Imaging of the Hip
Kawan S. Rakhra and Adnan M. Sheikh
Key Points
Introduction
Radiologic investigation of the hip has rapidly evolved through advances in technology and in knowledge about the causes and physiology of hip disease. In situations where the clinical history and physical examination findings are equivocal, orthopedic diagnosis and management of hip disorders often require adjuvant radiologic evidence of disease before treatment and intervention are begun. Today, several imaging modalities are available to physicians; each modality has a multitude of variations and protocols that can be optimized according to the patient profile, the clinical scenario, and the nature of the hip pathology. It is important for the orthopedic surgeon, radiologist, rheumatologist, and physiatrist, and all other allied musculoskeletal specialists, to understand the basic principles of hip imaging. Knowledge of the strengths and limitations of the various available radiologic modalities can facilitate and expedite efficient diagnosis and management of hip pathology.
Imaging Modalities
The various imaging modalities are compared in Table 31-1.
Table 31-1
Comparison of Modalities
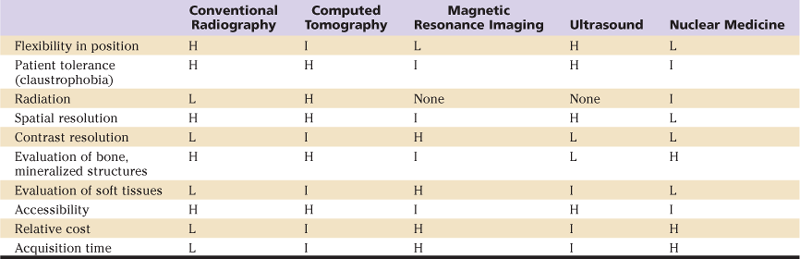
H, High; I, intermediate; L, low.
Conventional Radiography
Radiography is the first line of imaging for investigation of all hip pathologies, as it can demonstrate gross osseous alignment, morphology, and integrity. Advantages of plain radiography include ease of access, rapid acquisition, lack of any post processing, and flexibility in patient positioning. However, the shape, contour, and spatial relationships of bones may not be demonstrated by radiography to the same degree as by cross-sectional modalities such as computed tomography (CT) and magnetic resonance imaging (MRI).1–3 Radiography is also limited by its inability to demonstrate internal joint structures, including cartilage, labrum, capsule, and surrounding periarticular soft tissues.4–6
Many radiographic projections can be used in investigation of the hip; these are variably selected depending on the nature of the pathology and on the anatomic regions of concern. Standard imaging protocols have been established to ensure consistent positioning and optimal visualization of regions of interest.7–9
Anteroposterior (PA) Pelvis
Positioning: Patient supine (standing for dysplasia); feet internal rotation 15 degrees
Indications: all pathologies, including trauma, congenital dysmorphisms, and arthritis

Figure 31-1 Anteroposterior (AP) view of the pelvis. The femurs are held in 15 degrees of internal rotation, and the x-ray beam is centered at the midpoint between the superior margin of the symphysis pubis and at the midpoint between the anterior superior iliac spines (ASISs).
Judet (Oblique) Views
Frog-Leg Lateral
Cross-Table Lateral
Dunn View

Figure 31-2 Dunn projection, 45 degrees. The hip is held in 45 degrees of flexion and 20 degrees of abduction with the x-ray beam centered and the midpoint between the anterior superior iliac spine (ASIS) and the symphysis pubis.
False Profile View
X-ray technique: x-ray beam perpendicular to cassette, centered at femoral head
Structures of interest: acetabular coverage of femoral head anteriorly, posterior joint space

Figure 31-3 False profile view of the right hip. The patient is standing with the body rotated 65 degrees, with the right side rotated posteriorly toward the cassette. The x-ray beam is centered at the femoral head.
Computed Tomography
Computed tomography (CT) is a modality that allows accurate depiction of hip joint anatomy and many pathologies. It can provide very high spatial resolution images, revealing detailed information on osseous morphology, alignment, and integrity. CT acquires images in the axial plane, although images in the coronal, sagittal, and other oblique planes can be secondarily constructed by software reformation. Three-dimensional (3D) volume surface shaded images, models, and rotational series can be generated using advanced computer software algorithms. These postprocessing algorithms and filters can be applied to selectively optimize evaluation of the bones or soft tissues. Various structures, including bone, soft tissue, and even hardware, can be subtracted or emphasized with postprocessing techniques. The acquisition time of a CT scan is very short; thus motion artifacts are not significant.
Indications for CT evaluation of the hip include acute trauma (fracture, dislocation, intra-articular bodies, preoperative planning), treatment follow-up (healing assessment, joint congruity, hardware fixation devices), characterization of mineralized components of bone and soft tissue tumors and neoplasms, and characterization of congenital/developmental abnormalities.
In certain situations and pathologies, CT can be used to diagnose and characterize hematomas, fluid collections, and gross changes of inflammation and infection. However, it should be noted that compared with MRI, CT has relatively lower contrast resolution, which can limit evaluation of nonosseous and nonmineralized articular and periarticular structures and soft tissues of the hip. A potential concern with CT is the radiation dose that patients receive, especially to the gonads. Therefore, CT parameters should be optimized to minimize the radiation dose to the patient, with consideration of the degree of detail required given the clinical situation.
CT may be combined with intra-articular injection of iodinated contrast agents (CT arthrography) to assess labral and chondral integrity and to detect intra-articular bodies,6,10,11 although this is done only when MRI is contraindicated.
Magnetic Resonance Imaging
MRI offers exquisite contrast resolution, allowing optimal characterization of nonosseous and nonmineralized articular and periarticular structures, including labrum, cartilage, joint space, capsule, marrow space, and regional soft tissues.3,12,13 It can assess compact and cancellous bone as well, although sometimes not as accurately as CT.
MRI has multiplanar image acquisition capability. Images in standard axial, sagittal, coronal, or any oblique planes can be directly acquired or secondarily constructed with the use of postprocessing reformation software. Recent technological advances in MRI field strength and sequence protocols allow the preparation of 3D sequences with fairly high resolution. It is important to note that MRI does not involve ionizing radiation.
Indications for MRI of the hip are broad because of its ability to evaluate both osseous and regional soft tissue structures. Indications include trauma (detection of radiograph and CT occult fractures and stress or insufficiency fractures), avascular necrosis (AVN), bone marrow edema syndromes (transient osteoporosis, migratory osteoporosis), oncology (detection and characterization of lesions), arthritis (detailed cartilage assessment), internal joint derangement (labral evaluation), osseous deformity (femoroacetabular impingement, hip dysplasia), infection (joint, bone, surrounding soft tissues), myotendinous injury, and soft tissue inflammation (bursitis).
The combination of MRI with intra-articular injection of gadolinium-based contrast agents—direct magnetic resonance arthrography (MRA)—is often used to facilitate evaluation of small structures in the hip joint, including labrum, hyaline cartilage, and intra-articular bodies. The distention effect of the arthrogram may cause separation of capsular, labral, and osteochondral structures, resulting in increased spatial resolution. Injected contrast solution outlines both normal anatomic structures and abnormal pathologies, further improving contrast resolution and increasing the conspicuity of intra-articular pathology (Fig. 31-4A–C).14,15
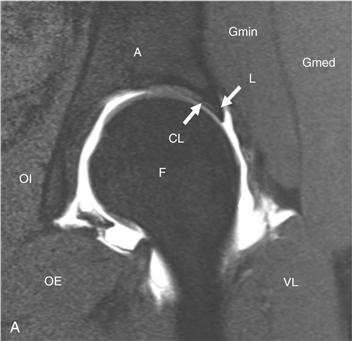
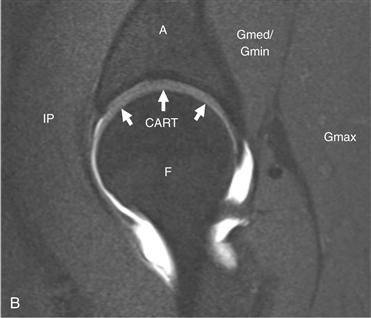
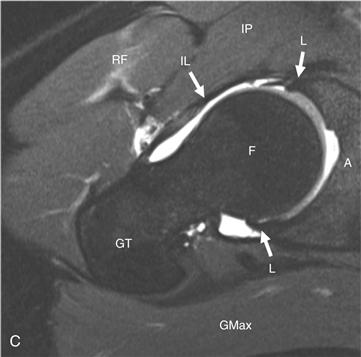
Figure 31-4 A through C, Direct magnetic resonance arthrography (MRA) T1-weighted images with fat suppression in the (A) oblique coronal, (B) oblique sagittal, and (C) oblique axial planes, with key anatomic structures labeled. A, Acetabulum; CART, hyaline cartilage; CL, chondrolabral junction; F, femoral head; Gmax, gluteus maximus; Gmed, gluteus medius; Gmin, gluteus minimus; IL, iliofemoral ligament/anterior capsule; IP, iliospsoas; L, labrum; OE, obturator externus; OI, obturator internus; RF, rectus femoris; VL, vastus lateralis.
Indirect MRA involves intravenous injection of gadolinium contrast, followed by a variable delay and/or physical activity regimen. Gadolinium contrast will distribute within the joint space, diffusely enhancing the synovial fluid.16 This will provide greater contrast resolution between joint fluid and labrum, cartilage, and capsule. The benefit of indirect MRA is that it is less invasive for the patient and does not require fluoroscopically guided joint injection. However, the distention effect that direct MRA provides is not realized. Enhancement of background extra-articular soft tissues and vascular structures, both normal and pathologic, will also be noted. This may make articular pathology less conspicuous.
MRI pulse sequence selection depends on the technique used; multiple, variable combinations of sequence classes can provide equally diagnostic studies. Spin echo, fast spin echo, and gradient recalled echo sequences can be used in the MRI investigation of hip pathology. Three-dimensional volume and isotropic voxel acquisitions with multiplanar reformations have become feasible in terms of time and imaging quality and can be applied to MRI and MRA of the hip.3 Multiplanar imaging with at least one sequence or reformation in each plane should be standard.
For nonarthrographic MRI, the protocol should include T1-weighted (T1W) imaging without fat suppression to demonstrate anatomy, joint alignment, marrow abnormality, or fracture. A fluid-sensitive sequence (T2W or proton density[PD]W) with fat suppression, or short tau inversion recovery (STIR), should always be part of any protocol to detect abnormal edema within marrow and soft tissues, as well as periarticular fluid collections or cysts.17 In addition, fluid-sensitive sequences increase the contrast between joint fluid and adjacent labrum, cartilage, bone, and capsule. With nonarthrographic MRI studies, higher resolution and an increased number of sampling averages13,18 are used; this may offset the lower contrast and spatial resolution of MRI compared with MRA.
With direct MRA, the most commonly used sequence is T1W, with or without fat suppression, in addition to fluid-sensitive sequences.16 With indirect MRA, the same sequence selection as for direct MRA is adequate, although with a few caveats. Fat suppression is strongly advised for maximal contrast resolution because the concentration of gadolinium within the joint may not be as high as with direct injection. As well, multiphasic imaging may be considered to understand the vascular physiology of the joint.16
Drawbacks of MRI include relatively longer acquisition times, susceptibility to motion artifacts, magnetic susceptibility artifacts due to regional metal prostheses, and/or postsurgical artifacts, along with several other absolute and relative contraindications (claustrophobia, non–MRI-compatible prostheses, some makes of electronic implanted devices and cardiac pacer equipment, orbital metal bodies).
Ultrasound
Ultrasound (US) is not as widely used as other modalities in radiologic investigation of the adult hip. It is very important in the pediatric hip for evaluation of developmental dysplasia. US is limited to assessment of soft tissues, fluid structures, and nonmineralized structures. It can detect the presence of an effusion, synovitis, and capsular thickening. As well, tendon abnormalities such as tendinosis, tenosynovitis, or tears can be diagnosed. US may also assess regional soft tissues for muscle tears, fluid collections, and bursitis. US is unique in that it allows dynamic, real-time visualization of periarticular structures with patient feedback. No parameters for US of the hip have been defined, although a high-frequency linear transducer should be used for high-resolution imaging of periarticular soft tissues. It is important to note that no ionization radiation is associated with US. However, US may be limited by patient habitus such as obesity, it can be operator dependent, and, unlike other modalities, it does not provide any gross information on regional osseous structures.
Nuclear Medicine
Nuclear medicine studies may be useful in providing insight into the physiologic state of the hip joint. A radioactive compound is injected into the bloodstream; this is followed by a variable imaging regimen. Several protocols and various radiotracers can used in isolation or in combination to generate images that track the flow and accumulation of tracers. Although traditionally two-dimensional (2D) images were acquired, 3D datasets can be obtained with the use of multiple rotational detectors, yielding greater spatial information. Indications for nuclear medicine studies include trauma (detection of occult acute and stress fractures), AVN, infection, and oncologic workup.
Femoroacetabular Impingement
Femoroacetabular impingement (FAI) has become a well-recognized pathogenic factor in the evolution of hip osteoarthritis (OA). The impingement is secondary to anatomic abnormalities of the femoral head-neck junction and/or the acetabulum. These dysmorphisms lead to impaired, pathologic interaction of the femur with the acetabulum during motion of the hip joint, resulting in altered biomechanics and premature degeneration of hyaline cartilage, and eventually to OA.19–23 Given that the impingement results from underlying structural aberrations, radiologic imaging is essential in the investigation of FAI. Imaging provides a visual presentation of the primary deformities, as well as the secondary joint derangements, that can result from FAI in both cam and pincer forms. It is known that most patients with FAI in fact have a variable combination of both forms of impingement. Radiography,19,24,25 CT,23 and MRI13,14,22,26,27 are validated modalities for imaging the hip in the setting of FAI. Characteristic radiographic morphologic features of both the femur and the acetabulum can facilitate, expedite, or confirm the diagnosis of clinically suspected FAI, even before gross osteoarthritic changes evolve.
Primary Anatomic Abnormalities of Femoroacetabular Impingement
Cam Femoroacetabular Impingement
In the cam form of FAI, the main dysmorphism is of the femoral head-neck junction. An excess of bone and/or cartilage bulk at the anterosuperior femoral head-neck junction results in reduced offset of the femoral head over the neck and femoral head asphericity.19,20,22,28,29 The abnormality can also be described as an osteochondral bump or excrescence, lack of head-neck concavity, diminished offset, or reduced wasting of the head-neck junction.21
The cam deformity can be identified on several radiographic projections. The optimal projection is the flexion abduction view (Dunn), which demonstrates the anterosuperior femoral head-neck junction in profile, followed by the cross-table lateral. The AP view may underestimate or even miss a cam deformity.24 Depending on the size and location of the cam deformity, and on the position of the femur, it may manifest on AP radiograph as an abnormal convexity along the lateral femoral head-neck junction, resembling the hand grip of a pistol.25
CT and MRI with their multiplanar capabilities are more sensitive than radiography in the detection of subtle osseous deformities.1–3 The oblique axial plane, parallel to the long axis of the femoral neck, is the imaging plane most frequently used to evaluate the femoral head-neck junction. This plane optimally images the anterior contour of the femoral head-neck junction. However, several studies have reported that, although present anteriorly, diminished offset is most pronounced anterosuperiorly and potentially at any location within the anterosuperior quadrant.27,28,30 Thus radial images, obtained using the femoral neck as the axis of rotation, have been recommended as a method for evaluating the femoral head-neck junction over its full circumference, as opposed to just anteriorly, as occurs when the more conventional oblique axial plane method is used.13,22,23,27,30 Radial images are based on a rotating plane such that each image is orthogonal to the femoral surface and visualizes the head-neck junction in profile. A clock face nomenclature can be applied for localization around the femoral head-neck junction, with superior and anterior locations designated 12 o’clock and 3 o’clock, respectively.
The alpha angle is a parameter used to qualify and quantify the cam deformity.14,26 Previous studies show that an elevated alpha angle is associated with symptomatic impingement.14,23,26,27 It can be measured on radiography, CT, or MRI on any plane. The alpha angle is determined by first drawing a best-fit circle around the perimeter of the femoral head. The first arm of the angle is the long axis of the femoral neck, defined as the line drawn between the center of the femoral neck at its narrowest point and the center of the best-fit circle. The second arm of the angle is drawn from the center of the circle anteriorly to the point where the head extends beyond the margin of the circle.26 Larger cam deformities will yield larger alpha angle values (Fig. 31-5).
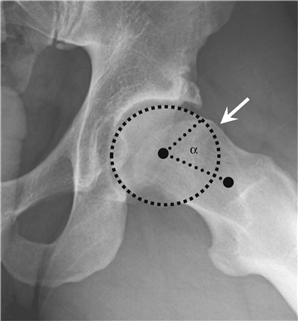
Figure 31-5 Dunn view (45 degrees) demonstrating a cam deformity with an elevated alpha angle of 74 degrees.
Several studies have proposed absolute thresholds (ranging from 50 to 55 degrees) for calling an alpha angle abnormal.23,26 In symptomatic cam-type FAI patients, the mean alpha angle value found in several studies ranges from 66.4 to 74.0 degrees.14,23,26,28 There is a range of normal values for the alpha angle. In asymptomatic patients, the alpha angle ranges from 39.3 to 48.3 degrees.23,26,31,32 In the normal hip, the mean alpha angle value in males and females, anteriorly, has been reported to be 44.0 degrees and 38.1 degrees, respectively, while anterosuperiorly, it was 54.1 degrees and 47.0 degrees, respectively.32 Thus, depending on which location around the femoral head-neck junction is being evaluated, and on the gender of the patient, threshold values for the alpha angle considered to be abnormal may have to be varied.
Anterior offset is another validated parameter for quantifying reduced offset of the femoral head on the neck. It is best measured on a cross-table lateral radiograph or on any radial CT or MRI view. A line is drawn parallel and tangential to the anterior cortex of the femoral neck. A second, parallel line is drawn tangential to the most anterior aspect of the femoral head. The perpendicular distance between these two lines is the anterior offset. In asymptomatic hips, the mean offset is 11.6 mm, and in cam FAI hips, offset is reduced to 7.2 mm. To normalize for patient size, the offset ratio can be calculated; this is the ratio between the anterior offset and the femoral head diameter. The mean offset ratio is 0.21 in asymptomatic hips; in cam FAI hips, it is 0.13.25,33
Pincer Femoroacetabular Impingement
In the pincer form of FAI, the primary abnormality is of the acetabulum. The impingement is the result of overcoverage of the femoral head by the acetabulum. This may be related to acetabular retroversion, coxa profunda, or acetabular protrusion.19,20,22
Acetabular retroversion causes focal overcoverage of the femoral head, and coxa profunda and acetabular protrusio result in more global overcoverage. All result in relative deepening of the acetabular fossa. These dysmorphisms lead to abnormal abutment of the femoral neck against the overcovering acetabulum, resulting in a linear zone of impingement anterosuperiorly, and shifting of the femoral head posteriorly.20,21 This latter phenomenon may lead to a predilection for posteroinferior joint space narrowing and OA.
The version of the acetabulum refers the orientation of the opening of the acetabular fossa relative to the sagittal plane. In the normal hip, the opening of the acetabular fossa is directed anteriorly, or is anteverted. With retroversion, the acetabular fossa is oriented posteriorly.21,34,35 Although this abnormality is best evaluated with the use of cross-sectional modalities such as CT or MRI, radiographs can detect gross morphologic features of the acetabulum that predispose to pincer impingement. On an AP pelvis radiograph, with acetabular retroversion, the superoanterior acetabular rim abnormally sits more lateral than the posterior rim. Crossing of the anterior rim margin laterally over the posterior rim gives a figure-of-eight density, referred to as the crossover sign.25 Retroversion may also manifest as a deficient posterior wall, where, on an AP radiograph, the posterior rim of the acetabulum projects medial to the center of the femoral head25 (Fig. 31-6).

Figure 31-6 Anteroposterior (AP) view of the left hip with signs of acetabular retroversion. The superior portion of the anterior rim of the acetabulum (dotted line, more horizontal) abnormally projects lateral to the superior portion of the posterior rim (dashed line, more vertical), resulting in “crossover.” Note that the posterior rim of the acetabulum lies medial to the center of the femoral head (solid dot). Retroversion also results in medialization and a prominent profile of the ischial spine (white arrow).
Acetabular version is best evaluated on axial plane images,36 whether by MRI or CT. CT, with its better depiction of compact bone, may allow more accurate delineation of the exact margins of osseous landmarks. The entire transverse dimension of the osseous pelvis, with both hips in the field of view, is required to correct for any positional tilt of the pelvis.
The normal acetabulum is anteverted by 20 to 23 degrees,34,37,38 with 15 to 25 degrees generally considered to be within normal limits. On axial images through the retroverted acetabulum, the anterior acetabular rim sits more lateral than the posterior rim.34 The orientation of the acetabular version is not fixed at all levels. A natural decrease in the degree of anteversion is noted, progressing from superior to inferior.34,36,39 It has been suggested that the version of the acetabulum should be evaluated at the level through the mid femoral head, on the image where the diameter of the femoral head is largest,34,36 or on the image where the head is most congruent with the acetabulum.39
Acetabular overcoverage can be global, resulting from increased depth of the acetabular fossa. Normally, the medial acetabular fossa line should be lateral to the ilioischial line. Coxa profunda is present when the fossa acetabuli line lies medial to the ilioischial line (Fig. 31-7A). Acetabular protrusio occurs when any portion of the femoral head sits medial to the ilioischial line25 (Fig. 31-7B).
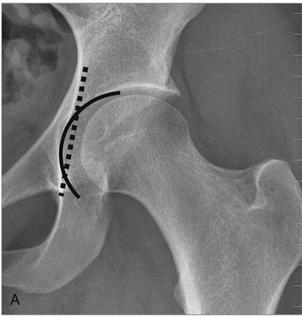
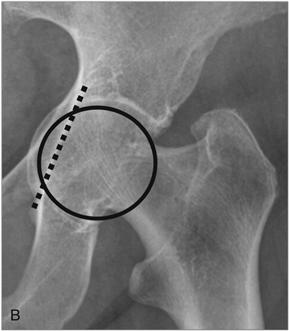
Figure 31-7 Anteroposterior (AP) radiographs of the hip demonstrate (A) coxa profunda—the fossa acetabuli line (solid line) lies medial to the ilioischial line (dashed line), and (B) acetabular protrusio—the femoral head (solid line circle) lies medial to the ilioischial line (dashed line).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







