Iliofemoral Pseudoarthrosis and Arthrodesis
Nicola Fabbri
Mary I. O’Connor
Mario Mercuri
Franklin H. Sim
The treatment and prognosis of musculoskeletal neoplasms have dramatically improved during the past three decades. However, the surgical management of malignant pelvic tumors remains a challenging problem from both oncological and functional standpoints. With respect to tumor control, a limb salvage procedure has been shown to be a reliable alternative to hemipelvectomy when an adequate surgical margin can be obtained or when an amputation does not provide a better margin (1,2,3,4). In general, if chances of tumor local control are the same, a limb sparing procedure is preferable because it usually is associated with superior function than hindquarter amputation and prosthetic fitting (5,6). In this setting, postoperative function depends upon tumor location, extent of resection, and whether pelvic stability, defined as the ability to withstand physiologic loading, is maintained or restored at the time of surgery (3). The best functional results are usually seen when pelvic stability is maintained, either by preservation or by surgical reconstruction of effective load transmission through femorosacral continuity (3,7).
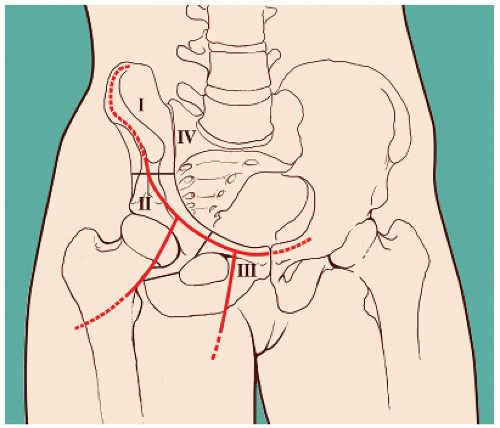
A schematic approach to pelvic anatomy and classification in four regions (2,3) is helpful in order to visualize these concepts (Fig. 2.1). In resections involving the ischiopubic region (region III) or incomplete resections of the ilium (region I), the continuity between the femur and the ipsilateral sacrum is maintained along with an essentially normal weight-bearing capability. In these circumstances, bone reconstruction is usually not required and functional results are uniformly quite satisfactory (1,2,3,4). Management of a malignant tumor involving the acetabulum (region II) is in general a more complex surgical challenge for the following reasons:
TUMOR EXTENSION
Lesions are usually of larger size and often extending into region I and/or region III, requiring a wider exposure and a more extensive dissection.
PROXIMITY TO NEUROVASCULAR STRUCTURES AND VISCERA
Anteriorly, external iliac and femoral artery and vein and the femoral nerve have to be adequately exposed and mobilized in order to gain access to the inner portion of the pelvis and medial wall. Posteriorly, exposure of the greater sciatic notch and sciatic nerve is mandatory to approach supra- and retro acetabular areas. Depending upon medial soft tissue extension and region III involvement, considerable work may be necessary to dissect the retropubic space, including urethra, urinary bladder, and ipsilateral ureter.
PELVIC STABILITY AND RECONSTRUCTION
Resection of the acetabulum by definition causes femorosacral discontinuity and pelvic instability. In terms of function, creation of a flail hip remains a better option than hemipelvectomy but is often associated with considerable disability. Reconstruction should be therefore at least considered in these instances in order to restore stability and improve function.
INDICATIONS
Selection of the reconstructive technique is a very important step in the overall management and is based on careful evaluation of numerous factors related to
Patient characteristics
Tumor features
Surgeon’s experience and preference
The role of the above factors in the selection of optimal technique may be summarized as follows:
Patient Characteristics
Age, Functional Demands, and Expectations Skeletal immaturity is relevant because of the patient’s size and growth potential, usually discouraging the use of massive implants and suggesting a more biologic approach. Potential for recreational activities, type of employment, and required level of function, namely the capability to weight bear and sustain load, are important considerations at any age.
Overall Medical Condition and Relationship With Tumor Prognosis Careful assessment of the general medical condition is important when facing a usually long and demanding procedure, sometimes associated with severe postoperative complications. Particularly, the presence of an immunocompromised status, as it occurs during multiagent chemotherapy, and other relatively common comorbidities, such as diabetes and obesity, has to be kept in mind because of the increased risk of infection.
Tumor Features
Diagnosis, Stage, and Prognosis Important considerations related to the tumor are the need for chemotherapy and/or radiotherapy and the presence of distant metastasis. While previous radiation therapy dramatically increases the risk of wound problems and infection, delay in resuming chemotherapy because of postoperative complications may severely impact survival. In these instances, an effort should be made to minimize morbidity of surgery. Not uncommonly, a patient presenting with pelvic sarcoma and lung metastasis may still be a candidate for surgery. Particular attention should then be paid to minimize the risks of surgery, maximize the role of adjuvant medical management, and focus on quality of residual life.
Tumor Location, Type of Resection, and Extent of Surgery Reconstructive technique may vary depending upon tumor extension and type of resection. Tumor involvement of zone I requiring partial or complete resection of the ilium and soft tissue involvement are important factors to consider. In fact, while iliac resection reduces the bone available for fixation, involvement and resection of the gluteus medius and/or superior gluteal nerve will cause loss of active abduction.
Surgeon’s Experience and Preference
Level of training and personal experience of the surgeon also play a relevant role. Common sense is as important as technical skills in pelvic surgery and avoidance of possibly catastrophic complications may outweigh
the potential functional benefit associated with a massive implant, such as a mobile hip and the absence of substantial limb shortening.
the potential functional benefit associated with a massive implant, such as a mobile hip and the absence of substantial limb shortening.
 FIGURE 2.2 Example of flail limb after resection of the whole hemipelvis and proximal femur (P1,2,3,H1). |
A detailed description of advantages and disadvantages pros of each technique is beyond the purpose of this chapter; however, a brief outline of the main inherent features is pertinent to the subject discussed.
Overview of Surgical Options
Various surgical options are available today following pelvic resection for a tumor involving the acetabulum. They can be schematically divided in three groups:
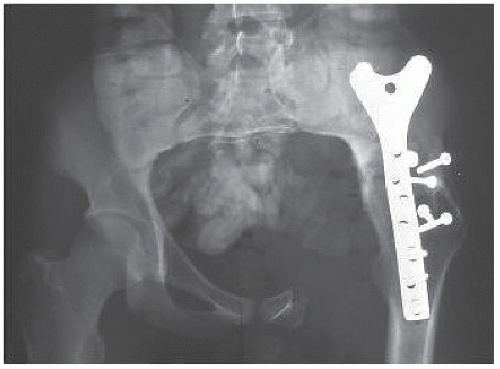
Flail Hip, Hip Transposition to Sacrum Flail hip (Fig. 2.2) is at the opposite end of the concept of pelvic stability and has been historically associated with significant limb shortening and substantial disability (2,3,8,9). Recent literature has reported excellent results in a subgroup of young patients, emphasizing the role of careful soft tissue reconstruction and prolonged rehabilitation as key for success (10). Hip transposition to the sacroiliac joint has been also described following resection of the whole hemipelvis (11). According to the authors, a stable pseudoarthrosis between the sacrum and the femur is obtained using a polyethylene terephthalate mesh tube (Trevira; Implantcast, Buxtehude, Germany) to augment soft tissue reconstruction and create a neo-joint capsule (Fig. 2.3). Functional and quality of life assessment indicate superior outcome of this technique when compared to prosthetic replacement and amputation (11).
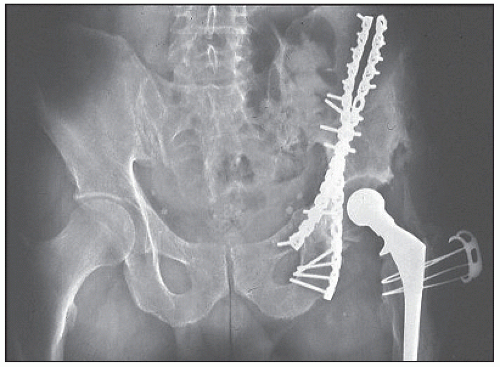
Iliofemoral Arthrodesis and Pseudoarthrosis, Ischiofemoral Arthrodesis and Pseudoarthrosis Iliofemoral and ischiofemoral arthrodesis or pseudoarthrosis have been employed successfully for many years in limb salvage for malignant pelvic tumors (1,2,3,4). The basic principle of both techniques is to obtain continuity of the hip with residual pelvis, by either fusion or coaptation, improving pelvic stability and weight-bearing potential (Figs. 2.4 and 2.5). Stability of the construct and functional results are depending upon the amount of pelvic bone left after resection. Both options are associated with limb shortening,
usually less severe in ischiofemoral techniques. Because intrinsically more stable, however, iliofemoral reconstructions have been predictably associated with better functional results than ischiofemoral reconstructions, which have lost popularity during the last 2 decades. Limb shortening, usually ranging 3.5 to 6 cm, may be easily compensated by a shoe lift without major impact on function (12).
usually less severe in ischiofemoral techniques. Because intrinsically more stable, however, iliofemoral reconstructions have been predictably associated with better functional results than ischiofemoral reconstructions, which have lost popularity during the last 2 decades. Limb shortening, usually ranging 3.5 to 6 cm, may be easily compensated by a shoe lift without major impact on function (12).
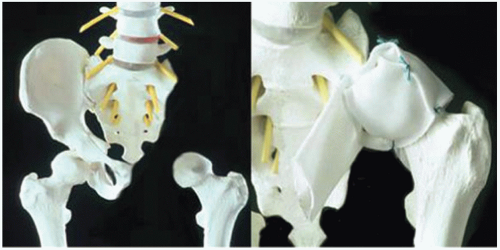 FIGURE 2.3 Hip transposition to the sacrum has been described following resection of the whole hemipelvis (11). A stable pseudoarthrosis between the sacrum and the femur is obtained using synthetic material. (Reprinted from Hoffmann C, Gosheger G, Gebert C, et al. Functional results and quality of life after treatment of pelvic sarcomas involving the acetabulum. J Bone Joint Surg Am. 2006;88:575-582.) |
Massive Implants (Pelvic Allograft or Allograft-Prosthetic Composite, Autoclaved or Irradiated Autograft, Pelvic Prosthesis, Saddle Prosthesis) The use of massive implants to restore hip motion and more physiologic function has been also pursued with enthusiasm in many centers more recently (Figs. 2.6, 2.7, 2.8). However, while good function in this setting has been reported mainly for allograft-prosthetic composite and occasionally for pelvic prosthesis, an high incidence of severe complications including infection, graft fracture, hip instability, and need for secondary hindquarter amputation has been associated with all these techniques (13,14,15,16,17,18,19).
Indications for Iliofemoral Arthrodesis and Pseudoarthrosis
The ideal candidate for iliofemoral fusion, either arthrodesis or pseudoarthrosis, is a patient requiring a type II or type II and III pelvic resection in which the proximal osteotomy through the ilium is close to the acetabulum. Availability of most of the ilium minimizes limb length discrepancy and allows wider bone contact and solid fixation, enhancing either fusion in iliofemoral arthrodesis or hip stability when pseudoarthrosis is preferred (12). In arthrodesis, rigid fixation is usually achieved with a plate, while cable wires or heavy mersilene sutures are used for pseudoarthrosis (1,3,12).
Iliofemoral fusion is preferable for young and active patients because it provides stable and durable construct capable to withstand high-demand functional requirements. Iliofemoral pseudoarthrosis appears indicated for more sedentary and older patients. Although the construct is less stable than iliofemoral fusion, maintaining the ability to flex the hip seems to be appreciated by older patients with a more sedentary lifestyle (1,12). In addition, iliofemoral pseudoarthrosis is usually a shorter and technically less demanding procedure possibly associated with a lower complication rate than iliofemoral pseudoarthrosis, features particularly appealing in older patients. When the proximal osteotomy is above the neck of the ilium, the iliac wing becomes thin, and obtaining solid fixation and fusion may be very difficult because of reduced bone contact and inadequate screw fixation. In this instance, iliofemoral arthrodesis is less than ideal while pseudoarthrosis remains a viable option (1,12).
CONTRAINDICATIONS
Extension of the tumor in zone I and inadequate iliac bone stock after the resection is the most important and common contraindication to iliofemoral arthrodesis. When the entire ilium is resected with the acetabulum, as it occurs in type I and II and type I to III resections, a different surgical strategy has to be considered to maximize function in the light of the overall clinical scenario. Flail limb, ischiofemoral arthrodesis or pseudoarthrosis, or a massive hemipelvic implant may be selected based on the factors previously discussed.
The need to sacrifice the sciatic or femoral nerve because of tumor involvement is not per se a contraindication to limb salvage surgery in general nor to iliofemoral arthrodesis or pseudoarthrosis in particular. However, since the rationale for undertaking limb salvage surgery is providing superior function than external hemipelvectomy, a realistic evaluation of the postoperative function versus perioperative complications is crucial in this setting.
PREOPERATIVE PLANNING
Tumor control remains the first priority of surgery and correlates with achievement of adequate surgical margin (1,2,3,20,21,22,23). The minimum surgical margin required for tumor control is a wide margin, which implies en bloc removal of the tumor completely surrounded by normal tissue (24). The goal of preoperative planning is to ensure the best chances to obtain an adequate margin and a stable reconstruction minimizing the risk of complications.
Successful preoperative planning is in our opinion based on three main steps:
Physical Examination and Staging Studies Review
Thorough review of the regional anatomy and careful evaluation of good quality recent staging studies are mandatory. History and physical examination may provide important clues such as limb edema, urinary symptoms, sciatic or out of proportion regional pain, possibly suggesting deep venous thrombosis or involvement of adjacent visceral or neurologic structures. The presence of previous incisions for abdominal or pelvic procedures (e.g., hernia repair, caesarian section) should be noted and taken into account as potential problem because of scarring and sometimes interference with ideal incision line. Because of the need to excise the biopsy track en bloc with the tumor (24,25,26), evaluation of the biopsy site is also important. A poorly
performed biopsy complicates surgical management, often requiring modification of the incision and surgical conduct in order to obtain an adequate margin (3



performed biopsy complicates surgical management, often requiring modification of the incision and surgical conduct in order to obtain an adequate margin (3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree