Hip Arthroscopy for Nonstructural Hip Problems
J.W. Thomas Byrd
Key Points
• Numerous nonstructural hip disorders may be amenable to arthroscopic intervention.
• Routine hip arthroscopy should include both central and peripheral compartments.
• Snapping hip syndromes, including iliopsoas tendon and iliotibial band, can be addressed.
Introduction
Femoroacetabular impingement (FAI) and dysplasia are the two most common structural problems implicated in hip pathology. However, numerous nonstructural problems are associated with disorders of the hip joint and hip region. These include macrotrauma, repetitive overuse microtrauma, consequences of kinetic and kinematic disorders, and intrinsic tissue disease. Hip problems manifested by painful symptoms are often the culmination of multifactorial causes. Underlying disease may render some joints more susceptible to acute injury. For example, acute subluxations and dislocations encountered among contact sports, which are relatively low-velocity injuries compared with those resulting from vehicular trauma, often have underlying findings of impingement.1 It is likely that owing to the underlying morphology, the hip is rendered more susceptible to luxation by the levering effect.
Numerous soft tissue disorders around the hip can cause problems and may be amenable to endoscopic intervention. The collective group of coxa saltans, which includes snapping of the iliopsoas tendon and iliotibial band and possibly other less evident entities, can be corrected endoscopically.2–4 Bursectomy can be performed, and many cases of recalcitrant trochanteric bursitis may actually represent painful abductor tendinopathies.5–7 Keep in mind that some of these disorders may be incidental, normally occurring observations, and others can occur as a normal consequence of aging or of subtle gait abnormalities. It is a challenge to the clinician to distinguish pathologic processes from normal variations. It is also important to keep in mind that several disorders may coexist, and one must differentiate which are the principal problems and how they should best be managed. Recommendations may range from simple activity modifications, to structured conservative treatment, to surgical intervention.
Indications/Contraindications
For nonstructural problems, the most common indication for arthroscopy is pain caused by some type of pathologic condition that can be corrected by arthroscopic techniques. Rarely is arthroscopy considered in the presence of a painless disorder. Often, patients may present for assessment with modest symptoms that are not sufficient to create a functional problem. Under these circumstances, thoughtful observation and other nonoperative treatments may be appropriate. If symptoms are worsening in the presence of recognized pathology, it may be prudent to be proactive in considering surgical intervention. Keep in mind that various disorders may coexist, which can include pathologic conditions and anomalies that are not responsible for the patient’s symptoms. For example, hip joint pathology may occur in conjunction with a snapping iliopsoas tendon, which may or may not be a contributing cause of pain warranting correction.
Contraindications to hip arthroscopy are few. Most important is simply ensuring that the patient’s condition is amenable to and appropriate for arthroscopic intervention. Another important consideration is ensuring that the patient’s expectations can be practically met by the procedure. Surgery in the presence of unreasonable expectations will be a failure regardless of the skill with which the procedure is performed. Advanced disease states such as severe degenerative arthritis are contraindications simply because arthroscopy cannot reasonably be of any benefit. Some severe deformities, wound problems, and medical conditions may contraindicate arthroscopy or possibly even any type of surgery.
Preoperative Planning
Imaging studies are an important part of the diagnostic workup and surgical planning. Radiographs reveal joint morphology and underlying structural disorders, as well as the presence of degenerative disease. It is important to keep in mind that damage within the joint is typically substantial before radiographic changes become evident. Thus reasonable joint space preservation may not preclude the existence of considerable degenerative disease. Also, subtle radiographic changes should be taken as serious evidence of advanced pathology.
Conventional magnetic resonance imaging (MRI) is an important component of most preoperative planning for hip surgery. Its reliability for detecting intra-articular pathology may be variable, but it is often helpful to rule out disorders that will not benefit from arthroscopy, such as avascular necrosis, transient regional osteoporosis, and many others. Gadolinium arthrography with MRI (MRA) is better but is not completely reliable for detecting all intra-articular pathology. Injecting anesthetic along with contrast is a valuable tool in substantiating that the hip joint is the source of symptoms. In cases of multiple pain generators, intra-articular injection helps to distinguish how much the hip is contributing.8 Assessing the patient’s response to the injection can be important in making the decision for surgery. In general, imaging studies are good for assessing labral pathology but may be less reliable in detecting associated articular damage. This is important when one is counseling patients because the uncertain extent of articular damage is often a limiting factor in the success of arthroscopy. Computed tomography has a significant role in assessing bony architecture and the three-dimensional morphology of the joint but is less often enlightening for soft tissue problems about the hip.
Problematic snapping of the iliopsoas tendon and the iliotibial band is mostly identified from the history and examination findings. This snapping is usually a dynamic phenomenon, not predictably reproduced with examination under anesthesia, and the arthroscopic findings do little to substantiate the diagnosis. Abductor tendinopathies can be a normal consequence of aging but can also be a source of relevant clinical pathology. Thus the clinical findings dictate how aggressive one should be with lesions encountered in the peritrochanteric space.
Description of Technique
The technique illustrated is being performed with the patient in supine position.9,10 The important principles for performing safe, effective, reproducible arthroscopy are the same whether the patient is in the lateral decubitus or supine orientation. Portal placements, relationships of extra-articular structures, and arthroscopic anatomy are all the same regardless of positioning.
Equipment
A standard fracture table or custom distraction device is needed to achieve effective joint space separation. The C-arm is important for precise placement of instrumentation within the joint. Extra-length arthroscopy instruments are also available to accommodate the dense surrounding soft tissue.
Anesthesia
The procedure is commonly performed with the patient under general anesthesia. It can be performed under epidural but requires an adequate motor block to ensure optimal distractibility of the joint.
Intra-Articular (Central) Compartment
Setup
The perineal post is heavily padded and lateralized against the medial thigh of the operative hip (Fig. 53-1). This aids in achieving the optimal traction vector (Fig. 53-2) and reduces pressure directly on the perineum, lessening the risk of neuropraxia of the pudendal nerve. Neutral rotation achieves a constant relationship between the topographic landmarks and the joint. Slight flexion may relax the capsule, but excessive flexion should be avoided because this places undue tension on the sciatic nerve and may block access to the anterior portal. Typically, about 50 pounds of force is needed to distract the joint. In general, the goal is to use the minimum force necessary to achieve adequate distraction while keeping traction time as brief as possible. Two hours is usually recognized as a reasonable limit for traction.

Figure 53-1 The patient is positioned on the fracture table so that the perineal post is placed as far laterally as possible toward the operative hip resting against the medial thigh. (Courtesy J. W. Thomas Byrd, MD, Nashville, Tenn.)
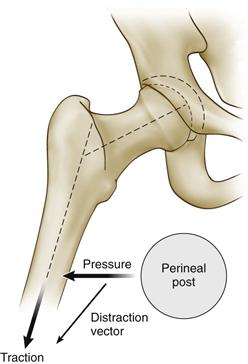
Figure 53-2 The optimal vector for distraction is oblique relative to the axis of the body and more closely coincides with the axis of the femoral neck than the femoral shaft. This oblique vector is partially created by abduction of the hip and is partially accentuated by a small transverse component to the vector created by lateralizing the perineal post. (Courtesy J. W. Thomas Byrd, MD, Nashville, Tenn.)
Portals
Three standard portals provide optimal access for the central compartment (Figs. 53-3 and 53-4). Two of these (anterolateral and posterolateral) are placed laterally over the superior margin of the greater trochanter at its anterior and posterior borders. The anterior portal is placed at the site of intersection of a sagittal line drawn distally from the anterior superior iliac spine and a transverse line across the tip of the greater trochanter. With careful orientation to the landmarks in relation to the joint, these portals are a safe distance from the surrounding major neurovascular structures.11 Additional portals may be needed occasionally Most common is a more distal mid-anterior portal for placing anchors in conjunction with labral repair. The more distal position is necessary to ensure that the anchor diverges at the rim to avoid perforating the acetabular surface.
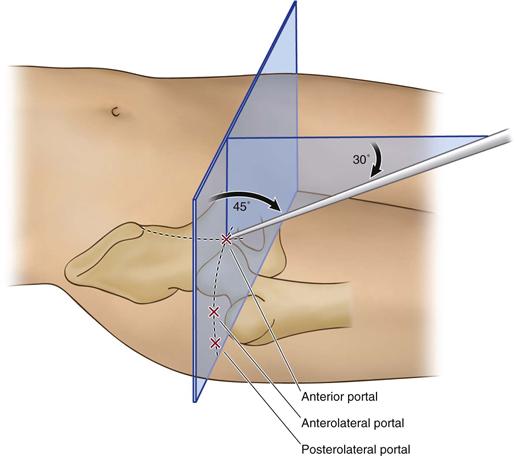
Figure 53-3 The site of the anterior portal coincides with the intersection of a sagittal line drawn distally from the anterior superior iliac spine and a transverse line across the superior margin of the greater trochanter. The direction of this portal courses approximately 45 degrees cephalad and 30 degrees toward the midline. The anterolateral and posterolateral portals are positioned directly over the superior aspect of the trochanter at its anterior and posterior borders. (Redrawn from Byrd JWT: Hip arthroscopy utilizing the supine position. Arthroscopy 10:275–280, 1994.)
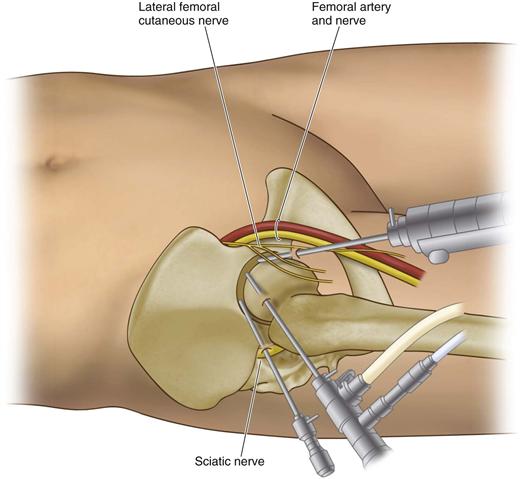
Figure 53-4 The relationship of major neurovascular structures to the three standard portals is demonstrated. The femoral artery and nerve lie well medial to the anterior portal. The sciatic nerve lies posterior to the posterolateral portal. Small branches of the lateral femoral cutaneous nerve lie close to the anterior portal. Injury to these is avoided by utilizing proper technique in portal placement. The anterolateral portal is established first because it lies most centrally in the safe zone for arthroscopy. (Courtesy J. W. Thomas Byrd, MD, Nashville, Tenn.)
Diagnostic Procedure
After traction is applied, a spinal needle is placed from the anterolateral position and the joint is distended with fluid. The anterolateral portal is then established under fluoroscopic control for introduction of the arthroscope (Fig. 53-5). Careful attention is necessary to avoid perforating the labrum or scuffing the articular surface.12 Using the 70 degree scope, the anterior and posterolateral portals are placed under direct arthroscopic view as well as under fluoroscopy for precise entry into the joint. Diagnostic and operative arthroscopy is then achieved by interchanging the arthroscope with instruments between the three established portals. Use of both 70 degree and 30 degree scopes provides optimal viewing despite limitations of maneuverability within the joint (Figs. 53-6 through 53-9). If needed, supplemental portals can be placed under similar arthroscopic control.
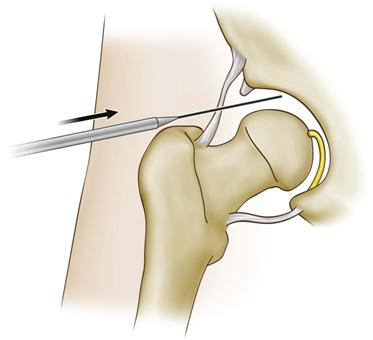
Figure 53-5 The arthroscope cannula is passed over a guide wire that was inserted through a prepositioned spinal needle. Fluoroscopy aids in avoiding contact with the femoral head or perforating the acetabular labrum.
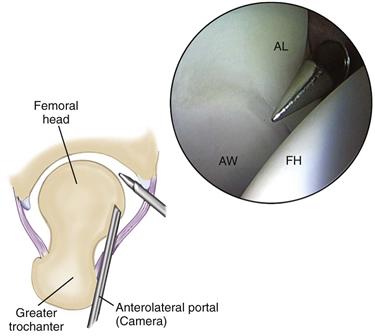
Figure 53-6 Arthroscopic view of a right hip from the anterolateral portal demonstrates the anterior acetabular wall (AW), the anterior labrum (AL), and the femoral head (FH). The anterior cannula is seen entering underneath the labrum. (Courtesy Smith & Nephew Endoscopy, Andover, Mass [artwork].)
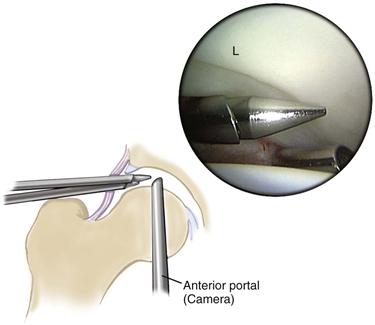
Figure 53-7 Arthroscopic view from the anterior portal demonstrates the lateral aspect of the labrum (L) and its relationship to the lateral two portals. (Courtesy Smith & Nephew Endoscopy, Andover, Mass [artwork].)
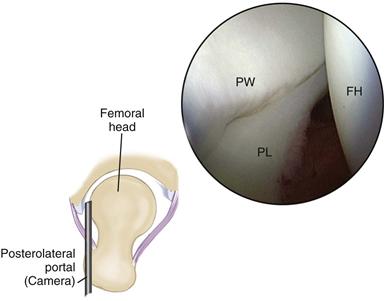
Figure 53-8 Arthroscopic view from the posterolateral portal demonstrates the posterior acetabular wall (PW), the posterior labrum (PL), and the femoral head (FH). (Courtesy Smith & Nephew Endoscopy, Andover, Mass [artwork].)
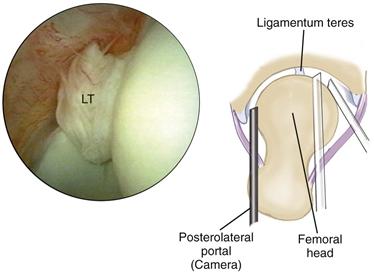
Figure 53-9 The acetabular fossa can be inspected from all three portals to view the ligamentum teres (LT) with its accompanying vessels traversing in a serpentine fashion from its more posteriorly placed acetabular attachment. (Courtesy Smith & Nephew Endoscopy, Andover, Mass [artwork]. Reprinted with permission. Byrd JWT: The supine position. In Byrd JWT, editor: Operative hip arthroscopy, New York, 1998, Thieme Medical Publishers [arthroscopic image].)
Peripheral Compartment
Positioning
Routine arthroscopy of the peripheral compartment is performed after arthroscopy of the intra-articular compartment has been completed. The instruments are removed, the traction released, and the hip flexed approximately 45 degrees (Fig. 53-10). This relaxes the capsule, providing access to the peripheral compartment. Note that when correction of impingement is performed, a capsulotomy is needed for exposure and facilitates movement between the central and peripheral compartments without the need to remove the instruments. This technique is described in Chapter 54.
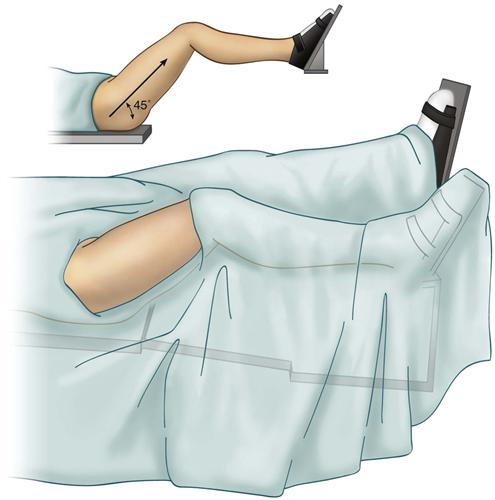
Figure 53-10 The operative area remains covered in sterile drapes while traction is released and the hip is flexed 45 degrees. Inset, Illustrates the position of the hip without the overlying drape.
Portal Placement
At least two portals are used routinely to access the peripheral compartment. These include the anterolateral portal and an ancillary portal established 4 to 5 cm distally. A broad safe zone in which to work is present, and numerous variations on portal placement are available. It is simply important to be consistent in portal choices for reproducibility of placement and for orientation to the anatomy of the periphery.
Diagnostic Procedure
The anterolateral portal is redirected onto the anterior neck of the femur (Fig. 53-11). The ancillary portal is then established distally under direct arthroscopic and fluoroscopic guidance (Fig. 53-12). The arthroscope and instruments are interchanged for inspection (Figs. 53-13 and 53-14). The 30 degree scope is usually sufficient for most work done in the periphery.
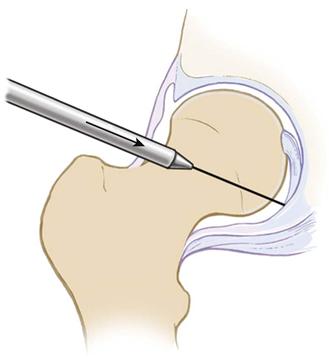
Figure 53-11 From the anterolateral entry site, the arthroscope cannula is redirected over the guide wire through the anterior capsule onto the neck of the femur. (Courtesy Smith & Nephew Endoscopy, Andover, Mass.)
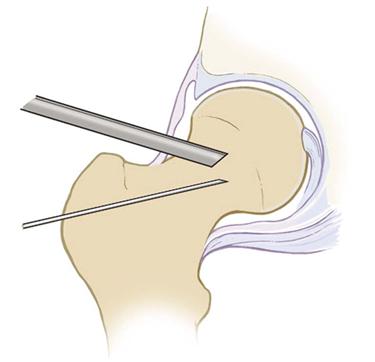
Figure 53-12 With the arthroscope in place, prepositioning is performed with a spinal needle for placement of an ancillary portal distally. (Courtesy Smith & Nephew Endoscopy, Andover, Mass.)
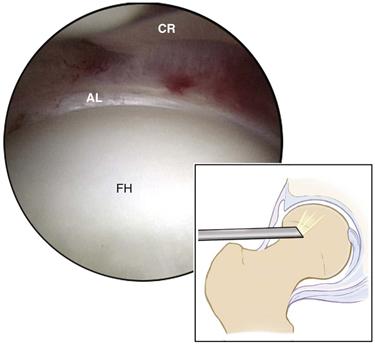
Figure 53-13 Peripheral compartment viewed superiorly demonstrates the anterior portion of the joint, including the articular surface of the femoral head (FH), the anterior labrum (AL), and the capsular reflection (CR). (Courtesy Smith & Nephew Endoscopy, Andover, Mass [artwork].)
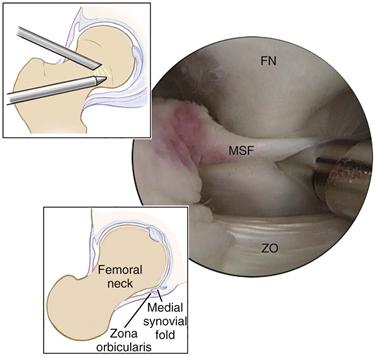
Figure 53-14 Peripheral compartment viewed medially demonstrates the femoral neck (FN), the medial synovial fold (MSF), and the zona orbicularis (ZO). (Courtesy Smith & Nephew Endoscopy, Andover, Mass [artwork].)
Iliopsoas Bursoscopy
Positioning
Flexion is slightly less (15 to 20 degrees) than that used to view the peripheral compartment. The hip is externally rotated; this moves the lesser trochanter to a position that is more anterior and accessible to the portals.
Portals
Two portals are needed for viewing and using instrumentation within the bursa (Fig. 53-15). These portals are distal to those used for the peripheral compartment and require fluoroscopy for precise positioning. They may be slightly more anterior for complete access to the area of the lesser trochanter.
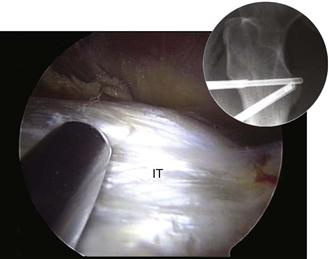
Figure 53-15 The arthroscope and the shaver are positioned within the iliopsoas bursa directly over the lesser trochanter, allowing identification of the fibers of the iliopsoas tendon (IT) at its insertion site.
Diagnostic Procedure
The spinal needle is placed directly on the lesser trochanter under fluoroscopy. With the arthroscope introduced, a second portal is established. Adhesions or fibrinous debris within the bursa may have to be débrided to achieve clear visualization (see Fig. 53-15). Staying next to bone avoids straying into the medial soft tissues.
Trochanteric Bursoscopy (Peritrochanteric Space)
Positioning
Positioning is the same as for arthroscopy of the central compartment, but no traction is needed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







