and Gautam M. Shetty2
(1)
Consultant Joint Replacement Surgeon Department of Orthopaedic Surgery, Breach Candy Hospital, Mumbai, Maharashtra, India
(2)
Consultant Arthritis Care and Joint Replacement Surgery, Asian Orthopedic Institute Asian Heart Institute and Research Center, Mumbai, Maharashtra, India
Abstract
Hyperextension deformity is uncommon in arthritic knees undergoing total knee arthroplasty (TKA), occurring in less than 5 % of patients. In a recent study by the authors, the overall incidence of hyperextension in arthritic knees undergoing TKA was 3.9 % (45/1,150 limbs). Hyperextension can be encountered in patients with valgus deformities and excessive ligamentous laxity, in patients with rheumatoid arthritis (RA), in patients post high tibial osteotomy (HTO) and in patients with neuromuscular disorders such as poliomyelitis. The results of our study indicated that the majority of patients with hyperextending, arthritic knees suffered from primary osteoarthritis (78 %) and 58 % of the limbs had an associated preoperative varus deformity compared to 42 % which had a valgus deformity.
Introduction
Hyperextension deformity is uncommon in arthritic knees undergoing total knee arthroplasty (TKA), occurring in less than 5 % of patients [1–3]. In a recent study by the authors [3], the overall incidence of hyperextension in arthritic knees undergoing TKA was 3.9 % (45/1,150 limbs). Hyperextension can be encountered in patients with valgus deformities and excessive ligamentous laxity, in patients with rheumatoid arthritis (RA), in patients post high tibial osteotomy (HTO) and in patients with neuromuscular disorders such as poliomyelitis [4–6]. The results of our study indicated that the majority of patients with hyperextending, arthritic knees suffered from primary osteoarthritis (78 %) and 58 % of the limbs had an associated preoperative varus deformity compared to 42 % which had a valgus deformity [3].
Treating a hyperextending, arthritic knee with TKA could be challenging due to associated coronal plane deformities (varus or valgus), bony abnormalities such as reverse sloping of the tibial plateau and significant medio-lateral instability which may lead to difficulty in achieving a stable, well-balanced knee and the possibility of recurrence postoperatively [1–3]. Surgical techniques to deal with hyperextension during TKA includes posterior capsular plication, proximal and posterior transfer of the collateral ligaments, tightening the extension gap using thicker inserts, under-resecting the bone, undersizing the femoral component, using distal femoral augmentation blocks and using a constrained prosthesis [1–3, 7]. However, the technique of under-resection of tibia and femur, over-resection of the posterior surfaces of the femur, using a smaller femoral size with bone resection being done first and ligaments being balanced later will usually result in a stable, well-balanced knee [2, 3]. This chapter aims to outline the means of tackling hyperextension deformity during TKA.
Pathoanatomy
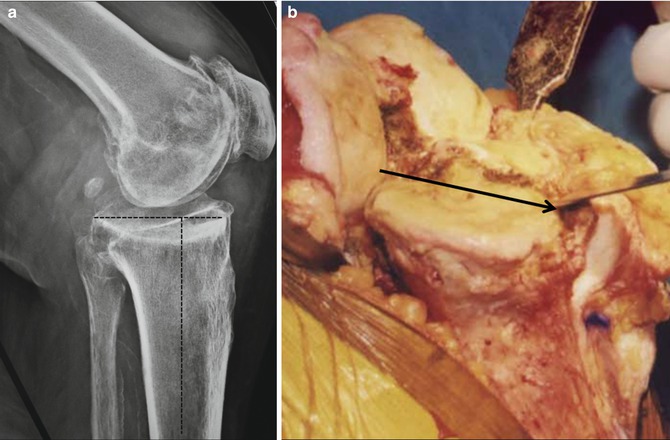
Arthritic knees with hyperextension have certain characteristic pathoanatomic features which need to be considered while performing a TKA. These are typically soft-tissue and bony abnormalities. Among the soft tissues, the posterior capsule is usually overstretched, causing hyperextension at the knee joint. This is associated with attenuation of the cruciate and collateral ligaments. These structural changes convert the posterior soft-tissue structures of the knee joint into a “hammock” (Fig. 6.1a) which needs to be made taut in order to correct this sagittal plane deformity and restore soft-tissue balance. In knees with associated valgus deformities, the iliotibial band may be contracted and anteriorly displaced which may accentuate the hyperextension deformity.
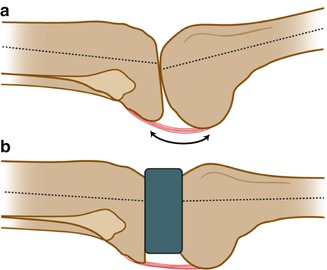
Fig. 6.1
Effect of posterior soft-tissue laxity and attenuation (posterior capsule particularly) in hyperextension deformity. (a) Overstretching and attenuation of the posterior capsule of the knee joint converts the posterior soft-tissue structures into a “hammock” in hyperextension deformities. (b) Owing to this attenuation of posterior soft-tissue structures, the resultant extension gap is much larger (compared to the flexion gap) in hyperextension deformity. Note that the tibial and the distal femoral bone cuts if too thick will significantly add to the already large extension gap
Owing to this attenuation of posterior soft-tissue structures, the resultant extension gap is much larger compared to the flexion gap in hyperextension deformities (Fig. 6.1b). Hence, standard resections of proximal tibia and distal femur will further widen this extension gap, resulting in severe extension-flexion gap mismatch and an excessively large extension gap requiring a very thick insert. Hence, one of the basic principles of treating hyperextension deformity during TKA is to resect minimal bone from both proximal tibia and distal femur and strictly avoid release of posterior soft-tissue structures. Apart from these soft-tissue changes, hyperextension may be accentuated by bony abnormalities such as decreased posterior slope or anterior sloping of the tibia or significant wear or bone loss on the anterolateral or medial aspect of the tibial plateau (Fig. 6.2a). In patients who have undergone a previous high tibial osteotomy, impaction of the anterior tibial cortex may also result in an anterior slope (Fig. 6.2b). In either scenario, the surgeon needs to be careful to not aggravate the bony abnormality by resecting the proximal tibia with a neutral slope or, worse, an anterior slope.