamoids (13).
The Sgarlato design is a hybrid between the Swanson and Sutter designs incorporating a hinge not dissimilar from Swanson, with the stems at 180 degrees in both the sagittal and transverse planes (83).
Sammarco showed that the normal first metatarsophalangeal joint axis is constantly changing but it remains within the first metatarsal head (53,55,56). With a hemiimplant, normal joint dynamics are changed to a lesser extent than the double-stem implants. With the double-stem implants, the joint axis and function are significantly altered. Depending on the degree of bone resection on either side of the joint, the joint axis will now fall distal to the axis before surgery. There is also a loss of Hick’s effect or the reciprocal motion between the phalanx and its metatarsal that reduces medial column stability (7). These functional limitations are the result of the constraint of the hinge that allows only simple rotatory motion about the axis defined by the location of the hinge of the implant.
TOTAL JOINT REPLACEMENT
Total joint systems have been designed as two-component semiconstrained or nonconstrained articulations for the first metatarsophalangeal joint. The former allows for only sagittal plane motion, whereas the latter allows motion in more than one plane. Materials used for opposing articular surfaces are chosen for their low coefficient of friction and their minimum wear characteristics.
Certainly, there were some early attempts by several surgeons including Joplin, Johnson (10), and Weil and Smith (9), but none of these designs proved successful enough to warrant general release. In examining the reports by early surgeon inventors, several conclusions can be drawn. Metatarsal components, whether cemented or simply press fit, generally loosened as a result of loading on the weight-bearing side of the joint. This instability was preceded by resorption around the stem on follow-up radiographs. Often, the joint reconstruction was compromised by pain or joint stiffness, which was the original reason for performance of the procedure.
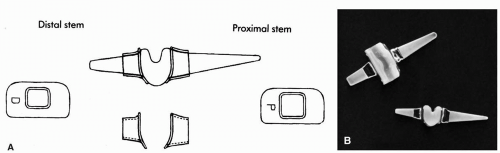
Biomet Total Toe (Biomet, Warsaw, IN)
The concept of a total joint system was again revived by Koenig (16), who modeled his design after the Whiteside knee system, both developed at Dow Corning-Wright (Dow Corning-Wright, personal communication, 1991). This involved a two-component articulating device with the metatarsal component made of titanium and the phalangeal one of UHMW polyethylene (Fig. 9). The metatarsal component possessed a large plantar flange that interlocked the plantar cortex and could provide for an articulating surface for the sesamoids, although Koenig later reported difficulties with the sesamoid implant articulation (84).
Titanium components are often advocated for their qualities of osseous integration and biocompatibility with bone. Problems with earlier metal components for the metatarsal involved bone resorption and loosening of the stem resulting from imposed stresses (11,71). The plantar ledge of this design was devised not for weight bearing but for translation of loading forces from the stem and into the greater portion of the metatarsal. In addition, the cobalt chromium metatarsal component was coated with plasma-sprayed titanium to enhance its osseous stability by means of tissue ingrowth.
The Biomet Total Toe system has been available for general use since 1989, after initial clinical trials were conducted by the surgeon inventor. Koenig reported a mean range of motion of 50 degrees in 18 procedures 18 months postoperatively (16). He recommended the implant for a wide range of deformities with arthrosis.
Bio-Action Great Toe Implant (MicroAire Surgical Instruments, Valencia, CA)
The Bio-Action implant is a spheric articular design the goal of which is to allow motion in all planes. It consists of a cobalt chromium metatarsal component and an UHMW polyethylene phalangeal component in two anatomic sizes with some variation, as described here (Fig. 10). The phalangeal component is available in a small or modified version. The small component is circular with a neutral stem 90 degrees to the articulating surface. The modified version provides a titanium flare to extend beyond the circular polyethylene articulating surface to provide additional stability when bone resection of the base of the proximal phalanx leaves a medial and lateral metaphyseal flare. This component is also flattened on its plantar surface but is otherwise neutral in the transverse and sagittal planes.
The metatarsal components are a spheric cap with a tapered rectangular stem. The implant comes in a small and large neutral version or a small right and left modification. All components possess tapered rectangular stems. On the neutral components, the stems are at 90 degrees to the articulating surface, whereas with the right and left versions of the metatarsal component, the stem is deviated 10 degrees in the transverse plane to allow for a degree of abduction of the great toe, as normally found. This does require that the distal metatarsal head be resected at an 80-degree angle and is proposed to improve the excursion of motion with the reconstruction.
Zang et al. stated that this implant was used in more than 250 patients, and these investigators examined 34 of these patients, randomly selected, with an average follow-up of 26 months. The patients, 30 women and 4 men, ranged in age from 19 to 79 years, with an average of 61.5 years, and they were selected for joint implantation with a variety of disorders from hallux valgus with degenerative arthrosis to hallux limitus, rheumatoid arthritis, and failed prior first metatarsophalangeal joint procedures. These investigators reported good range of motion postoperatively without delineating dorsiflexion from total range of motion (85).
More recently, Gerbert and Chang reported on use of 10 Bio-Action implants over a 3-year period in patients with an average age of 49 years (6). Two implants required removal, and this article discusses indications and complications of total joint replacement implants in general.
Acumed Great Toe System (Acumed, Beaverton, OR)
The Acumed system is another of the component joint replacement systems. This is the only total joint replacement system that was designed to be press fit, although it may also be cemented (R. Hubner, personal communication, 1995). This system also combines a cobalt chromium metatarsal component and a UHMW polyethylene phalangeal component (Fig. 11). The metatarsal component possesses a dorsal flange or dorsal extension of the articular surface to allow an increased range of dorsiflexion of the first metatarsophalangeal joint. A beaded area on the metatarsal component allows for biointegration with the distal resected surface of the metatarsal head.
The metatarsal component is available in three anatomic sizes: small, medium, and large, all with the same-size tapered cylindric medullary stems to allow complete interchangeability of the various sizes. The phalangeal components are available in small and large sizes in both a standard and + 2 mm size, one with a narrow and other with a wider thickness of the base portion. The phalangeal stems are of a tapered rectangular configuration, and again all are the same and are interchangeable.
The only preliminary report involving use of this implant was published by Gerbert and Chang (6). They reported use of 21 implants in patients with an average age of 50 years. Dorsiflexion increased from an average of 25 degrees preoperatively
to 53 degrees postoperatively. No implants required removal, but several complications were noted, although these authors discussed their observations on the use of both Acumed and Bio-Action total joint replacement systems collectively.
to 53 degrees postoperatively. No implants required removal, but several complications were noted, although these authors discussed their observations on the use of both Acumed and Bio-Action total joint replacement systems collectively.
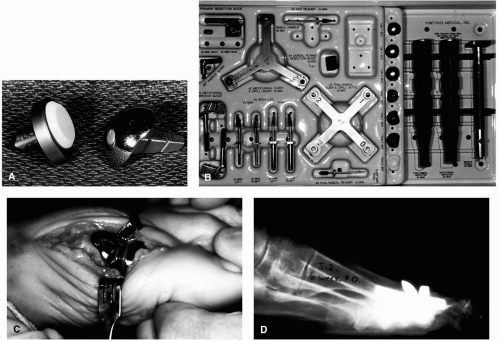
Kinetik Great Toe Implant (Kinetikos Medical Inc., San Diego, CA)
The Kinetik Great Toe Implant joint replacement system is marketed as an anatomic design attempting to incorporate features to accommodate metatarsal declination, intermetatarsal angle, and proximal articular set angle. The metatarsal component is manufactured from cast cobalt chromium, whereas the phalangeal component is a titanium alloy (Fig. 12). A UHMW polyethylene articular inset is found within a thick phalangeal base. The metatarsal component is available in right and left designs incorporating a 13-degree offset of the stem in the transverse plane as well as a 12-degree inclination in the sagittal plane. The articular surface is a spheric design but is extended dorsally to provide a surface for further joint extension; this does require resection of a portion of the dorsal cortex.
The metatarsal component is available in three sizes in both left and right models, whereas the phalangeal component is available in four sizes, and each is interchangeable with any of the six, left and right, metatarsal components.
The metatarsal stems are a tapered rectangular configuration, whereas the phalangeal ones are round with a distal point and a flute not dissimilar to that found on a tap or selftaping screw. All the stems on the respective metatarsal and phalangeal implants are the same size, meaning that the final implant size may be varied right to the point of insertion of the implants. The stems possess a roughened surface and grooves on the stems to improve the likelihood of osseous integration. The metatarsal component is available in three anatomic sizes: small, medium, and large, all with the same size tapered rectangular medullary stems to allow complete interchangeability of the various sizes. Each size metatarsal component is available in right and left versions. The phalangeal components are available in small and large sizes, one with a narrow and another with a wider thickness of the base portion. The phalangeal stems are of a round naillike configuration with the tip pointed and a fluted surface to the stem. All stems are the same size and therefore are interchangeable.
A full set of instruments is available and is numbered 1 to 8, to facilitate chronologic use and the recommended surgical technique. As with all the total joint systems, familiarization with the implant design and with surgical instrumentation is pivotal for success.
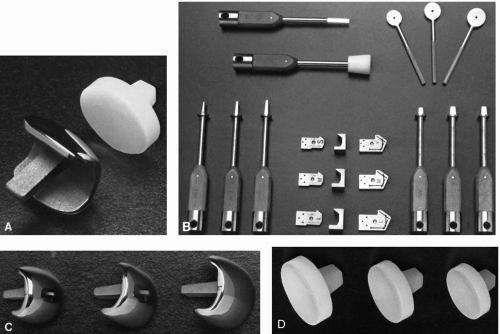
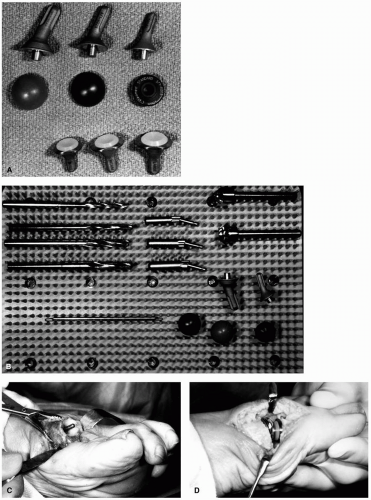
Osteomed Reflexion First Metatarsophalangeal Joint Implant System (Osteomed Corp., Irving, TX)
The Osteomed total joint system, the last of the currently available first metatarsophalangeal joint replacement systems
to be introduced, is markedly different from the preceding four implants. This implant also has a metatarsal and a phalangeal component, but the metatarsal prosthesis is actually two separate implants (Fig. 13). The titanium alloy metatarsal stem is round with ridges cut into the peripheral proximal stem with a conical portion distally. This serves as the foundation for a cobalt chromium convex articulating cap that snaps onto the distal stem. The conical portion of the metatarsal stem is dorsally angulated from the proximal stem, so it also provides for greater excursion of dorsiflexion or extension. As a result of this offset design, it is anticipated that it will provide increased stability of the metatarsal component.
to be introduced, is markedly different from the preceding four implants. This implant also has a metatarsal and a phalangeal component, but the metatarsal prosthesis is actually two separate implants (Fig. 13). The titanium alloy metatarsal stem is round with ridges cut into the peripheral proximal stem with a conical portion distally. This serves as the foundation for a cobalt chromium convex articulating cap that snaps onto the distal stem. The conical portion of the metatarsal stem is dorsally angulated from the proximal stem, so it also provides for greater excursion of dorsiflexion or extension. As a result of this offset design, it is anticipated that it will provide increased stability of the metatarsal component.
The phalangeal portion of this implant system is a circular polyethylene concave articulating disc integrated onto a titanium-backed stem. The stem itself is round and distally flattened on two surfaces, whereas the proximal portion is also conical.
The articular surfaces of this spherical system have been designed so the one-size metatarsal head is completely compatible with any size phalangeal component. The metatarsal stems and phalangeal components come in small, medium, and large, whereas the metatarsal head is available in small, large, and extralarge.
Instrumentation is provided to allow precise fitting of the joint replacement system, although as with all these systems, each possesses individual surgical details and subtleties that must be mastered.
Synopis of Total Joint Replacement Systems
Total joint systems have been designed as two-component nonconstrained articulations for the first metatarsophalangeal joint that allow for not only sagittal plane motion but also small amounts of motion in the frontal or transverse plane as required by the excursion of the resultant joint reconstruction. Materials used for opposing articular surfaces are chosen for their low coefficient of friction and their minimum wear characteristics. The accepted standard is a cobalt chromium alloy with UHMW polyethylene. Many of the total joint systems have incorporated design features to resemble normal anatomy more closely and, one hopes, to improve the functional result of the reconstruction. As yet, there is no consensus that the use of these implant systems has any value. These systems have been recommended for many reasons, but as yet clinical studies to warrant the widescale use of these devices have not materialized. Only a few reports have been written, and most are little more than preliminary case reports.