Chapter 6 Human Movement and Anterior Cruciate Ligament Function
Anterior Cruciate Ligament Deficiency and Gait Mechanics
INTRODUCTION
The anterior cruciate ligament (ACL) plays an important role in stability of the knee primarily through its passive constraint to anterior tibial translation and tibial rotation. In addition, the ACL influences the dynamic function of the knee. For example, ambulatory changes have been associated with functional adaptations after loss of ACL function. The nature of these functional adaptations may be considered a potential functional marker for the ability to return to vigorous activities3,28,29 as well as for secondary degenerative cartilage changes after ACL injury.7
The purpose of this chapter is
Differences in the manner in which patients adapt their gait characteristics to the loss of the ACL provide a possible explanation for the variable outcome after this injury. It is likely that some patients can dynamically adapt to the loss of an ACL, whereas others will not adapt. The large variation in treatment selection and outcome8,9 suggests a need for better methods of assessing the clinical and functional status of the patient after ACL rupture. Diagnostic methods for identifying a torn ACL have improved substantially; however, prognostic methods for assessing the probability of successful treatment are not yet available. Even quantitative laxity measurements obtained from devices such as the KT-1000 have not been predictive of clinical outcome.36 Thus, variability in dynamic adaptations achieved through alteration in the patterns of muscle firing1,23,34 during a particular activity provides a possible explanation for the differences in outcome of patients after ACL injury.
JOINT KINETICS DURING GAIT AND THE ACL-DEFICIENT KNEE
An analysis of the kinetics (forces and moments) that act at the knee during walking provides useful insight into the functional changes associated with the ACL-deficient knee. In particular, the moments that act at the knee suggest the cause and potential effect of gait changes after ACL injury. For example, a reduction in the intersegmental moment tending to flex the knee (balanced by net quadriceps contraction) during walking was among the first changes in walking mechanics reported in the ACL-deficient knee.10 The reduction of the net internal quadriceps moment is consistent with quadriceps muscle atrophy, which is frequently reported after ACL injury20 and helps to explain why it is difficult to restore quadriceps strength in these knees. Thus, it is useful to examine the physical meaning and relevance of the intersegmental moment at the knee during walking. This section provides a summary of the methods used to determine the joint moments, an example of how to interpret the magnitude and pattern of the flexion-extension moment at the knee in context of the function of the knee flexors and extensors during ambulation, and an example of how an analysis of the flexion-extension moment during walking can provide insight into the functional role of the ACL.
Critical Points JOINT KINETICS DURING GAIT AND THE ACL-DEFICIENT KNEE
Definition of Intersegmental Moment
A moment is a vector quantity that can be considered a rotational force (lever arm x force) in the sense that it tends to produce a rotation about a specific point. Whereas moments can be calculated at any point, it is useful to use the joints between adjacent limb segments to define the moments that act on the body during walking. For example, the moment acting at the knee would be the intersegmental moment between the thigh and the shank. The external moment tending to flex or extend the joint is illustrated in Figure 6-1. The intersegmental moments are typically calculated from measurement of the foot-ground reaction forces (using a force platform) and the motion of markers placed on the limbs using an optoelectronic system for motion capture. The weight and inertial forces are often approximated by modeling the leg as a collection of rigid segments representing the thigh, shank, and foot. The reader should be aware of the assumptions used in performing these calculations.5 Finally, the units of a moment are force and length. Therefore, it is useful when comparing different-sized subjects to express the intersegmental moments in nondimensional units by dividing the moment by the subject’s height (ht) and body weight (bw). Thus, moments measured during gait are often expressed in units of percentage of the product of the body weight and height (% bw x ht), so that moments can be compared among subjects of different heights and weights.
Interpretation of Intersegmental Moment
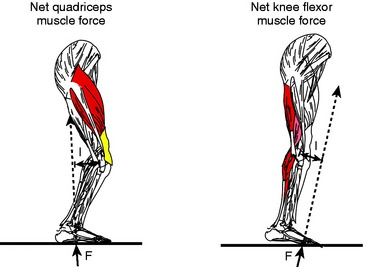
The moment can be visualized in the context of the direction of the ground reaction vector relative to the position of the knee joint center (see Fig. 6-1). If the vector passes anterior to the knee, the moment will tend to extend the knee, whereas if the vector passes posterior to the knee, the moment will tend to flex the knee. As noted previously, the direction of the moment can be used to infer the net muscular moment. Thus, an external moment tending to flex the knee will be balanced by a net quadriceps moment. Previous studies have demonstrated that the external moments measured can be interpreted in terms of the loads on muscles, passive soft tissue, and joint surfaces.32 In addition, the joint moments have been shown to be sensitive indicators of differences between normal and abnormal function.3,10,31
It is useful to examine the assumptions used as the basis for the interpretation of the joint moments during function. Mechanical equilibrium dictates that external forces and moments must be balanced by internal forces and moments. Internal forces generated by muscle, passive soft tissue, and joint contact force create these internal moments. If muscles act only synergistically when balancing the external moments, one could directly infer the internal muscle force in synergistic muscle groups. For example, the total force in the quadriceps needed to balance an external moment tending to flex the knee joint could be determined.32 However, if antagonistic muscle activity is present, the external moment reflects the net balance between agonist and antagonist muscles. The force in the synergistic muscle group would be greater under these conditions. The external moment can, however, be used to obtain a conservative estimate or lower bound on the synergist muscle force. Throughout this chapter, external moments are described from the measurements taken in the laboratory and inferences are made in terms of the net muscular moment (see Fig. 6-1).
The Flexion-Extension Moment and the ACL-Deficient Knees
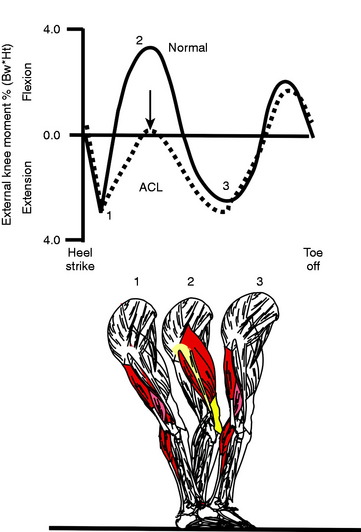
The normal temporal pattern of the flexion-extension moment during stance phase of walking can be interpreted in terms of the net quadriceps moment or net knee flexor muscle moment (hamstrings and/or gastrocnemius) during stance phase (Fig. 6-2). Typically, at heel strike, there is an external moment that tends to extend the knee joint, demanding a net knee flexor force. As the knee moves into midstance, the external moment reverses its direction, demanding a net quadriceps force. As the knee passes midstance, the moment again reverses its direction, demanding net flexor muscle force. Finally, in the pre-swing phase, the moment tends to flex the knee, demanding a net quadriceps muscle force. As previously noted, a reduction of the net quadriceps moment relative to normal is frequently seen in ACL-deficient subjects during level walking (see Fig. 6-2). Specifically, ACL-deficient subjects walk in a manner that has been interpreted as a tendency to avoid or reduce the demand on the quadriceps muscle.10 Whereas the reduction in net quadriceps moment can be interpreted as either a reduction in the quadriceps or an increase in the knee flexor muscle moment, the fact that quadriceps atrophy is a common finding after ACL injury20 supports the conclusion of a reduction in quadriceps contraction during walking.
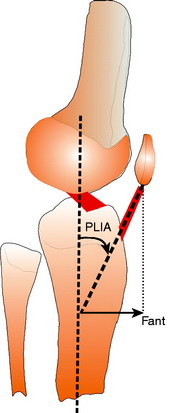
The mechanics of the knee extensor mechanism suggests a possible cause for the inhibition of quadriceps contraction during walking. As illustrated in Figure 6-3, the anterior angulation of the patellar ligament insertion angle (PLIA) causes an anterior force to be applied to the tibia when the quadriceps contracts. In the absence of the ACL, the tibia moves forward when the quadriceps contracts until the force is balanced by other secondary restraints to anterior tibial displacement, such as the medial collateral ligament, meniscus, or a hamstrings contraction. Thus, more anterior tibial translation could occur in ACL-deficient knees than in uninjured knees when the quadriceps contracts. The amount of anterior force is greatest at full extension because the PLIA has the largest anterior angle at full extension and this angle reduces as the knee flexes.17,25 Thus, walking would produce a substantial component of anterior force owing to quadriceps contraction because the knee remains near full extension throughout stance phase, with maximum flexion angles less than 30°. A reduction in quadriceps contraction could eliminate large anterior tibial translations near full extension and prevent sensations of joint instability by the patient.
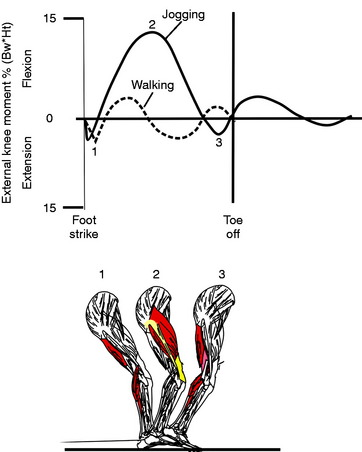
Interestingly, the magnitude of the net quadriceps moment can increase by more than a factor of 5 during jogging as compared with level walking (Fig. 6-4), yet the percentage change in the net quadriceps moment between ACL-deficient and normal subjects is substantially less during jogging than during walking.10 The fact that the maximum net quadriceps moment during jogging occurs when the knee is at approximately 40° of flexion, as compared with 20° during level walking, might provide an explanation for the fact that patients with an ACL-deficient knee do not show a similar reduction in the net quadriceps moment during jogging compared with walking. Similarly, while ascending stairs, the maximum net quadriceps moment occurs at approximately 60° of flexion and thus the amount of reduction in the net quadriceps moment is small compared with that during level walking. The adaptations during activities of daily living appear to be dependent upon the angle of knee flexion when the greatest net quadriceps moment occurs. These observations suggest an interaction between the direction of pull of the patella ligament and the functional role of the ACL (Fig. 6-5). When the knee is near full extension, the patellar ligament places an anterior pull on the tibia. As the knee flexes beyond approximately 45°, the orientation of the patellar ligament reverses direction during the quadriceps contraction and places a posterior pull on the tibia. At deeper flexion angles, the contraction of the quadriceps acts to compensate for an absent ACL.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree