A Ossification of proximal femur This sequence shows ossification in the normal child.
Redrawn from Tönnis (1984).
Growth of the upper femur occurs not only in the capital epiphysis and trochanteric apophysis but also along the neck of the femur [C]. Growth from the triradiate cartilage is a major contributor to acetabular development [B]. The deformities caused by trauma are site-specific [C].


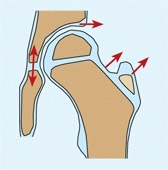
C Proximal femoral growth Note that growth (red arrows) occurs at many sites about the upper femur, including appositional growth of the femoral neck. Damage to the greater trochanteric apophysis from curettage for a bone cyst (yellow arrow) or from reaming to place an IM nail (orange arrow) causes a reduction in width and functional elongation of the femoral neck.
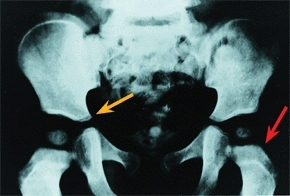
B Pelvic growth This child had a phosphorized oil dietary supplement as a child. Growth patterns are shown. Note the growth that occurs in the triradiate cartilage (orange arrow) and upper femur (red arrow). Courtesy I. Ponseti.
Most growth of the acetabulum occurs from the triradiate cartilage. Closure will cause severe progressive dysplasia. Additional growth of the acetabulum occurs from the acetabular epiphysis. This growth is especially important late in childhood and during adolescence.
Damage to these growth centers, either from trauma or as a complication of treatment, is a common source of deformity and disability. The upper femur is very susceptible to vascular or epiphyseal injury.
Vascularity
Disturbances in blood supply to the upper femur are a common cause of many serious deformities and subsequent disability.
The femoral head may receive blood through the ligamentum teres, epiphyseal vessels, or metaphysis. The femoral head in the infant is supplied by epiphyseal vessels and vessels that traverse the epiphyseal plate [A]. These transphyseal vessels disappear as ossification develops in the femoral head. Circulation in the child is primarily through the metaphyseal vessels. Only in late childhood and adolescence do the ligamentum teres vessels make a significant contribution. After closure of the capital physeal plate, the metaphyseal vessels contribute to the circulation.

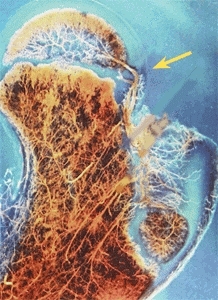
A Vascularity of the femoral head In infancy, transphyseal vessels are often present (red arrow). In childhood, the femoral head is supplied by the lateral retinacular vessels that must traverse the joint (yellow arrow). From Chung (1976).
During most of childhood, this vascular supply is provided by two anastomotic rings formed by the medial and lateral circumflex vessels [B]. The pattern of distribution is variable, and deficiencies may contribute to the development of avascular necrosis.
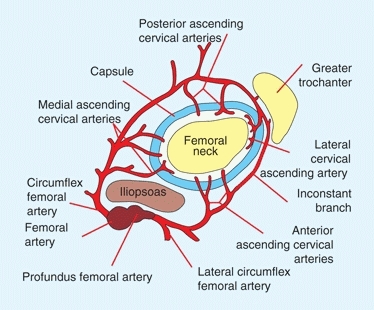
B Vascularity of the femoral head Note that the proximal femur is supplied by an arcade of vessels that arise from the profundus femoral artery.
Biomechanics
Loading within the joint is affected by the load-bearing area [C]. Increased loading is prominent when the hip is subluxated or shallow. Increased loading leads to osteoarthritis in adult life.
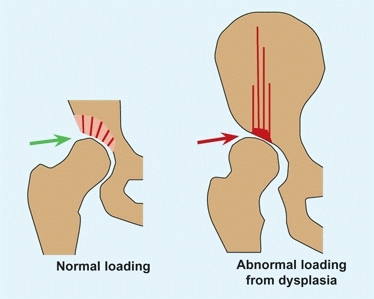
C Biomechanics of the hip In the normal hip, loading (green arrow) is low and well distributed. In dysplasia, loading is concentrated (red arrow), resulting in eventual cartilage degeneration.
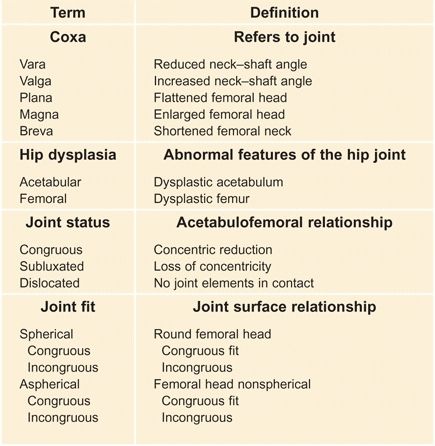
D Nomenclature for deformity These terms are commonly used to describe various patterns of hip deformity.
Operative procedures, especially osteotomies of the pelvis and femur, dramatically affect the biomechanics of the hip. The hip joint normally carries about four times its body weight. Hip joint loading is reduced by varus femoral osteotomy or by medializing the joint, as done in the Chiari osteotomy. When reconstructing a hip, try to achieve as normal an anatomy as possible.
Nomenclature
Hip terminology is reasonably straightforward [D, previous page]. The most significant recent change was the replacement of the term congenital with developmental in hip dysplasia. Congenital hip disease (CDH) thus becomes developmental hip dysplasia (DDH). Hip disorders caused by muscle disorders secondary to neurologic disorders such as cerebral palsy are called neurogenic dysplasia of the hip (NDH). The term dysplasia is a broad term covering disorders that may involve the acetabulum, upper femur, or both elements.
Evaluation
A thorough evaluation of the hip is important due to the vulnerability of the hip joint to damage, especially from impaired blood supply. Delays in diagnosis of DDH, septic arthritis, and slipped epiphysis are relatively common and sometimes result in joint destruction. The deep position of the hip joint makes evaluation more difficult than most extremity joints such as the knee or ankle. This, together with its tenuous vascularity, places the hip at special risk.
History
Is there a family history of hip problems? DDH is familial. Has the child complained of pain? Night pain suggests a neoplastic origin. Remember that hip pain may be referred to the knee [A]. Has the child limped? Were there systemic signs? Has the problem been getting worse or has it plateaued? Be certain to rule out septic arthritis and slipped epiphysis as acute disorders and DDH as a long-term problem.
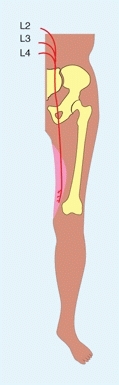
A Hip pain referred to knee The obturator nerve supplies articular branches to the hip and cutaneous coverage about the knee. Hip disorders may present with knee pain.
Physical Examination
Observation
Does the child appear ill? Is there spontaneous movement of the limb? Pseudoparalysis is common in trauma and infections. Does the child limp? Limping from hip problems is usually antalgic or due to an abductor lurch.
Palpation
Palpate for tenderness over the bony prominences. Tenderness is often found in the adolescent with bursitis, tendonitis, or overuse syndromes. By determining the point of maximum tenderness exactly, a presumptive diagnosis can often be made.
Range of Motion
Hip disorders often result in loss of motion. Inflammatory disorders usually cause a reduction in internal hip rotation early on and eventually flexion and adduction contracture of the hip.
Hip rotation
Assess with the child prone. Assessing the range of medial rotation is a valuable screening test [B]. The finding of asymmetric hip rotation is abnormal and indicates the need for a radiograph of the pelvis.
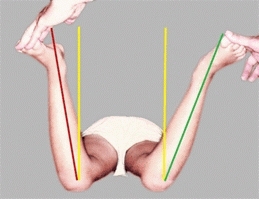
B Hip rotation test Position the child prone with the knees flexed to 90°. Rotate the hips internally and note any guarding and the extent of rotation. Asymmetry of rotation is usually abnormal. In this child with Legg-Calvé-Perthes disease on the left hip, rotation was limited compared to the normal right hip.
Flexion
Detect the presence of a contracture using the Thomas or prone extension test [C]. The prone extension test is most accurate, especially in children with neuromuscular disorders.
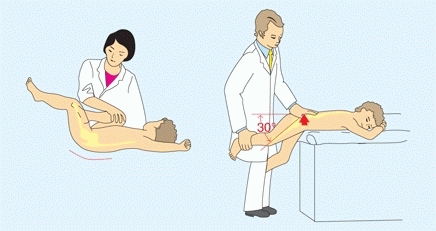
C Hip flexion contracture assessment The Thomas test (left) is performed with the contralateral hip flexed. Extend to measure the degree of contracture. The prone extension test (right) is performed with the child prone. Gradually extend the hip until the hand on the pelvis begins to rise. The horizontal–thigh angle indicates the degree of contracture.
Abduction–Adduction
Assess while stabilizing the pelvis with one hand.
Trendelenburg Test
Assess an abductor lurch using the Trendelenburg test [D]. Ask the child to lift one leg at a time. The pelvis should rise on the elevated side. A drop of that side is a positive sign and suggests that the abductor mechanism is weak on the opposite side. This lurch may be due to weakness of the muscles, a change in shape of the upper femur, or inflammation of the joint.

D Trendelenburg test This girl has DDH with weakness of the left hip abductors. When standing on her right leg, right hip abductors contract to elevate the left pelvis to maintain the head centered over the body (green lines). When standing on the weaker left leg, abductor weakness allows the right pelvis to fall (blue arrow). She must then shift her weight over the left leg (red lines).
Laboratory Studies
A CBC and an ESR and CRP are often helpful in evaluating hip disorders. The ESR and CRP are useful in differentiating septic arthritis from toxic synovitis. Infections usually elevate the ESR above 25–30 mm/hr. Toxic synovitis causes only a slight elevation in the ESR and CRP. Hematologic disorders such as leukemia and sickle cell disease may cause pelvic pain.
Hip Joint Aspiration
The aspiration of the hip is the most certain method of establishing the diagnosis of septic arthritis. Aspirate the joint promptly if the diagnosis of septic arthritis is seriously included in the differential. Although a negative aspirate (even when documented by an arthrogram) is not absolutely definitive, it is highly suggestive that the problem is not within the joint.
Delays in diagnosing septic arthritis may be catastrophic because it jeopardizes the vascularity to the femoral head and articular cartilage. Joint aspiration does not affect bone scans and should not be delayed by plans to perform imaging procedures.
Imaging
Imaging is required to evaluate hip disorders in children. Imaging is the only way to establish a prognosis. The vast majority of hip problems in children can still be managed adequately by careful examination and conventional radiographs.
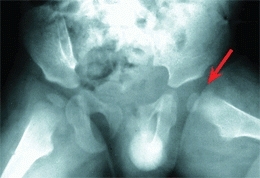
Conventional radiography
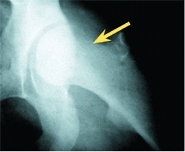
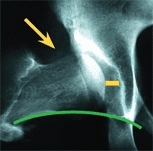
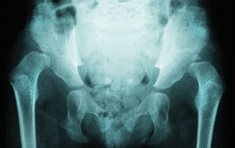
Evaluate most hip problems with conventional radiography. Except for the initial study, use a gonad shield. Obtain a single AP study [A]. Several useful measures may be made from this simple study [B, and A, next page]. Note any asymmetry in ossification of the pelvis. A painful condition such as an osteoid osteotomy results in hemideossification [C]. Be aware of the situations in which false negative studies are commonly misleading. A negative study does not rule out DDH in the neonate or an early septic arthritis. An AP radiograph may not show a mild slipped capital femoral epiphysis (SCFE).
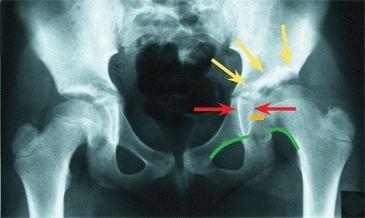
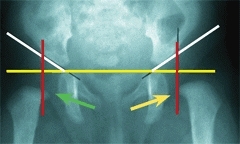
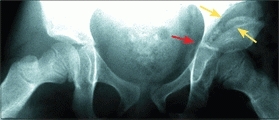
A AP x-ray of pelvis Much can be learned from this simple study. The right hip is normal. Acetabular dysplasia is present on the left. Note the triangular shape of the tear drop (red arrows). Note that the joint space (orange line) is widened. Shenton’s line (green lines) is disrupted. The sourcil, or acetabular roof (yellow arrows), is sclerotic. The left hip joint is slightly higher and more laterally positioned than the normal side.
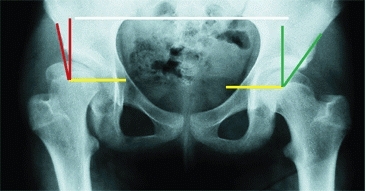
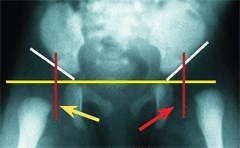
B Center–edge (CE) angle This child has a normal left hip with a CE angle of 30°. The right hip is aspherical and subluxated, and the CE angle is 10°. Note that measures are made with the pelvis level (white line).
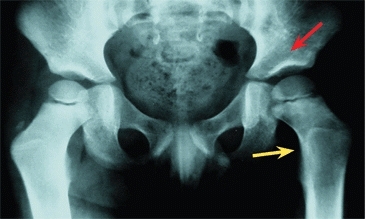
C Hemideossification Note the bone loss of the left hemipelvis (red arrow) due to an osteoid osteoma (yellow arrow) of the proximal femur.
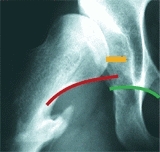
Add other views as necessary. The frog-leg lateral allows comparison of both upper femora. The true lateral is useful in assessing the degree of slip in SCFE, the degree of involvement in Legg–Calvé–Perthes disease, or anterior coverage in DDH [D].

D Lateral x-rays of the proximal femur Frog-leg lateral (red arrow) is only an oblique view. A true lateral (yellow arrow) requires special positioning but provides more information, as it is made at right angles to the AP view. Note the lack of anterior coverage on lateral (red arrow).
Useful special views include the abduction–internal rotation study for hip dysplasia [E], maximum abduction and adduction views for assessing hinge abduction problems, and anteversion studies. Femoral anteversion measurement is seldom necessary.
E Abduction internal rotation (AIR) view The resting position (red arc) shows the hip in a 14-year-old child with cerebral palsy. The hip is subluxated (orange lines), and Shenton’s line (green arc) is disrupted (red arc). The AIR view (yellow arrow) shows improved congruity and less subluxation and restoration of Shenton’s line.
The load-bearing area
of the hip significantly affects its longevity. A reduction in this area may be due to one or more of the following factors:
Simple hip dysplasia
The hip joint is either maldirected or shallow. Both reduce contact area. The depth of the acetabulum is often assessed by the CE angle. This angle increases during childhood as the joint ossifies. At the end of growth, values are like those of adults, with a normal range of 25°–45°. Features of the normal hip are used as a basis for assessing deformity [A] and planning reconstruction.
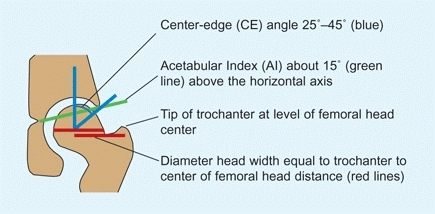
A Normal measurements These are measurements of the normal adolescent hip.
Incongruity reduces contact area
The femoral head is normally round and matches the shape of the acetabulum [B]. An aspherical femoral head is usually due to vascular problems. In the young child, the acetabulum usually remodels to become congruous, and the hip becomes aspherical and congruous [C]. If acetabular remodeling fails to occur, the hip may be aspherical and incongruous—a bad combination.
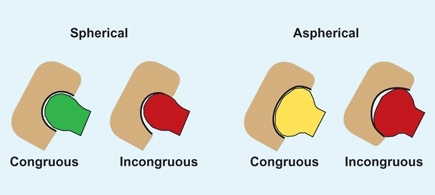
B Congruity Congruity of the hip may be either spherical or aspherical and congruous or incongruous. Incongruity (red) results in areas of excessive load, causing excessive cartilage wear and eventually osteoarthritis.

C Aspherical congruity This deformity resulted from Legg-Calvé-Perthes disease during middle childhood. The head became flattened and the acetabulum remodeled (red arrows) to become congruous.
Displacement of the femoral head
The relationship between the femoral head and acetabulum is normally congruous. If the head is displaced, it becomes subluxated. If all cartilage contact is lost, the joint is dislocated.
Ultrasonography (US)
Ultrasound studies are of greatest value when readily available and performed by an orthopedist in conjunction with the overall evaluation. Cost, restricted access, and operator inexperience may limit value. Ultrasound’s greatest potential usefulness is in assessing DDH in early infancy. Assessing joint effusion, localizing abscesses, and assessing the severity of SCFE, head size in LCP disease, and neck continuity in coxa vara are other applications. This imaging technique is underutilized in North America.
Scintigraphy
Bone scans (BS) are useful in localizing inflammatory processes about the pelvis [D] and in assessing the circulation of the femoral head. Order high-resolution or pinhole-collimated AP and lateral scans of both proximal femora when assessing avascular necrosis (AVN). The bone scan is useful in confirming a preslip and assessing bone tumors.
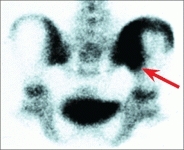

D Imaging options This bone scan shows inflammation of the sacroiliac joint (red arrow), and in a different patient, the MRI shows a slipped epiphysis (yellow arrow).
Arthrography
The usefulness of this procedure is limited, as it is invasive and requires sedation or anesthesia. Arthrography is appropriate to confirm joint penetration in negative taps for suspected joint sepsis and for special situations in managing DDH. The role in LCP disease is more controversial.
Magnetic resonance imaging (MRI)
These studies are the most expensive and require sedation for infants and young children. MRI studies are most useful in assessing intraarticular disorders of the hip. Cartilaginous loose bodies or fracture fragments, deformity of the cartilaginous femoral head, status of the growth plate, and avascular necrosis are usually definable.
Computerized tomography (CT)
Order CT studies to evaluate inflammatory conditions such as an iliopsoas abscess or the configuration of the upper femur and acetabulum. CT scans have replaced tomography in assessing AVN and physeal bridges.
Three-dimensional CT reconstructions are often helpful in visualizing complex deformities of the hip, which is necessary when planning surgery [E].
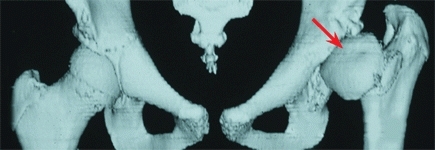
E Three-dimensional CT reconstructions Reconstructions are useful in assessing complex hip deformity prior to surgery. The deformity of the proximal femur (red arrow) is secondary to avascular necrosis associated with DDH management in infancy.
Hip and Pelvic Pain
The causes of hip and pelvic pain are numerous [A], sometimes making the diagnosis difficult.
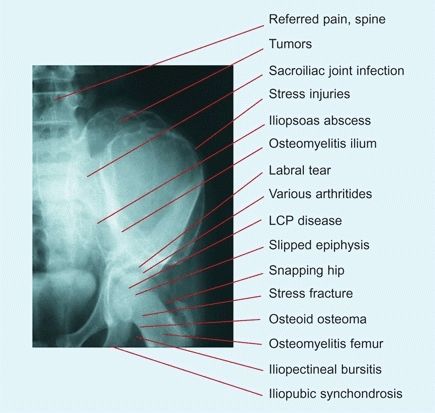
A Causes of hip pain in children The differential diagnosis is extensive.
Diagnosis
Detailing these features may help to establish the diagnosis.
Age
Consider the age of the child with hip pain [B]. For example, LCP disease is most common in boys in middle childhood [B]. SCFE must be considered in the older child or adolescent. Overuse syndromes are most common in the adolescent.
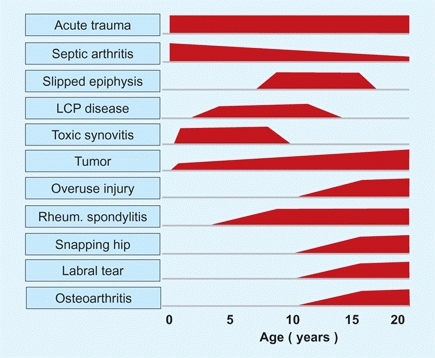
B Hip pain causes by usual age of onset These are ages when conditions are most common.
Onset
Acute onset is suggestive of injury or a rapid onset of infection. SCFE may be chronic or sudden. Acute slips are characterized by a mild injury and inability to walk. LCP disease onset is usually insidious. Overuse syndromes are most painful when active.
Spontaneous movement
The most consistent physical finding for septic arthritis of the hip is a loss of spontaneous movement of the affected limb.
Systemic illness
The child is ill with septic arthritis, and less sick with toxic synovitis, rheumatoid spondylitis, and tumors.
Resting position of the limb
Intraarticular hip disorders usually result in the spontaneous positioning in slight flexion and lateral rotation [C]. This position reduces the intraarticular pressure.

C Observation Observation revealed pseudoparalysis of the left leg, and the left hip is positioned in slight flexion and external rotation. These findings are typical for septic arthritis of the left hip.
Tenderness
Palpate to determine the site of tenderness [D].
D Thigh tenderness Palpate for localized tenderness.
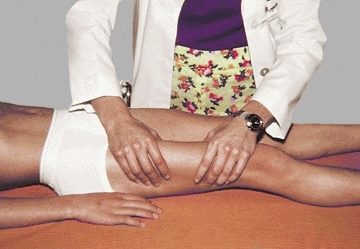
Hip rotation test
Guarding and a loss of medial rotation suggest the problem is within the joint [E].

E Hip rotation test This child has reduced medial rotation of the right hip due to toxic synovitis.

F Joint damage from septic arthritis Note the severe joint damage from septic arthritis treated two weeks after onset.
Night pain
Nocturnal pain suggests the possibility of a malignant tumor.
Back stiffness
Limitation of forward bending suggests that the disorder may be referred from the spine.
Causes
Establish the diagnosis by considering the features and the common causes of hip pain [A].
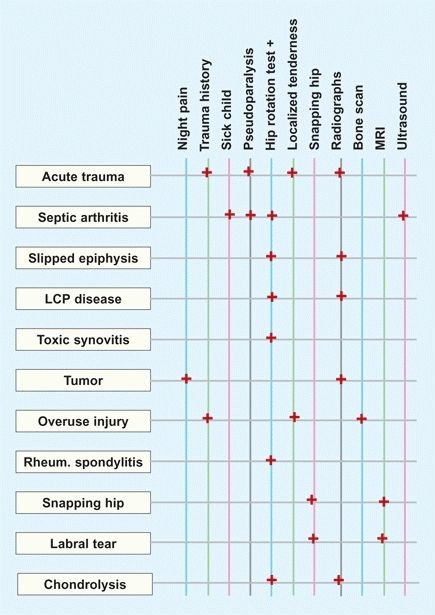
A Hip pain and major diagnostic features These are some of the major clinical features that differentiate each cause of pain.
Infection
is a common cause of pelvic pain. The early diagnosis of septic arthritis is critical because it may severely damage or destroy the hip joint [F, previous page]. Because of the tenuous vascularity of the hip, joint infections must be diagnosed and drained promptly. Soft tissue abscess, such as the psoas abscess, may be suspected by the finding of tenderness on rectal examination and soft tissue swelling on the AP radiograph of the pelvis. Confirm the diagnosis by CT or MRI studies. Sacroiliac infections are identified by bone scans.
Stress injuries
or repetitive microtraumas may cause hip pain. Such pain is most common during the second decade and often follows vigorous activity. It may involve the upper femur, but more commonly it involves the origin of muscles such as the greater trochanter and iliac spines. The diagnosis is usually suggested by the history, physical findings of well-localized tenderness, and negative radiographs but a positive bone scan.
Tumors
A variety of tumors occur about the hip and pelvis. Osteoid osteoma is common in the proximal femur and produces pain in a pattern that is nearly diagnostic. The pain is nocturnal and relieved by aspirin. The tumor produces reactive bone with a radiolucent nidus on conventional radiographs [B].

B Osteoid osteoma These lesions are common in the proximal femur and cause night pain.
Toxic synovitis
(or transient synovitis) is a idiopathic benign inflammation of the hip joint [C] that occurs in children. This condition is important, as it may be confused with septic arthritis and less commonly with LCP disease. The condition causes pain and irritability of the hip. It subsides spontaneously over several days.
C Toxic synovitis The hip is often positioned in slight flexion and external rotation (red arrow). Ultrasound studies often show an effusion (yellow arrow).
Idiopathic chondrolysis
This uncommon condition is seen in late childhood or adolescence. The hip becomes painful and stiff, and joint space narrowing is present [D]. See page 228.


D Chondrolysis This hip shows narrowing of the joint space on conventional radiographs (red arrow), and the arthrogram (yellow arrow) shows thinning of the cartilage on the femoral head.
Rheumatoid spondylitis
Unlike juvenile rheumatoid arthritis, hip involvement may be the first sign of rheumatoid spondylitis. Establish the diagnosis with serologic tests.
Developmental Hip Dysplasia
DDH is a generic term describing a spectrum of anatomic abnormalities of the hip that may be congenital or develop during infancy or childhood. The spectrum covers mild defects such as a shallow acetabulum to severe defects such as teratologic dislocations. Teratologic dislocations occur before birth and include severe deformity of both the acetabulum and proximal femur.
Incidence
DDH incidence depends on how much of the spectrum is included [A]. At birth, hip instability is noted in 0.5–1% of joints, but classic DDH occurs in about 0.1% of infants. The incidence of mild dysplasia contributing to adult degenerative arthritis is substantial. It is thought that half of the women who develop degenerative arthritis have preexisting acetabular dysplasia.
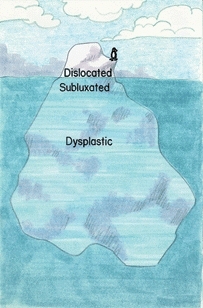
A Spectrum of hip dysplasia Dislocated hips are usually diagnosed during infancy, but hip dysplasia may not become evident until adult life and then present as degenerative arthritis.
Etiology
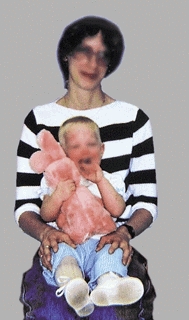
DDH is considered to be inherited by a polygenic mode. DDH is more common in breech deliveries [B], in children with joint laxity [C], and in girls.

B Breech association DDH is often associated with breech presentation.

C DDH and joint laxity Children with DDH often show excessive joint laxity.
Pathology
The acetabulum is often shallow and maldirected. The proximal femur shows antetorsion and coxa valga. Structural interpositions between the displaced femoral head and acetabulum are common [D]. The iliopsoas tendon is insinuated between the femoral head and acetabulum, causing a depression in the joint capsule. This gives the capsule an hourglass configuration. The acetabular labrum is inverted into the joint, the ligamentum teres is enlarged, and the acetabulum may contain fat (pulvinar).
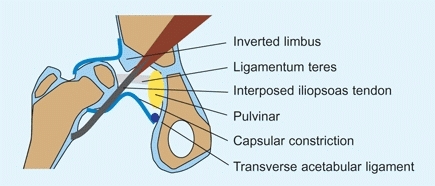
D Structures blocking reduction in DDH These interpositions may block reduction of the hip.
Natural History
Residual acetabular dysplasia is common in DDH. This may occur even following an apparently good early reduction [F]. The disability from dysplasia is related to the degree of displacement [E]. Greater displacement causes more function disability. Pain is most common with severe subluxation or articulation in a false acetabulum [G].
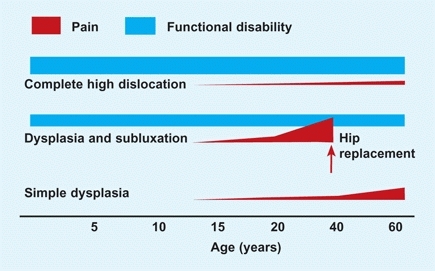
E Conceptual chart showing disability from DDH Pain, altered function, and cosmetic problems often result from persisting hip deformity due to DDH.
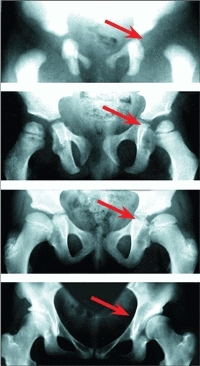
F DDH with residual acetabular dysplasia Radiographs at birth, 3, 10, and 19 years (top to bottom) show persisting dysplasia.

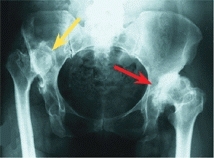
G Adult degenerative arthritis Note that arthritis is most severe in the subluxated (red arrow) hip as compared with the totally dislocated hips (yellow arrows).
Diagnosis
The early diagnosis of DDH is critical to a successful outcome. Acetabular development is abnormal if a hip is subluxated or dislocated. Delays in management result in residual abnormalities and eventual degenerative arthritis.
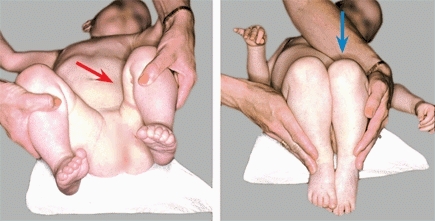
Neonatal examination
Every newborn should be screened for signs of hip instability. The hip should be examined using both the Barlow and Ortolani techniques [A and B]. Examine one hip at a time. The infant should be quiet and comfortable so the muscles about the hip are relaxed. Use no force. Test for instability in several positions.

A Barlow’s sign Hip instability is demonstrated by attempting to gently displace the hip out of the socket over the posterior acetabulum.

B Ortolani’s sign The thigh is first adducted and depressed to subluxate the hip. The thigh is then abducted. The hip reduces with a palpable “clunk.”
Changing manifestations of DDH
The signs of DDH change with the infant’s age [C]. For example, the incidence of hip instability declines rapidly, 50% within the first week. The classic findings of stiffness and shortening increase over the first few weeks of life. These signs become well established in the older infant [D].
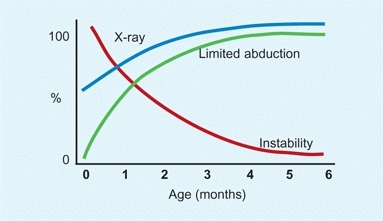
C Changing signs of DDH With increasing age, signs change.
D DDH in older infant Note the limited abduction (red arrow) and shortening (blue arrow) on the affected left side.
Repeated examinations
The hip should be examined during each “well baby” examination. In the neonatal period, DDH is detected by different signs, based on the infant’s age. In early infancy, instability is the most reliable sign. Later, limitation of abduction and shortening are common. Beware of bilateral dislocations, as they are more difficult to identify [E]. If hip abduction is less than about 60° on both sides, order an imaging study.

E Bilateral DDH This girl has symmetrical bilateral dislocations. The hip symmetry makes early diagnosis more difficult. Note the typical lumbar lordosis (arrow) that occurs with high dislocations.
Mother’s intuition
Although not proven, a common clinical experience is the accuracy of the mother’s sense that something is wrong. Take the mother’s intuition seriously [F].

F Mother’s intuition This mother had DDH as a child. She suspected that her son’s hip was abnormal, but the primary care physician found nothing on examination. She insisted on a radiograph. This study demonstrated a dislocation (red arrow). This scenario is not uncommon.
Hip-at-risk factors
The presence of several factors increase the risk of DDH [A and C]. When risk factors are present, the infant should be examined repeatedly and the hip imaged by ultrasound or radiography.
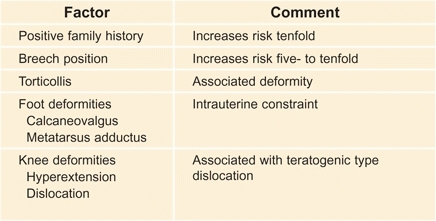
A Risk factors These factors increase the risk of DDH and signal the need for careful and repeated examinations and imaging studies.
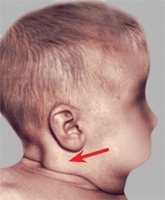
C DDH and torticollis This infant showed the typical features of muscular torticollis with a sternocleidomastoid tumor (red arrow). A radiograph of the pelvis demonstrated DDH.
Hip “clicks” and asymmetrical thigh folds
Hip clicks are fine, short-duration, high-pitched sounds that are common and benign. These are to be differentiated from “clunks,” the sensation of the hip being displaced over the acetabular margin. Clicks and asymmetrical thigh folds are common in normal infants [B].

B Asymmetrical thigh folds These occur in up to 20% of normal infants.
Radiography
Radiographs become progressively more diagnostic with increasing age. By 2–3 months of age, radiography is reliable and this is the optimum age for screening by this method. A single AP radiograph is adequate. Draw the reference lines and measure the acetabular index. Normally, the AI in early infancy falls below 30°, is questionable in the 30°–40° range, and abnormal if above 40°. Hip subluxation or dislocation may often be demonstrated by the metaphysis of the femur positioned lateral to the lateral acetabular marginal line [D].
D Assessing radiographs in early infancy Note that in the normal hip (green arrow) the femoral metaphysis lies medial to the acetabular line. In the subluxated hip (yellow arrow) and dislocated hip (red arrow) the metaphysis falls progressively more lateral.
Ultrasound imaging
The effectiveness of ultrasound imaging depends upon the skill and experience of the examiner. A skillful ultrasound evaluation is an effective screening technique for DDH [E]. The major problem with this screening is in the interpretation of the findings. If the hip is unstable, imaging is unnecessary. Imaging is appropriate to evaluate a suspicious finding, when hip-at-risk factors are present, and to monitor the effectiveness of treatment.
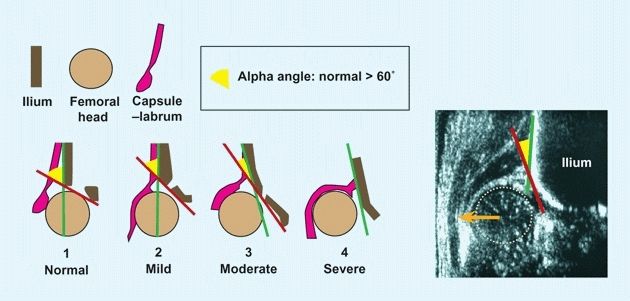
E Graf grading of DDH by ultrasound Drawing shows how the hips can be graded by measurements based on the ultrasound evaluation. The grades shown are divided by Graf into four types. Each is subdivided into subtypes (not shown). Reference lines are drawn to show the iliac margin (green), and the joint inclination (red). The alpha angle (yellow arc) can be constructed to show severity. The ultrasound image shows a severe displacement (orange arrow) of the femoral head (tan circle) in an infant with DDH.
Documentation
Document your hip evaluation. The failure to diagnose DDH is a common cause of suits against physicians. If the diagnosis is delayed, a record showing that appropriate examinations of the hip were made provides the best defense. DDH may be missed by even the most skilled examiners. Failure to screen for DDH is not acceptable by current standards.
Management
The management of DDH is challenging. Delays in diagnosis or problems in management often lead to residual anatomic defects and subsequent degenerative arthritis. The objectives of management include early diagnosis, reduction of the dislocation, avoidance of avascular necrosis, and correction of residual dysplasia.
Birth to 6 Months
This is the ideal age for management [A]. Treat DDH in this age group first with an abduction orthosis such as the Pavlik harness.
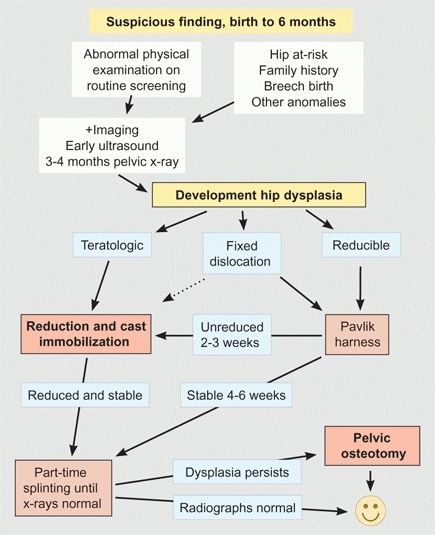
A DDH management flowchart, birth to 6 months
Pavlik harness
This widely used orthosis allows motion in flexion and abduction. Be certain that it is fitted properly [B], both initially and as applied by the parents. Advise the family on ways of transporting the infant [C and E].
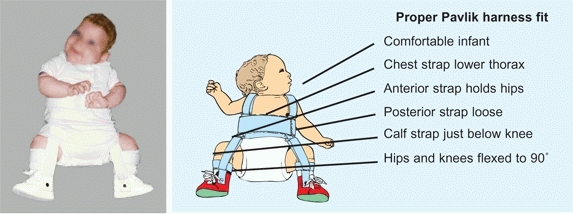
B Proper fit of Pavlik harness The harness should be carefully fitted. Make certain it is the proper size for the infant. The harness must be comfortable. Check the fit after the parent applies the harness to assess problems before the parent leaves the clinic.

C DDH mobility These carriers are ideal, as they provide abduction, mobility, and comfort for the infant and parent.



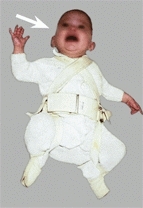
E DDH splints and car transportation These splints should fit into standard infant car seats.
See the infant weekly in the brace. Make certain the brace is being fitted properly [D] and progress is being made. The hip should become progressively more stable.

D Pitfalls in management Triple diaper management (orange arrow) is ineffective and gives a false sense that treatment has been initiated. Pavlik harness errors are common. Make certain that the straps are not too tight (red arrows), the calf strap is not too low (yellow arrow), and the infant is comfortable (white arrow).
If harness treatment is successful, continue full-time bracing for 6–8 weeks to allow the hip to become stable. Monitor with ultrasound imaging or by AP radiographs of the pelvis about every 2–4 weeks. Continue the brace at night until the radiographs are normal.
If a dislocated hip has not reduced by 3–4 weeks, abandon Pavlik treatment. Persisting with this treatment may cause head deformity and posterior fixation, making closed reduction difficult or impossible. Proceed with closed or open reduction. Manage as is described for infants over 6 months of age.
Night splinting
After the hip is reduced and stable, continue with night splinting to facilitate acetabular development. Continue until the radiographs are normal. A simple abduction splint is inexpensive and is well accepted by the infant.
6 to 18 Months
In this age group, most cases of DDH can be managed by closed reduction and spica cast immobilization [A and C].

A Home traction Setup at home is less expensive, less stressful for the infant, and often more convenient for the family.

C Spica cast immobilization Infants require cast immobilization to retain the reduction of a dislocated hip.
Traction
The need for traction is controversial. The current practice is to omit traction in most cases. Traction may be useful if the hip is stiff and closed treatment is planned. Use home traction when possible. Maintain for about 3 weeks with the legs flexed and abducted about 45° with 2–3 pounds of traction applied to each limb [B].
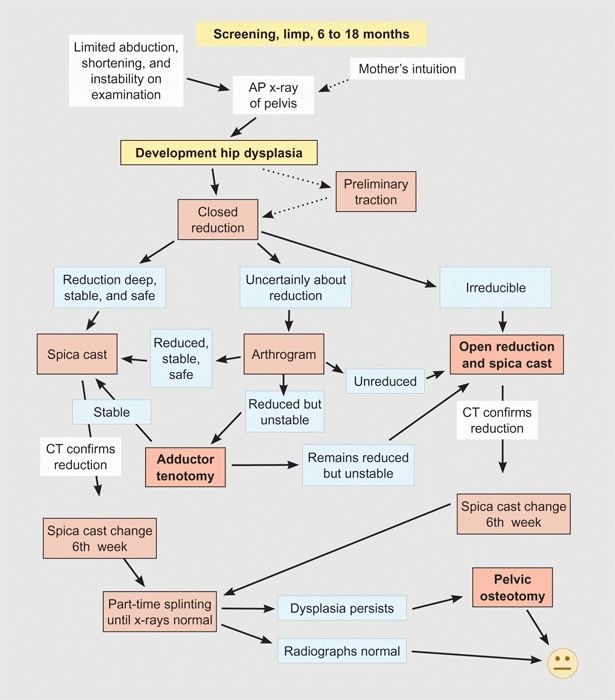
B DDH management flowchart, 6 to 18 months
Scheduling
Schedule and obtain consent for a closed, or possibly open, reduction.
Reduction
by closed means is first tried. If unsuccessful, open reduction is required.
Arthrography
is useful when the quality of reduction is uncertain or the decision regarding management is difficult.
Follow-up
After reduction, the infant should be followed carefully to assess the effect of time on growth, reduction, and acetabular development. Follow with AP radiographs made quarterly through infancy, yearly though early childhood, and then about every third year during middle and late childhood. The frequency of follow-up studies should be individualized based on the severity of any residual dysplasia.
18 to 30 Months
In this age group, operative management is usually required [A]. Occasionally, an infant with a “loose dislocation” can be managed as described in the flowchart for infants 6–18 months of age [B, previous page]. If the hip is unusually stiff, be prepared to add femoral shortening, as described for management of children over 30 months of age (next page).
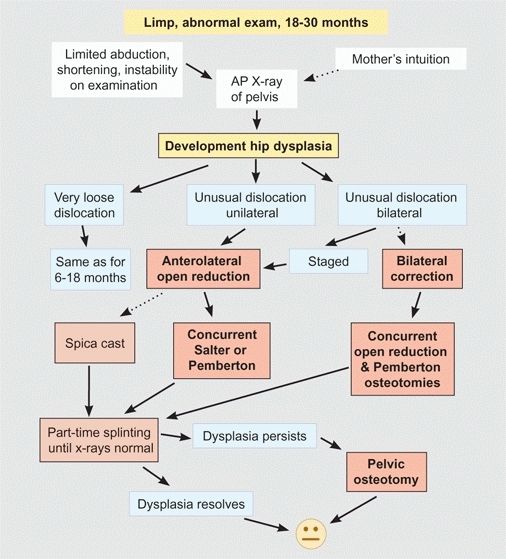
A DDH management flowchart, 18 to 30 months.
Management
Manage with an open reduction through an anterolateral approach and perform a concurrent Salter or Pemberton osteotomy. The open reduction is technically challenging. Add the pelvic osteotomy to improve results and save the child a second procedure.
Open reduction
is the most difficult part of the procedure. The pelvic osteotomies are relatively simple, but the reduction can sometimes be difficult. The open reduction requires good exposure, careful dissection to minimize the risk of avascular necrosis, and a concentric reduction. The obstacles to reduction must be corrected [C].
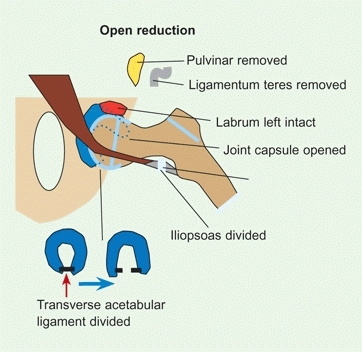
C Open reduction Open reduction is often difficult, and obstruction must be corrected.
Iliopsoas tendon
This tendon is interposed between the femoral head and acetabulum and must be released.
Capsular constriction
Open the capsule widely to ensure a complete release.
Transverse acetabular ligament
This structure lies across the base of the acetabulum and will block a deep concentric reduction unless released.
Pulvinar
is fatty fibrous tissue that often fills the depth of the acetabulum. Remove with a rongeur.
Ligamentum teres
is elongated and sometimes hypertrophied. Removal is usually required. The vascular contribution through this ligament is minimal.
Limbus
is often inverted and hypertrophied. Do not excise this structure. Once the hip is concentrically reduced, the limbus will remodel and form the labrum, an important structure for hip stability and longevity.
Concurrent osteotomy
This choice may be based on the pathology and on the experience and preference of the surgeon.
Femoral osteotomy
Proximal femoral varus osteotomy is becoming less commonly used because the acetabular dysplasia is the more significant deformity. Include only minimal rotational correction.
Salter innominate osteotomy
is suitable for unilateral mild to moderate dysplasia. The procedure is simple, risks are few, and results good.
Pemberton pericapsular osteotomy
[B] is more versatile because it can be performed bilaterally, does not destabilize the pelvis, provides greater correction, and requires no internal fixation. Avoid overcorrection. Stiffness is more common with this procedure, as the operation changes the shape of the acetabulum.
B Pemberton pericapsular osteotomy The osteotomy hinges at the triradiate cartilage (red arrow) and graft wedges open the osteotomy (yellow arrows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








