Fig. 6.1
(a) AP radiograph demonstrating dysplastic left hip fully contained within true acetabulum. (b) AP radiograph demonstrating high dislocations of bilateral hips, as described by Hartofilakidis, in spite of prior corrective osteotomies
The natural history of dysplasia is variable and depends upon a number of factors including the severity of the anatomic abnormalities. Abnormal contract stresses across the joint are thought to lead to increased wear of the cartilage and the development of osteoarthritis [17]. Regardless of the grade of dysplasia, the mean age of onset of symptoms of hip pain has been reported to be in the fourth decade of life [18].
Evaluation
Not all patients with hip dysplasia are symptomatic, and in mild cases, the diagnosis may be made incidentally. However, in symptomatic individuals, groin pain, worsened with activity, is the most common presenting complaint. This pain may be caused by subluxation of the femoral head in the hip joint or be secondary to early degenerative changes of the cartilage. Mechanical symptoms such as catching or locking may signify labral pathology, or internal or external snapping hip [7]. Additionally, trochanteric bursitis, apophysitis, sacroiliac joint dysfunction, and iliotibial band tightness all must be included in the differential of hip and groin pain.
After a detailed history, including any previous treatment as an infant for a congenitally dislocated hip, or a family history of either congenital hip dysplasia or early onset of hip osteoarthritis, a physical examination is performed. Physical exam findings can help differentiate hip pain from other extra-articular causes of groin pain, such as athletic pubalgia, adductor strains, and inguinal or femoral hernias. The hip is taken through a full range of motion consisting of flexion and extension, abduction and adduction, and internal and external rotation. Any limitations of range of motion, or pain with the range of motion, are documented. Palpation is performed over all of the major bony prominences, musculature, and tendinous insertions [2]. The Patrick or FABER (flexion, abduction, and external rotation) test helps delineate hip pathology from sacroiliac joint pathology [9]. Ober’s test is used to assess the iliotibial band, trochanteric bursa, and tensor fascia lata. The Thomas test can be employed to identify hip flexion contracture or iliopsoas related pain [3]. Resisted hip flexion, or the Stinchfield test, is the most specific test for intra-articular hip pathology [4–6]. Positive straight leg raise, with pain radiating to the distal leg and foot, often signifies sciatic nerve irritation and lumbar spine pathology. While there is no specific test to diagnose hip dysplasia on physical exam, pain is typically reproduced with hyperextension and external rotation of the hip [1].
Gross physical examination of leg length and gait completes the physical examination. Alterations in gait may signify muscle imbalance or weakness (e.g., Trendelenburg gait) [8]. Gross leg length discrepancy may signify severe dysplasia or even frank dislocation of the hip. Examination of the spine is necessary to evaluate for scoliosis as well as assess pelvic obliquity. Finally, examination of the knee is necessary to identify referred pain to the hip secondary to knee pathology.
Imaging
Once hip pathology is suspected, appropriate imaging is necessary to confirm the diagnosis. Hip dysplasia is diagnosed by characteristic findings on plain radiographs as determined by the relationship of the femoral head to the acetabulum based on anatomic landmarks. Specific views of the pelvis and hips are ordered if hip pathology is suspected. Each view can provide different information with regards to gross anatomic position of the hip, sphericity of the femoral head, anterior and lateral coverage of the femoral head by the acetabulum, center of hip rotation, and morphology of the proximal femur and acetabulum. Anterior–posterior (AP) pelvic view and frog-leg lateral of the involved hip are the most commonly ordered exams. In addition, a false profile and 45° or 95° Dunn view are added to provide additional information on acetabular and proximal femoral anatomy [10]. The AP and false profile views provide information regarding acetabular anatomy. The lateral and Dunn views evaluate proximal femoral anatomy. MRI may be useful in assessing the integrity of the cartilage and labrum, particularly in the presence of mechanical symptoms.
When radiographs have been obtained, a careful assessment is made evaluating the acetabulum and the proximal femur. On the AP radiograph, acetabular depth, acetabular inclination, lateral center-edge angle, and hip center can be measured. Acetabular depth can be assessed by evaluating the floor of the acetabulum and the femoral head to the ilioischial line. Coxa profunda occurs if the floor of the acetabulum touches the ilioischial line, while protrusio acetabuli is present if the femoral head is medial to the ilioischial line (Fig. 6.2) [10].
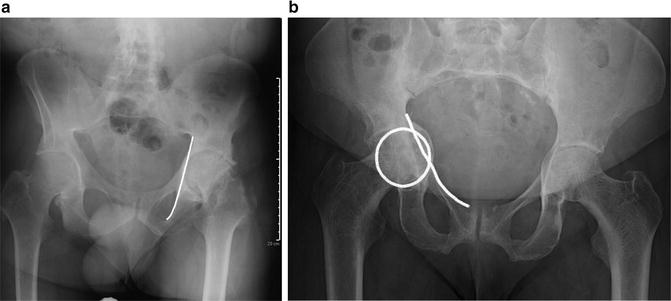
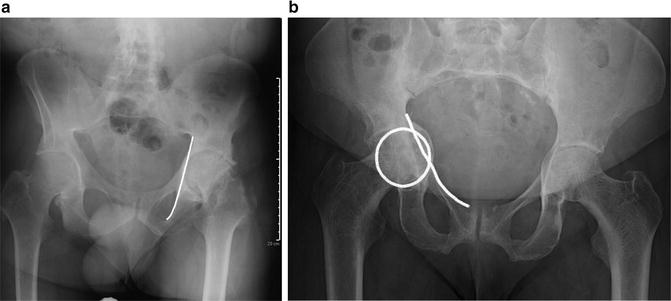
Fig. 6.2
(a) AP radiograph of the pelvis depicting Coxa profunda. The medial border of the acetabulum extends medially beyond the ilio-ischial (Kohler’s) line, while the medial border of the femoral head remains lateral to Kohler’s line. (b). AP radiograph of the pelvis demonstrating protrusio of the right acetabulum. Note the medial border of the femoral head (highlighted circle) extends medially beyond Kohler’s line (line)
Acetabular inclination is a measure of the orientation of the acetabulum in the coronal plane. This is measured by creating an angle from the lateral and inferior aspects of the sourcil (sclerotic weight-bearing portion of acetabulum) and a line parallel to a line created by connecting the teardrops. This Tonnis angle (normal 0–10°) is an indicator of the weight-bearing portion of the acetabulum (Fig. 6.3). A Tonnis angle greater than 10° indicates increased acetabular inclination, which leads to more concentrated stresses in a smaller area of the femoral head [10,13]. The lateral center-edge angle on the AP represents lateral coverage of the femoral head by the acetabular rim [3]. This is measured by drawing a line perpendicular to the transverse axis of the pelvis through the center of the femoral head, and creating an angle with a point at the lateral edge of the sourcil (Fig. 6.4). A normal center-edge angle is between 25° and 40° [22]. Less than 20° may indicate incomplete coverage of the femoral head and is generally considered to be diagnostic for acetabular dysplasia. Finally, the hip center can be determined by measuring the distance of the medial aspect of the femoral head to the ilioischial line (Fig. 6.5). A distance greater than 10 mm indicates a lateralized hip center of rotation [10]. Increased lateralization can increase joint reaction forces, leading to degenerative changes.
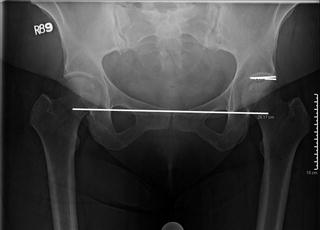
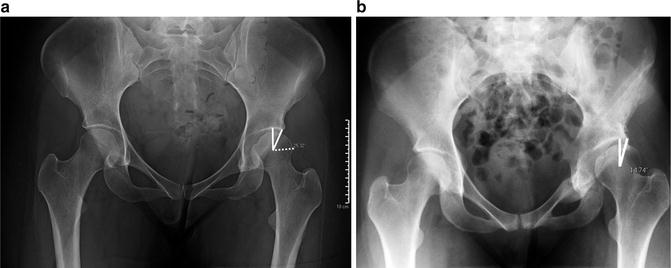
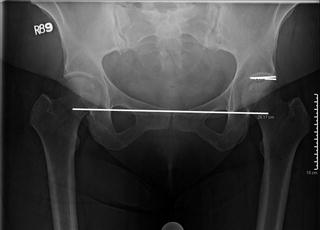
Fig. 6.3
AP radiograph demonstrating the Tonnis angle on the left hip. Tonnis angle formed between a line connecting the inferior and lateral edge of the sourcil to a line parallel to the inter-teardrop line
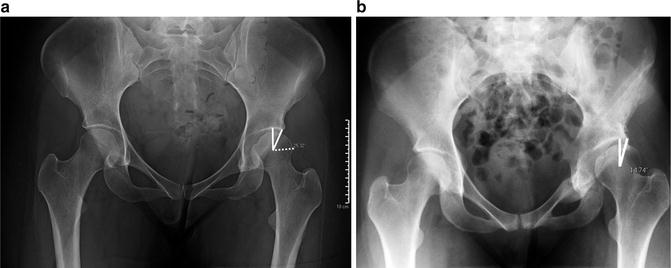
Fig. 6.4
(a) AP pelvis radiograph demonstrating lateral center-edge angle of Wiberg. This is the angle created from a vertical line from the center of the femoral head and a line from the center of the femoral head to the lateral edge of the sourcil. (b) Dysplastic hip with center-edge angle <15°, demonstrating increased uncoverage laterally of the femoral head by the acetabulum









