Hip Arthrodesis
Nemandra A. Sandiford
Clive Duncan
INTRODUCTION
The average age of patients presenting with symptomatic coxarthrosis is decreasing (1). Excellent medium- to long-term results can be predictably achieved in such patients with total hip arthroplasty (THA). The results of THA in young, active patients (less than 50 years old) are less predictable. Failure rates in this group have been reported as higher (2,3), and risks particular to arthroplasty such as dislocation, osteolysis, and soft tissue reactions to wear particles (adverse reaction to metal debris) are genuine concerns. These results are expected to improve with newer techniques and technology.
The surgeon thus needs to consider all available options in this patient population, which would allow return to an active, productive, and independent lifestyle while delaying their need for a THA. Nonsurgical treatment in this group often fails to address the cause of their symptoms and can sentence them to an increasingly dependent and sedentary lifestyle with resultant health and socioeconomic consequences.
When too late for joint-preserving intervention, such as arthroscopy or osteoplasty, the remaining surgical options in this group include arthrodesis, realignment pelvic or femoral osteotomies, and arthroplasty. Arthrodesis has a definite place in the management of this challenging group especially in the teenage or young adult years (4). It predictably relieves pain, allows return to daily function including manual work, and can be converted to THA at a later date (5,6). Arthrodesis has been shown to significantly improve quality of life and provide high levels of patient satisfaction (7).
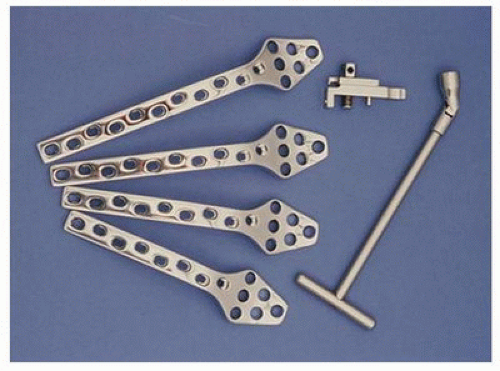
One of the more popular techniques used for hip arthrodesis is that proposed by Duncan et al. (the Vancouver technique) (8). This is in the focus of this chapter. It is associated with a high rate of fusion and usually requires no supplementary immobilization such as a hip spica. The Vancouver technique utilizes a laterally placed “cobra” plate (Fig. 10-1), which facilitates excellent exposure, initial rigid fixation, and reattachment of the greater trochanter over the plate with the attached abductors at their normal length and tension. The trochanter can be mobilized easily at a later date during fusion conversion to a replacement arthroplasty.
INDICATIONS FOR HIP ARTHRODESIS
The ideal candidate is a teenage or young adult male patient involved, or likely to be, in heavy manual labor.
CONTRAINDICATIONS
Contraindications to arthrodesis include the following:
Active infection
Lower back pain or evidence of an abnormality that may become painful (e.g., spondylolisthesis)
Ipsilateral knee instability or osteoarthritis
Contralateral hip osteoarthritis
Significant bone loss (absent head and neck) or poor quality such that rigid fixation would be challenging
PREOPERATIVE ASSESSMENT AND SURGICAL PLANNING
Appropriate patient selection is vital. The most common causes for conversion of arthrodesis to THA include progressive pain in the lumbar spine, ipsilateral knee, and contralateral hip (9). As a result, concurrent degenerative disease in these areas needs to be excluded with a thorough history examination and radiographic evaluation. It is important to accurately measure and document leg lengths and to explain that modest shortening of the limb is to be expected after operation. This is in fact desirable because it facilitates swing through of the foot while walking.
RADIOGRAPHIC EVALUATION
Leg lengths, bone quality, and bone stock of the proximal femur and acetabulum need to be carefully assessed in order to predict intraoperative technical challenges. Poor bone stock on either side of the hip can affect the quality of fixation and fusion rates. A dysmorphic femoral head (secondary to trauma, avascular necrosis, or childhood disease) can result in greater shortening of the limb. Any angular or rotational deformity of the proximal femur must be noted as this can affect the final position of the limb after arthrodesis. This influences the decision as to whether a simultaneous osteotomy is also required.