Hip Arthroscopy: The Lateral Position
Victor M. Ilizaliturri Jr
Alberto N. Evia-Ramirez
After adequate patient selection, patient positioning is the first and most important step in hip arthroscopy. Modern hip arthroscopy requires a dynamic technique of patient positioning. Traction is used to access the central compartment of the hip, which is the articular portion of the joint (1, 2). Structures in the central compartment are the acetabular articular surface, the acetabular labrum, the acetabular fossa and its contents, and most of the femoral head. The hip periphery (3), which is the intracapsular nonarticular portion of the hip joint, is usually accessed without traction. The hip periphery is considered to begin lateral to the free margin of the labrum. The structures inside the hip periphery are a small portion of the femoral head, the femoral neck, and the hip capsule with its synovial folds and zona orbicularis. Furthermore, hip mobility is frequently evaluated dynamically to assess clearance or improve access to different parts of the hip periphery. Therefore, effective patient positioning implies effective traction to separate the femoral head from the acetabulum and versatility to provide range of motion to the hip joint without traction to perform an adequate evaluation of the hip periphery.
TECHNIQUE FOR LATERAL PATIENT POSITIONING
The lateral positioning technique for hip arthroscopy was developed by Glick and Sampson (4) in San Francisco. It was first used successfully in a case where the patient presented morbid obesity and the developers failed to gain arthroscopic access into the hip using the supine approach. They decided to try the technique with the patient in lateral decubitus, expecting to produce the fatty tissue to “fall away” from the trochanteric region, thus providing access through the less soft tissue between the portal sites and the inside of the joint. The lateral position was also adopted and further developed by McCarthy et al. (6) in Boston.
The operating room setup for the lateral position is different from the setup for the supine position. When the patient is supine, both the surgeon and the assistant are on the operative side of the patient and monitors are on the opposite side. When the lateral position is used, the surgeon stands in front of the patient because most of the pathology inside the hip is in the front. The surgical assistant stands at the back side of the patient and in front of the surgeon. It is more comfortable to have access to an endoscopy suite that has monitors in every side of the room. If there is access to an arthroscopy cart with only a single monitor, we position it on the back side of the patient and proximal to the patient’s head; this will give a very adequate view both to the surgeon standing in the front side and to the assistant standing at the back side of the patient. The monitors of the image intensifier are positioned at the back side of the patient distal to the patient’s feet; these will provide a very adequate view to the surgeon and to the surgical assistant (Fig. 47.1).
When the lateral position is used, only the operative side foot is fixed to the traction device; pelvic tilt from the application of traction is avoided by the patient’s body weight and the length of the nonoperative leg resting free on the operative table.
In the supine position, pelvic tilt is avoided by fixing both feet to traction devices. Countertraction is applied on the foot in the nonoperative side.
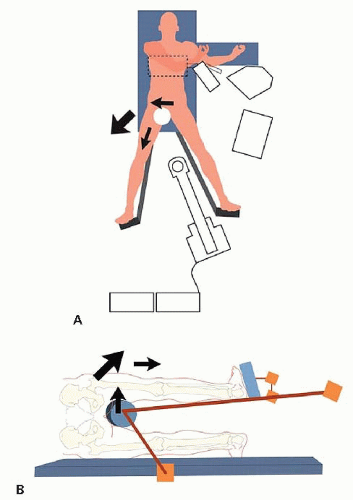
Both the lateral and the supine positions use a perineal post to fix the pelvis and upper body in position on the surgical table while traction is applied. The position of the perineal post in both cases is lateralized relative to the patient’s body, with the perineal post resting on the medial upper thigh. This protects the pudendal nerve from direct compression and lateralizes the vector of force from traction, aligning it closer to the direction of the femoral neck than to the direction of the femoral shaft (Fig. 47.2A and B). For both the lateral and the supine techniques, an oversized perineal post of at least 10-cm diameter is used (4). The position of the patient’s genitalia should be verified before traction is established to protect them from compression injury.
When using the lateral position, lateralization of the perineal post is obtained by raising the position of the post relative to the operating table, and the surgeon should be careful not to over-raise the post, producing a “hanging patient” situation.
The arch of the image intensifier is positioned horizontally to obtain an antero posterior view of the affected side hip. Our preference is to position the arch under the surgical table (Fig. 47.3). In some patients the size of the arch may not be large enough to reach the operative side hip from under the table (because the patient is in lateral decubitus, the operative hip is on the upper side of the patient opposite to the operating table). If this is the case, the arch can be brought into the operating field in an over-the-top position and tilted in the direction of the patient’s head to prevent it from obstructing the surgical team.
Foot fixation is a very important step in patient positioning. As mentioned above, when the lateral position is used, only the operative side foot is fixed to the traction device. Fracture tables and dedicated hip distractors have a foot platform, which is connected to the traction device. The way the foot is fixed to the platform varies and depends on the design of the table or distractor and surgeons’ preference. The objective is to provide adequate and stable foot fixation to the traction device so that the traction force is effectively applied to the foot and transmitted through the lower extremity onto the hip joint, producing effective separation of the femoral head from the acetabulum. Separation occurs at the hip because the pelvis is stabilized with the perineal post. Adequate padding of the foot should always be performed to prevent compression injury. There are different methods of foot fixation to the traction platform:
Elastic bandage and taping. We have found this method to be effective and inexpensive. A cotton wrap is used around the foot for padding, the foot is fixed to the traction platform using an AC-bandage, and finally it is stabilized using adhesive tape to prevent foot separation from the platform. The result is like a boxer’s bandage.
Traction booties. Most of the fracture tables provide traction booties as fixation devices to the platform. Belt buckles or Velcro straps are available for fixation of the booties over the feet. In our experience, Velcro straps seem to be more stable. It is also important to provide adequate padding to the foot inside the bootie. Fixation may be complemented with an elastic bandage around the bootie.
Ski boots. McCarthy introduced the concept of a ski bootlike design for the Inomed lateral distractor (Savannah, GA). This is the most effective fixation device. It provides a stable fixation between the foot and the boot and between the boot and the traction platform. Care must be taken to ensure adequate padding of the foot within the ski boot. It is the most expensive of the foot fixation systems and may not be available for every traction table or distractor.
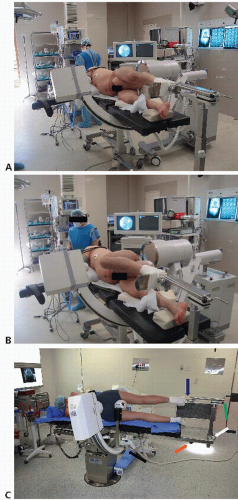
FRACTURE TABLES
Fracture tables are the option of choice when hip arthroscopy is performed in the supine approach, because the positioning technique is very similar to the position used for fracture fixation. Fracture tables may also be used with the lateral position but special accessories are necessary, and they may not be available at every hospital (Fig. 47.4A-C). Because most of the cases of hip arthroscopy today require dynamic hip positioning, the surgeon and the operating room team should be very familiar with the design of the fracture table to operate it adequately to provide traction, traction release, and hip range of motion during the case. It is very important that the unscrubbed surgical team understand the operation of the fracture table because the surgeon will be in the sterile field and the table will be operated at the request of the surgeon by unsterile operating room staff.
DEDICATED HIP ARTHROSCOPY DISTRACTORS
Dedicated hip arthroscopy distractors were originally designed for the lateral approach because many of the fracture
table designs had no accessories for the lateral position. The main advantage of dedicated distractors is that they can be used in combination with a standard surgical table. The first generation of hip distractors was designed to provide only traction to obtain separation of the femoral head from the acetabulum and perform surgery of the central compartment. In these early designs, dynamic examination of the hip periphery was not considered.
table designs had no accessories for the lateral position. The main advantage of dedicated distractors is that they can be used in combination with a standard surgical table. The first generation of hip distractors was designed to provide only traction to obtain separation of the femoral head from the acetabulum and perform surgery of the central compartment. In these early designs, dynamic examination of the hip periphery was not considered.
More recent distractors have been designed for providing traction and range of motion without traction for arthroscopic access of both the central and the peripheral compartments. Ease of operation is also a design feature of modern hip distractors to facilitate their operation by unsterile operating room personnel under the sterile drapes (Fig. 47.5A and B).
Dedicated supine distractors for hip arthroscopy are also available today. They are a good option for surgical centers where fracture tables are not available and have a very competitive cost compared with the cost of a fracture table system.
OTHER POSITIONING SYSTEMS
Positioning system technology such as the Spider (Tenet Medical, Calgary, Canada) has been a very popular option in shoulder and ankle surgeries. The system consists of a multiple joint “arm” that uses pneumatic pressure. When the system is pressurized, the joints are stable, and the arm holds a position. When pressure is released, the joints are loose, and range of motion can be reproduced. To apply the spider in hip arthroscopy, a perineal post and the Spider are attached to the surgical table; a traction device and a fixation boot are attached to the end of the Spider; the system is used to bring the lower extremity to a pretraction position; and the system is stabilized and traction is applied with the traction device (Fig. 47.6). When the traction time is completed, the system pressure is released, allowing range of motion to be applied to the hip joint. The system can be pressurized again at any position of the hip the surgeon decides. The system is the most versatile for range of motion and gives full control of pressure release to the surgeon, making it very easy to operate. The disadvantages of the system are that it may be insufficient for very heavy or muscular patients and that a lateral rail extension is necessary to mount the Spider distally.
TRACTION POSITION AND TRACTION TEST
The position of the hip for traction has been a matter of debate among different authors. Our preference is to position the patient with neutral hip rotations. Internal rotation may place the sciatic nerve closer to the posterior margin of the greater trochanter, increasing the risk of puncture while introducing a needle through the posterolateral portal (at the posterior superior corner of the greater trochanter). The hip is positioned in slight flexion, of 15° to 20° to relax the anterior hip capsule. More flexion may increase tension on the sciatic nerve (7). Slight adduction of about 3° to 5° is applied to take mechanical advantage of the perineal post, using it to slightly lever the hip laterally with the proximal femur.
Once the patient is in position with the anesthetic procedure installed and the arch of the image intensifier has been placed optimally to provide an antero posterior view of the operative hip, a traction test is performed before draping. Separation of at least 10 mm from the acetabular rim and the superior femoral head should be documented with the image intensifier (6). With the traction test applied, the surgeon must do a final examination of contact areas from the perineal post, make sure the patient’s genitalia are free of compression, verify there are no compression points or lift off of the foot from the traction plate, and confirm padding is adequate. If the traction test was successful, traction is released and the patient is prepared and draped. In the case of an unsuccessful traction test, the surgeon should verify every step of patient positioning and look for the problem.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree