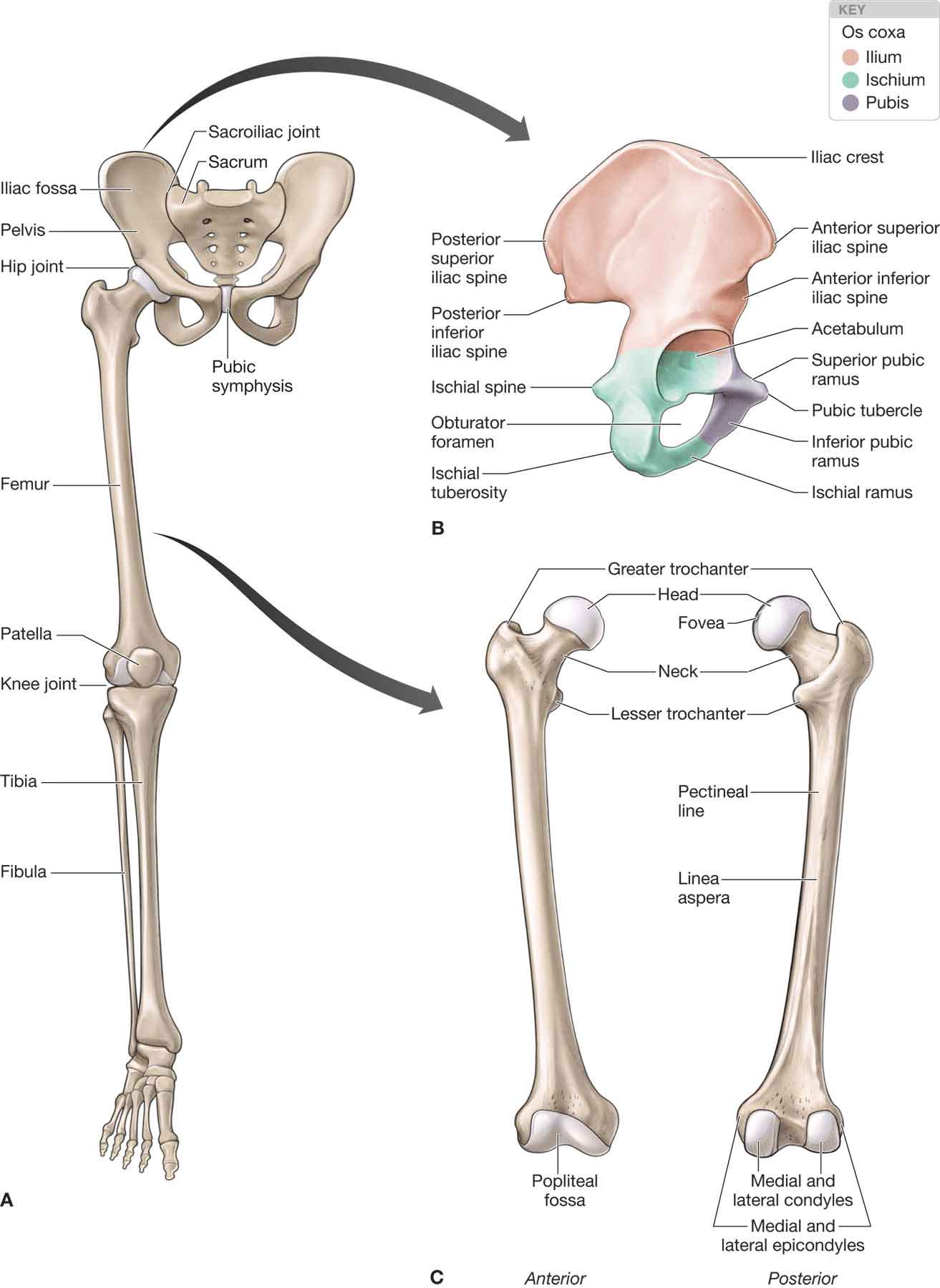
The structure and design of the hip allow for both mobility and stability,1 the latter of which is particularly important for weight bearing and ambulation. In the human body, the center of gravity is located at the second sacral vertebral level, several segments above and medial to the femoral head. Control of the body mass from such a distant fulcrum requires the generation of significant counterbalance forces as well as the ability of the joint to sustain both high compression and tensile strains.2 Thus, a major function of the hip joint is to provide a pathway for the transmission of forces between the pelvis and the lower extremities. The hip articulation is formed by the head of the femur and the acetabulum of the pelvic bone (Fig. 19-1). This articulation is classified as an unmodified ovoid (or ball and socket) joint. The hip joint which, although similar in nature to the shoulder joint, differs in the fact that the former has a deeper acetabular socket and acts as a weight-bearing joint with a smaller total arc of motion. FIGURE 19-1 Bones of the lower extremity. (Reproduced, with permission, from Chapter 34. Overview of the Lower Limb. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
CHAPTER 19
Hip
OVERVIEW
ANATOMY
Bony Anatomy
Normal hip joint growth and development occur because of a genetically determined balance of growth of the acetabulum and the presence of a strategically located spherical femoral head.3–7
The os coxa (hip bone), more commonly referred to as the innominate bone initially begins life as three individual bones: the ilium, the ischium, and the pubis (Fig. 19-1). As life progresses, these three bones fuse together.
Ilium
The ilium (Fig. 19-1) is the largest of these three bones. It is composed of a large fan-like wing (ala) and an inferiorly positioned body. The body of the ilium forms the superior two-fifths of the acetabulum.
 The wing of the ilium spans superiorly from the posterior superior iliac spine (PSIS) to the anterior superior iliac spine (ASIS). The wing serves as the insertion of the gluteus minimus, medius, and maximus.
The wing of the ilium spans superiorly from the posterior superior iliac spine (PSIS) to the anterior superior iliac spine (ASIS). The wing serves as the insertion of the gluteus minimus, medius, and maximus.
 The anterior surface of the ilium forms a fossa and serves as the proximal attachment of the iliacus muscle.
The anterior surface of the ilium forms a fossa and serves as the proximal attachment of the iliacus muscle.
Ischium
The ischium (Fig. 19-1) is composed of a body, which contributes to the acetabulum, and a ramus. The ischium forms the posterior two-fifths of the acetabulum. Together, the ischium and the ramus form the ischial tuberosity. The ischial tuberosity is an important landmark for palpation, as it serves as the attachment for several muscles (Table 19-1) and the sacrotuberous ligament. The ischial spine, located on the body of the ischium, serves as the attachment for the sacrospinous ligament.
TABLE 19-1 | Muscles That Attach to the Ischial Tuberosity |
Semimembranosus Semitendinosus Long head of the biceps femoris Adductor magnus Quadratus femoris Gemellus inferior |
Pubis
The pubis (Fig. 19-1) is the smallest of the three bones and consists of a body and inferior and superior rami. The pubis forms the anterior fifth of the acetabulum.
Acetabulum
The ilium, ischium, and pubis fuse together within the acetabulum and form a deep-seated depression in the lateral pelvis, which allows for the proximal transmission of weight from the axial skeleton to the lower extremity.8 The orientation of the surface of the acetabulum faces laterally, inferiorly, and anteriorly (Fig. 19-1). The superior and posterior margins of the acetabulum are reinforced with a compact cortical bone, which extends the peripheral brim of the fossa, enhancing the stability of the joint during weight bearing from both flexed and extended positions.8 The coverage of the femoral head by the acetabulum is measured by the center edge angle (CEA) of Wiberg (see Clinical Pearl below). The absence of a normal femoral head during growth, such as in developmental dysplasia of the hip (DDH), causes the acetabulum to have a flat shape. A deformed head stimulates the formation of a correspondingly deformed acetabulum if the deformation occurs at a young enough age.3
Hip dysplasia is considered to be the result of undercoverage of the femoral head. This bony undercoverage can lead to excessive joint stress during normal function. For example, a situation of edge loading of the acetabulum can lead to premature articular cartilage degeneration, hip dysplasia, anteversion, coxa valga, or acetabular labral injury.11 Conversely, excessive bone coverage, or overcoverage can predispose an individual to hip injury secondary to alterations in the mechanical loading patterns of the hip joint.11 Overcoverage usually is indicative of pathologies such as pincer impingement, acetabular retroversion, or profundus/protrusion.
While the majority of acetabular development is determined by the age of eight,12–14 the depth of the acetabulum increases additionally at puberty, because of the development of three secondary centers of ossification.3,4,15 Around the periphery of the acetabulum is a thickened collar of fibrocartilage known as the acetabular rim, or labrum (see “The Acetabular Labrum”), that further deepens the concavity and grasps the head of the femur.8 The transverse acetabular ligament is a fibrous tissue link spanning the inferior acetabular notch that connects the anteroinferior and posteroinferior horns of the semilunar surface of the acetabulum. The posterior aspect of the ligament attaches to the bone beneath the lunate surface, and the anterior aspect attaches to the labrum.16 The transverse acetabular ligament contains no cartilage cells.17 The function of this ligament in the hip is currently unknown.
The articular surface of the acetabulum is limited to an inverted horseshoe-shaped area covering the anterior, superior, and posterior margins.8 The articular cartilage is thickest on the superior aspect of the acetabulum, but thins near the center of the joint, and is absent over the acetabular notch (Fig. 19-1), the area occupied by the ligamentum teres and obturator artery.18 This relatively small contact area may contribute to the prevalence of degenerative disease of the hip joint in humans.19 The diameter of the acetabulum is slightly less than that of the femoral head and results in an incongruous fit of the joint surfaces. This incongruity unloads the joint during partial weight bearing (PWB), by allowing the femoral head to sublux laterally out of the cup, while, in full weight bearing, the femoral head is forced into the acetabulum.8 In addition, elastic deformation of the acetabulum increases joint congruency of the two-joint surfaces in weight bearing.20 Finally, a strong vacuum contributes to the joint coaptation.1
Femur
The femur is the strongest and the longest bone in the body. The proximal end of the femur, the femoral head, articulates with the acetabulum to form the hip joint (Fig. 19-1). The femoral head is composed of a trabecular bone core encased in a thin cortical bone shell. Approximately two-thirds of the femoral head is covered with a smooth layer of cartilage except for a depression, the fovea capitis, which serves as the attachment of the ligamentum teres. The articular cartilage is thickest on the superior-posterior aspect of the femoral head.
Both the trabecular framework of the head and its pliable hyaline cartilage covering contribute toward the shaping of the femoral head within the acetabulum during full weight bearing.8
The neck of the femur is located between the shaft of the femur and its head. The head–neck offset is measured by the alpha angle. This angle, which determines how spherical the femoral head is, is measured by first drawing a best-fit circle around the femoral head and then drawing a line from this down the femoral neck. The alpha angle is formed between this line and a line drawn from the center of the circle to where the femur deviates from the circle. An alpha angle of greater than 55 degrees is indicative of a condition called cam impingement, described later.
In the frontal plane, the femoral neck lies at an angle to the shaft of the femur. This neck–shaft angle, or angle of inclination, is normally 125–139 degrees in the adult population.22 Femoral varus (coxa varum) occurs when the angle of inclination is less than 125 degrees, and femoral valgus (coxa valgus) occurs when the angle is greater than 139 degrees (see “Biomechanics”).
In the transverse plane, the proximal femur is oriented anterior to the distal femoral condyles as a result of a medial portion of the femur.23 The normal range for femoral alignment in the transverse plane in adults is 15–20 degrees of anteversion, depending on the level of the acetabulum.24,25 Increased anteversion is greater than 25 degrees, and relative retroversion occurs at less than 10 degrees. Absolute retroversion occurs at an angle less than 0 degree. Typically, an infant is born with about 30 degrees of femoral anteversion.26,27 This angle usually decreases to 15 degrees by 6 years of age because of bone growth and increased muscle activity.
On the anterior surface of the femoral neck is the rough intertrochanteric line. The femoral neck serves to extend the weight-bearing forces lateral and inferior to the joint fulcrum. The intertrochanteric crest marks the posterior junction between the neck and the shaft of the femur. The greater trochanter serves as the insertion site for several muscles that act on the hip joint (Table 19-2). The lesser trochanter, located on the posteromedial junction of the neck and the shaft of the femur, is created by the pull of the iliopsoas muscle.
TABLE 19-2 | Muscles That Attach to the Greater Trochanter |
Piriformis Gluteus medius Gluteus minimus Obturator internus Gemellus superior Gemellus inferior |
The head of the femur is angled anteriorly, superiorly, and medially. The femoral neck is externally rotated with respect to the shaft. The angle that the femoral neck makes with the acetabulum is called the angle of anteversion/declination (see “Biomechanics”).
Joint Capsule
The joint capsule of the hip (Fig. 19-2), a substantial fibrous sleeve, attaches proximally to the pelvis just lateral to the acetabular labrum and extends laterally over the femoral head and neck to attach to the intertrochanteric line anteriorly. Posteriorly, the capsule attaches to the lateral one-third of the femoral neck allowing for the attachment of the obturator externus tendon in the posterior intertrochanteric fossa.8 The joint capsule is thicker anterosuperiorly, where maximal stress and weight bearing occurs, and thinnest posteroinferiorly. The joint capsule has three thickened regions that constitute the capsular ligaments. These anterior capsular thickenings, which have been studied extensively, include the iliofemoral ligament and the pubofemoral ligament. Despite these studies, the exact functions of each of these ligaments are still debatable.
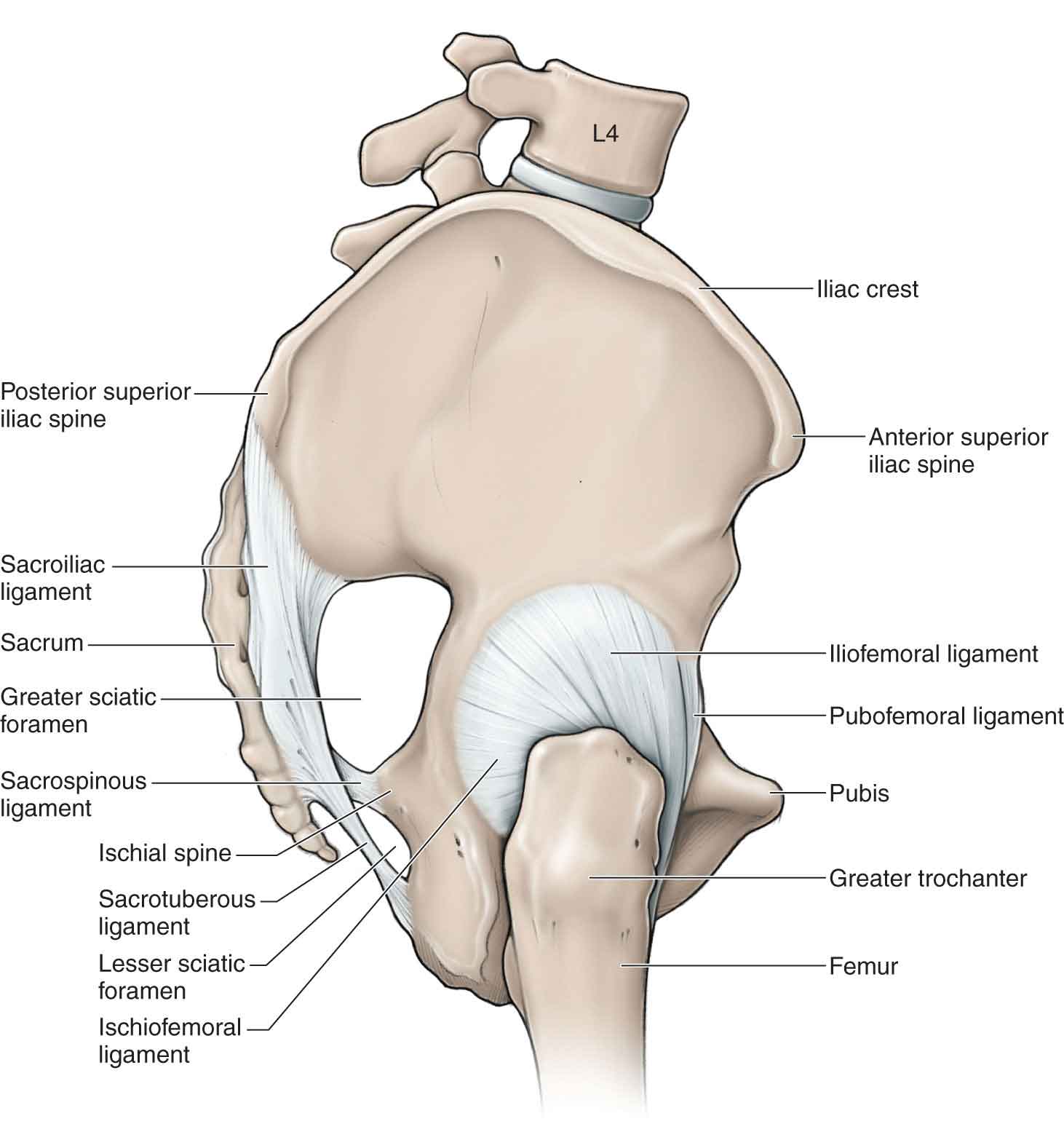
FIGURE 19-2 The hip joint capsule. (Reproduced, with permission, from Chapter 35. Gluteal Region and Hip. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
 The iliofemoral ligament (Y ligament of Bigelow) (Fig. 19-2) is triangular in shape and consists of two parts: an inferior (medial) portion and a superior (lateral) portion making it resemble an inverted Y. The iliofemoral ligament is the strongest ligament in the body and reinforces the anterior aspect of the hip joint. The ligament, which attaches to the anterior inferior iliac spine (AIIS) at its apex, is oriented superior laterally and blends with the iliopsoas muscle. The medial portion inserts into the inferior aspect of the trochanteric line, while the lateral portion inserts onto the superior aspect of the trochanteric line. By limiting the range of hip extension, this ligament, with the assistance of the pubofemoral ligament, allows maintenance of the upright posture and reduces the need for contraction of the hip extensors in a balanced stance. The ligament exhibits the greater stiffness and prevents anterior translation during extension and external rotation,28 in both flexion and extension.29 Myers et al.30 reported that the iliofemoral ligament significantly limited external rotation and anterior translation of the femoral head and was supported by the labrum acting as a secondary stabilizer.9 Hip adduction tightens the superior portion of the iliofemoral ligament.
The iliofemoral ligament (Y ligament of Bigelow) (Fig. 19-2) is triangular in shape and consists of two parts: an inferior (medial) portion and a superior (lateral) portion making it resemble an inverted Y. The iliofemoral ligament is the strongest ligament in the body and reinforces the anterior aspect of the hip joint. The ligament, which attaches to the anterior inferior iliac spine (AIIS) at its apex, is oriented superior laterally and blends with the iliopsoas muscle. The medial portion inserts into the inferior aspect of the trochanteric line, while the lateral portion inserts onto the superior aspect of the trochanteric line. By limiting the range of hip extension, this ligament, with the assistance of the pubofemoral ligament, allows maintenance of the upright posture and reduces the need for contraction of the hip extensors in a balanced stance. The ligament exhibits the greater stiffness and prevents anterior translation during extension and external rotation,28 in both flexion and extension.29 Myers et al.30 reported that the iliofemoral ligament significantly limited external rotation and anterior translation of the femoral head and was supported by the labrum acting as a secondary stabilizer.9 Hip adduction tightens the superior portion of the iliofemoral ligament.
 The pubofemoral ligament (Fig. 19-2) blends with the inferior band of the iliofemoral, and with the pectineus muscle. The orientation of the pubofemoral ligament is more inferior-medial. The ligament attaches medially to the iliopectineal eminence, the superior pubic ramus, and the obturator crest and membrane, and laterally to the anterior surface of the trochanteric line. Its fibers tighten in extension, as with the other hip ligaments, and also tighten in external rotation29 and reinforce the joint capsule along the medial surface.
The pubofemoral ligament (Fig. 19-2) blends with the inferior band of the iliofemoral, and with the pectineus muscle. The orientation of the pubofemoral ligament is more inferior-medial. The ligament attaches medially to the iliopectineal eminence, the superior pubic ramus, and the obturator crest and membrane, and laterally to the anterior surface of the trochanteric line. Its fibers tighten in extension, as with the other hip ligaments, and also tighten in external rotation29 and reinforce the joint capsule along the medial surface.
 The ischiofemoral ligament, which accounts for the posterior thickening of the capsule (Fig. 19-2), winds posteriorly around the femur and attaches anteriorly, strengthening the capsule. This ligament, which tightens with internal rotation of the hip in flexion and extension, as well as adduction of the flexed hip, is more commonly injured than the other hip ligaments.
The ischiofemoral ligament, which accounts for the posterior thickening of the capsule (Fig. 19-2), winds posteriorly around the femur and attaches anteriorly, strengthening the capsule. This ligament, which tightens with internal rotation of the hip in flexion and extension, as well as adduction of the flexed hip, is more commonly injured than the other hip ligaments.
All of these capsular thickenings/ligaments are taut in hip extension, especially the inferior portion of the iliofemoral ligament. Conversely, all the ligaments are relaxed in hip flexion. Because of their inherent strength, the hip ligaments are only usually compromised with severe macrotrauma involving a fracture/dislocation of the hip.
The ligamentum teres, or capitis femoris ligament (Fig. 19-3), an embryonic remnant, is a structure seen only in the hip joint.8 This ligament spans the hip joint running from the edges of the acetabular notch to the fovis capitis of the femur, attaching the femoral head to the inferior acetabular rim. The ligament is entirely enclosed by a synovial membrane, which forms a sheath around the ligament. Within this sheath, vessels and nerves pass to the femoral head, providing an important source of arterial blood from a tiny posterior branch of the internal iliac artery during femoral head vascular development. Although this arterial supply is a significant source of blood to the femoral head in infants and children,31 it becomes less significant in adulthood, because of collateral circulation from the circumflex arteries (see “Vascular Supply”) surrounding the femoral neck, although chronic interruption of the blood supply to the femoral head has been associated with osteonecrosis and degenerative arthritis.32
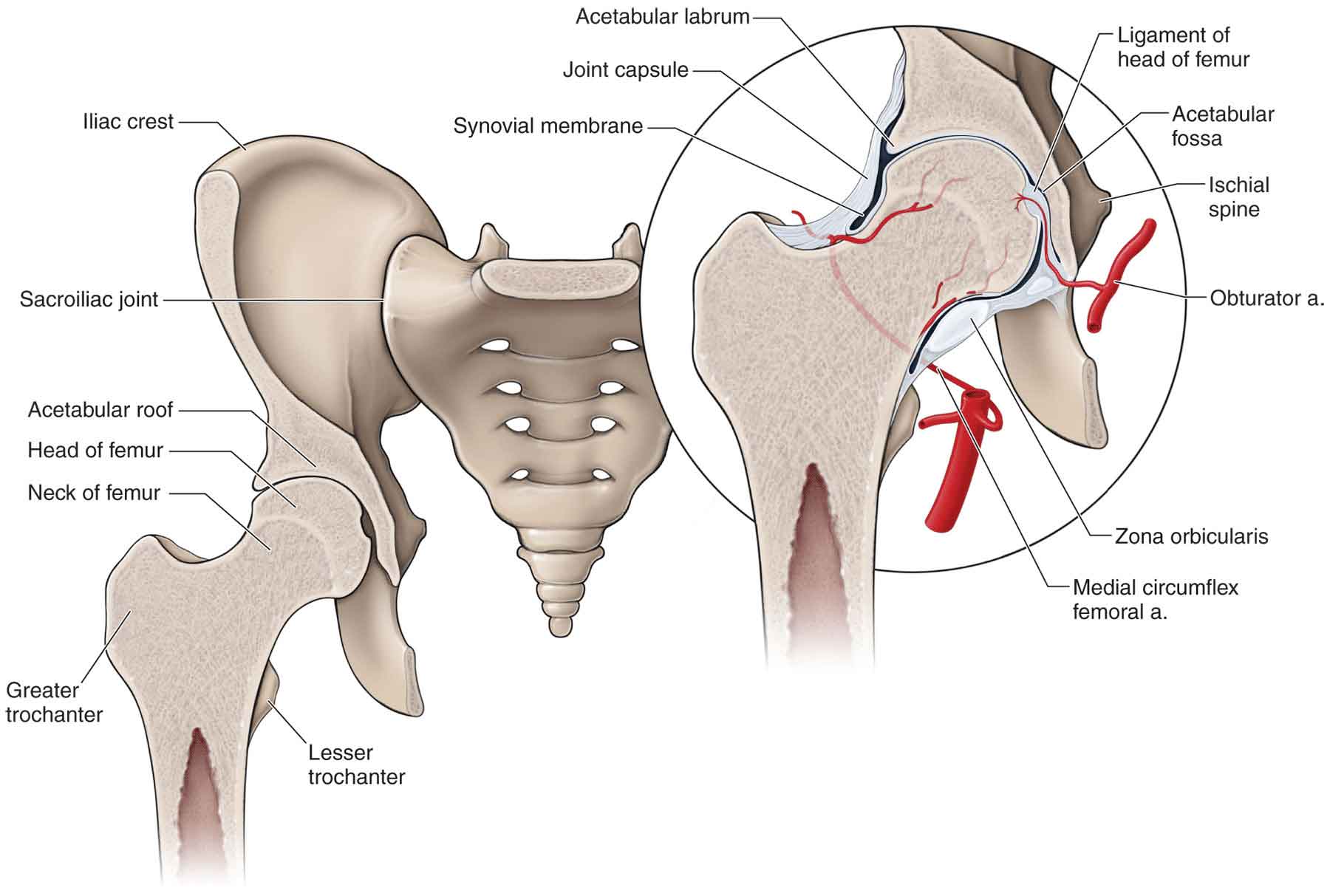
FIGURE 19-3 The hip joint. (Reproduced, with permission, from Chapter 35. Gluteal Region and Hip. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
Though traditionally thought to play a minimal role in joint function, more recent findings suggest that the ligamentum teres may play a number of key roles in stabilization.34–37 It would appear that the ligamentum teres can function analogous to the anterior cruciate ligament as a stabilizer against subluxation of the hip, particularly when the hip is externally rotated in flexion or internally rotated in extension.38 Although not a major stabilizer, a patient with a tear of the ligamentum teres may develop hip microinstability which, when combined with recreational and sports activities, may result in damage to the labrum and cartilage.39 In addition, the ligamentum teres forms a sling-like structure that supports the femoral head inferiorly as the hip goes into flexion and abduction (i.e., squat).9 Finally, Gray and Villar40 have proposed that the ligamentum teres has a windshield wiper effect in distributing synovial fluid within the hip joint. The ligament tightens during adduction, flexion, and external rotation, and it can become injured during subluxation.41
The Acetabular Labrum
The acetabular labrum (Fig. 19-3) is a semicircular ring consisting of fibrocartilage and dense connective tissue42 that encases the femoral head and is attached to the acetabular margin. The labrum, which varies greatly in form and thickness, has a triangular cross section: an internal articular surface, an external surface contacting the joint capsule, and a basal surface attached to the acetabular bone and transverse ligaments.43 Most of the labrum is composed of thick, type I collagen fiber bundles principally arranged parallel to the acetabular rim, with some fibers scattered throughout this layer running obliquely to the predominant fiber orientation.44 The normal microvasculature of the acetabular labrum consists of a group of small vessels located in the substance of the labrum traveling circumferentially around the labrum at its attachment site on the outer surface of the bony acetabular extension.45 In addition, the labrum is surrounded by highly vascularized synovium that is present in the capsular recess.45 The central portion is contiguous with the cartilaginous surface of the acetabulum, and the periphery is continuous with the hip capsule.33 The majority of the acetabular labrum on the articular side was thought to be avascular. However, cadaver studies have shown it to contain sensory and vascular innervations with the blood vessels entering primarily the peripheral part of the labrum, and with penetration only into the outer one-third of the substance of the labrum.42 Nerve endings and sensory end organs in the superficial layers of the labrum participate in nociceptive and proprioceptive mechanisms.46,47 The acetabular labrum of the hip, to a large extent, is analogous to the meniscus of the knee (see Chapter 20) and the labrum of the glenohumeral joint (see Chapter 16) in that it enhances joint stability by deepening the socket, and decreasing the forces transmitted to the articular cartilage.46,47 The osseous acetabulum in the hip provides substantial static stability to the hip joint.48 Deepening of the socket that is provided by the labrum would, therefore, appear to be less important at the hip. Past research does indicate, however, that the labrum may enhance stability by providing negative intra-articular pressure in the hip joint so that it serves as a suction-seal mechanism.49
In addition, the labrum functions as a force distributor and shock absorber.33 Another proposed function of the labrum is to improve the mobility of the hip by providing an elastic alternative to the bony rim.20
Muscles
The hip joint is surrounded by a wide variety of muscles that accelerate, decelerate, and stabilize the hip joint by providing dynamic and passive resistance to external forces that may contribute to excessive motion. Indeed 21 muscles cross the hip, providing both triplanar movement and stability between the femur and the acetabulum.50 Consequently, abnormal performance of the muscles of the hip may alter the distribution of forces across the joint articular surfaces, potentially causing, or at least predisposing, degenerative changes in the articular cartilage, bone, and surrounding connective tissues.50 The origin, insertion, and innervation of these muscles are outlined in Table 19-3. Since the hip joint is able to move through a wide range of motion (ROM), a muscle’s line of pull may be altered with changing hip position, which makes describing a muscle’s action difficult. For example, the orientation of the gluteus medius allows it to work as an internal rotator in hip flexion yet as a weak external rotator in hip extension.51 Similarly, the tensor fascia latae (TFL) is a hip abductor and flexor, depending upon the hip position, while being a weak internal rotator in all positions.52 The hip muscles and their respective actions are outlined in Tables 19-3 and 19-4.
TABLE 19-3 | Origin, Insertion, and Innervation of Muscles Acting Across the Hip Joint |
Muscle | Origin | Insertion | Innervation |
Adductor brevis | External aspect of the body and inferior ramus of the pubis | The line from the greater trochanter of the linea aspera of the femur | Obturator nerve |
Adductor longus | In angle between pubic crest and symphysis | The middle third of the linea aspera of the femur | Obturator nerve |
Adductor magnus | Inferior ramus of pubis, ramus of ischium, and the inferolateral aspect of the ischial tuberosity | To the linea aspera and adductor tubercle of the femur | Obturator nerve and tibial portion of the sciatic nerve |
Biceps femoris | Long head arises from the sacrotuberous ligament and posterior aspect of the ischial tuberosity. Short head does not act across the hip | On the lateral aspect of the head of the fibula, the lateral condyle of the tibial tuberosity, the lateral collateral ligament, and the deep fascia of the leg | Tibial portion of the sciatic nerve, S1 |
Gemelli (superior and inferior) | Superior-posterior (dorsal) surface of the spine of the ischium and inferior-upper part of the tuberosity of the ischium | Superior- and inferior-medial surface of the greater trochanter | Sacral plexus |
Gluteus maximus | Posterior gluteal line of the ilium, iliac crest, aponeurosis of the erector spinae, posterior (dorsal) surface of the lower part of the sacrum, side of the coccyx, sacrotuberous ligament, and intermuscular fascia | Iliotibial tract of the fascia latae and gluteal tuberosity of the femur | Inferior gluteal nerve |
Gluteus medius | Outer surface of the ilium between the iliac crest and the posterior gluteal line, anterior gluteal line, and fascia | Lateral surface of the greater trochanter | Superior gluteal nerve |
Gluteus minimus | Outer surface of the ilium between the anterior and inferior gluteal lines, and the margin of the greater sciatic notch | On the anterior surface of the greater trochanter | Superior gluteal nerve |
Gracilis | The body and inferior ramus of the pubis | The superior medial surface of the proximal tibia, just proximal to the tendon of the semitendinosus | Obturator nerve |
Iliacus | Superior two-thirds of the iliac fossa and upper surface of the lateral part of the sacrum | Fibers converge with tendon of the psoas major to lesser trochanter | Femoral nerve |
Obturator externus | Rami of the pubis, ramus of the ischium, and medial two-thirds of the outer surface of the obturator membrane | Trochanteric fossa of the femur | Obturator nerve |
Obturator internus | Internal surface of the anterolateral wall of the pelvis and obturator membrane | Medial surface of the greater trochanter | Sacral plexus |
Pectineus | Pectineal line | Along a line extending from the lesser trochanter to the linea aspera | Femoral or obturator or accessory obturator nerves |
Piriformis | Pelvic surface of the sacrum, gluteal surface of the ilium, capsule of the sacroiliac joint, and sacrotuberous ligament | Upper border of the greater trochanter of femur | Sacral plexus |
Psoas major | Transverse processes of all the lumbar vertebrae bodies and intervertebral disks of the lumbar vertebrae | Lesser trochanter of the femur | Lumbar plexus |
Quadratus femoris | Ischial body next to the ischial tuberosity | Quadrate tubercle on femur | Nerve to quadratus femoris |
Rectus femoris | By two heads, from the anterior-inferior iliac spine, and a reflected head from the groove above the acetabulum | Upper border of the patella | Femoral nerve |
Sartorius | Anterior-superior iliac spine and notch below it | Upper part of the medial surface of the tibia in front of the gracilis | Femoral nerve |
Semimembranosus | Ischial tuberosity | The posterior-medial aspect of the medial condyle of the tibia | Tibial nerve |
Semitendinosus | Ischial tuberosity | Upper part of the medial surface of the tibia behind the attachment of the sartonus and below that of the gracilis | Tibial nerve |
Tensor fascia latae | Anterior part of outer lip of the iliac crest and the lateral surface of the anterior-superior iliac spine | Iliotibial tract | Superior gluteal nerve |
TABLE 19-4 | Hip Actions and Muscles If in Anatomic Position | ||
Hip Action | Prime Movers | Assistant Movers |
Flexors | Iliopsoas Sartorius Tensor fascia latae Rectus femoris Pectineus Adductor longus | Adductor brevis Gracilis Gluteus minimus (anterior fibers) |
Extensors | Gluteus maximus Semitendinosus Semimembranosus Biceps femoris (long head) Adductor Magnus (posterior head) | Gluteus medius (middle and posterior fibers) Adductor magnus (anterior head) |
Abductors | Gluteus medius (all fibers) Gluteus minimus (all fibers) Tensor fascia latae | Sartorius Rectus femoris Piriformis |
Adductors | Adductor magnus (anterior and posterior heads) Adductor longus Adductor brevis Gracilis Pectineus | Biceps femoris (long head) Gluteus maximus (posterior fibers) Quadratus lumborum Obturator externus |
External rotators | Gluteus maximus Gemellus inferior Gemellus superior Obturator internus Quadratus femoris Piriformis (at less than 60 degrees hip flexion) | Gluteus medius (posterior fibers) Gluteus minimus (posterior fibers Biceps femoris (long head) Sartorius Obturator externus |
Internal rotators | No specific muscle | Semitendinosus Semimembranosus Gracilis Piriformis (at 90 degrees hip flexion) Gluteus medius (anterior fibers) Adductor longus Adductor brevis Pectineus Adductor Magnus (posterior head) Gluteus minimus (anterior fibers) Tensor fascia latae |
Data from Anderson LC. The anatomy and biomechanics of the hip joint. J Back Musculoskeletal Rehabil. 1994;4:145–153; Neumann DA. Kinesiology of the hip: a focus on muscular actions. J Orthop Sports Phys Ther. 2010;40:82–94. | ||
Iliopsoas
The iliopsoas muscle, formed by the iliacus and psoas major muscles (Fig. 19-4), is the most powerful hip flexor while also functioning as a weak adductor and external rotator of the hip. The iliopsoas attaches to the hip joint capsule, thereby giving it some support anteriorly. Since the muscle spans both the axial and appendicular components of the skeleton, it also functions as a trunk flexor, and affords an important element of the vertical stability of the lumbar spine, especially when the hip is in full extension, and passive tension is greatest in the muscle.50,54 Functionally, the hip flexors assist with foot clearance during level ambulation and stair negotiation. Theoretically, a sufficiently strong and isolated bilateral contraction of any hip flexor muscle will either rotate the femur toward the pelvis, the pelvis (and possibly the trunk) toward the femur, or both actions simultaneously.50 Intermuscular cooperation between the iliopsoas group and the rectus abdominis to prevent an anterior tilt and reinforce a neutral pelvis is fundamental to creating a stable proximal platform of the lumbopelvic region for effective therapeutic exercise.50
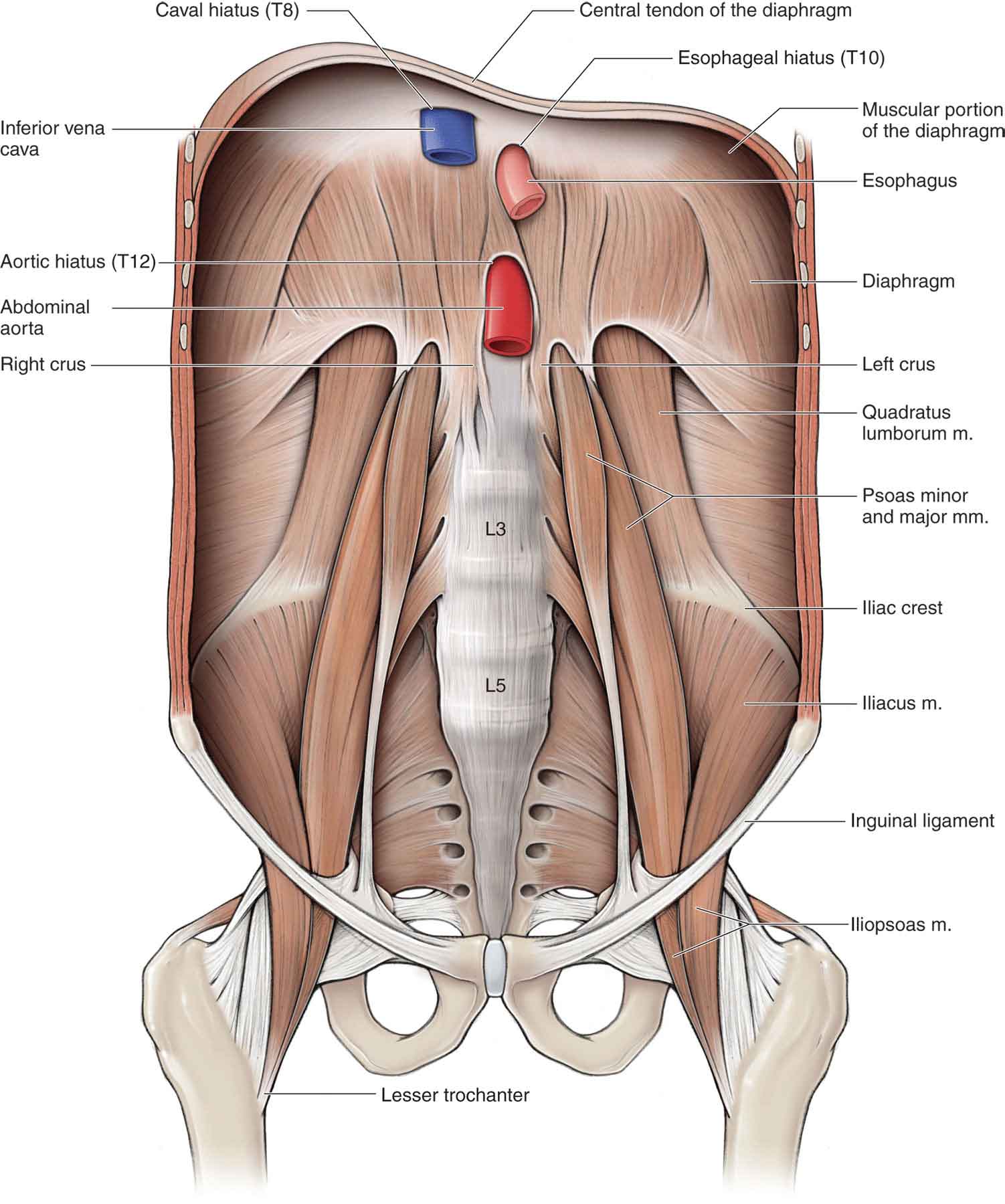
FIGURE 19-4 Muscles of the anterior hip. (Reproduced, with permission, from Chapter 11. Posterior Abdominal Wall. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
Iliocapsularis
The iliocapsularis muscle is a lesser-known structure that originates from the anterior medial hip capsule and inserts just distal to the lesser trochanter so that it overlies the anterior hip capsule. Its function is to help stabilize and tighten the anterior hip capsule.55 The iliocapsularis muscle has been found to be significantly hypertrophied in dysplastic hips versus normal hips.56
Tensor Fascia Latae
The TFL arises from the anterior aspect of the outer lip of the iliac crest and the lateral surface of the ASIS, and part of the lateral border of the notch below it (Fig. 19-5). As it passes inferiorly, the TFL envelops the muscles of the thigh. The trochanteric bursa is found deep to this muscle, as it passes over the greater trochanter (see later).57 The TFL, which flexes, abducts, and externally rotates the hip, also serves to counteract the backward pull of the gluteus maximus on the iliotibial band (ITB). The attachment of the TFL via the ITB to the anterolateral tibia provides a flexion moment in knee flexion and an extension moment in knee extension. The anteromedial fibers of the TFL have been shown to be increasingly active during jogging, running, and sprinting.9 This is theorized to be because of its role in assisting decelerating hip extension and accelerating hip flexion.58
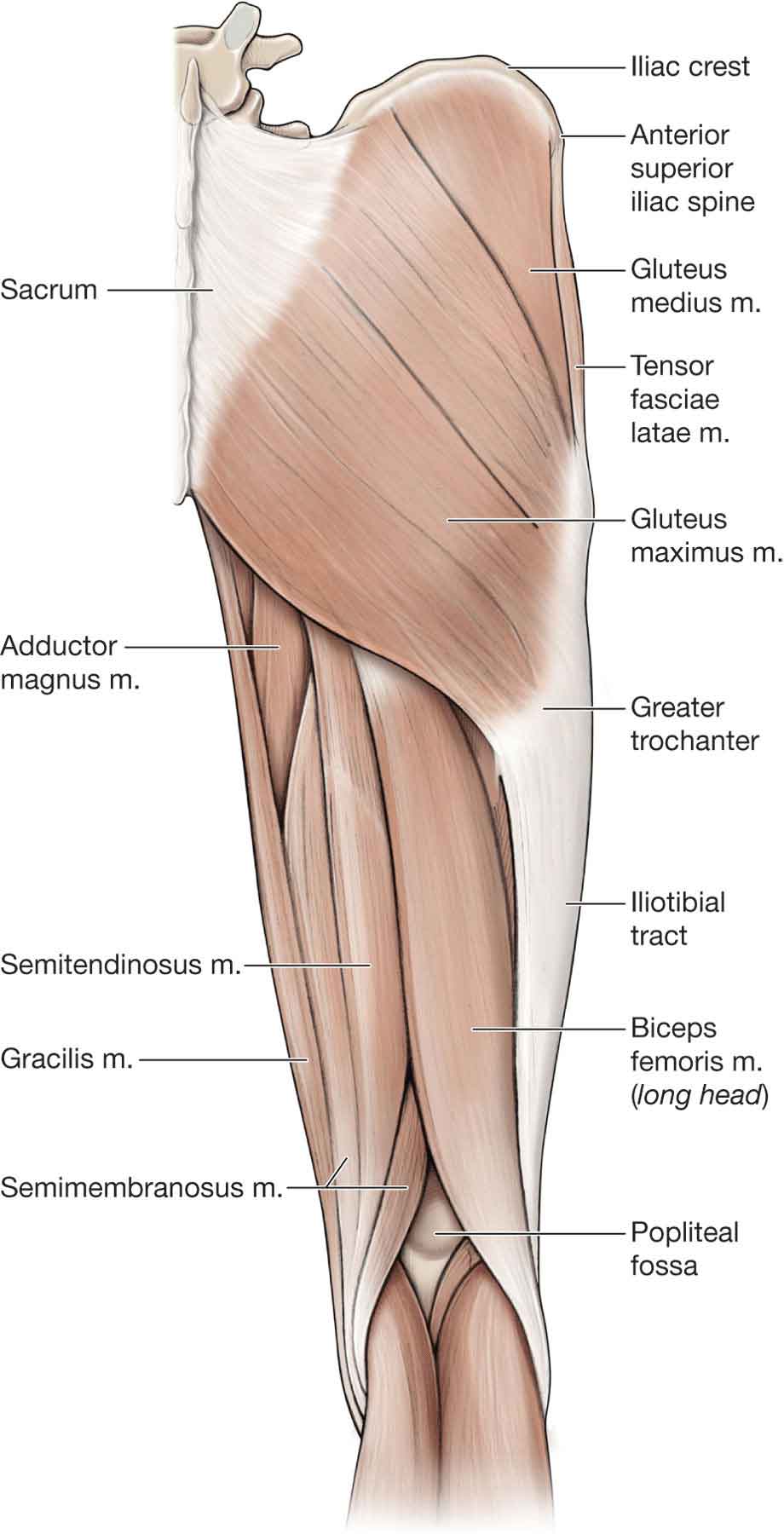
FIGURE 19-5 Superficial muscles of the posterior hip. (Reproduced, with permission, from Chapter 35. Gluteal Region and Hip. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
Gluteus Maximus
The gluteus maximus (Fig. 19-5) is the largest and most powerful hip extensor. It is also an important external rotator of the hip when the hip is in an anatomic neutral position.50 The larger, superficial portion of this muscle inserts into the proximal part of the ITB, while the deep portion inserts into the gluteal tuberosity of the femur. The inferior gluteal nerve, which innervates the muscle, is located on the deep portion.
The gluteus maximus50 is normally active only when the hip is in flexion, as during walking up an incline, stair climbing or cycling, or when extension of the hip is resisted.60 The superior portion of the gluteus maximus acts as a hip abductor during gait.61 Fibrous attachments over the sacroiliac joint from the gluteus maximus assist in trunk extension, control of lateral sway, and contributes to bipedal locomotion.59 The hip extensors as a group create the greatest amount of torque across the hip joint.9
Gluteus Medius
Because of its shape and functional similarities, the gluteus medius is known as the deltoid of the hip and, like the deltoid muscle at the shoulder, the gluteus medius can be divided into three functional parts: an anterior portion, a middle portion, and a posterior portion, each of which are innervated by separate branches of the superior gluteal nerve.9 The anterior portion, the fibers of which are oriented the most vertical, works to flex, and internally rotate the hip. The middle portion, the fibers of which are slightly obliquely oriented, abducts the hip. The posterior portion, the fibers of which are oriented almost parallel to the femoral neck, extends and externally rotates the hip while also stabilizing the femoral head in the acetabulum.9 On the deep surface of this muscle is located the superior gluteal nerve and the superior and inferior gluteal vessels.
The gluteus medius (Fig. 19-5) is the primary source of dynamic stabilization of the hip joint in the frontal plane, making it critical for balancing the pelvis during single-limb stance, which accounts for approximately 60% of the gait cycle (see Chapter 6).62 During single-limb stance, approximately three times the body weight is transmitted to the hip joint with two-thirds of that being generated by the hip abductor mechanism.62 In addition to its role as a stabilizer, the gluteus medius also functions as a decelerator of hip adduction.
Gluteus Minimus
The gluteus minimus (Fig. 19-6), the most major internal rotator of the femur, is a relatively thin muscle situated between the gluteus medius muscle and the external surface of the ilium. The gluteus minimus also abducts the thigh, as well as having a primary function as a joint stabilizer, creating compression through its attachment to the capsule.63 The ability to maintain joint centering to facilitate efficient joint mobility and decrease joint injury is an important function of this muscle in relation to pathological conditions related to joint instability, acetabular undercoverage, and congenital anomalies.59 It receives support from the TFL, semitendinosus, semimembranosus, and gluteus medius.60
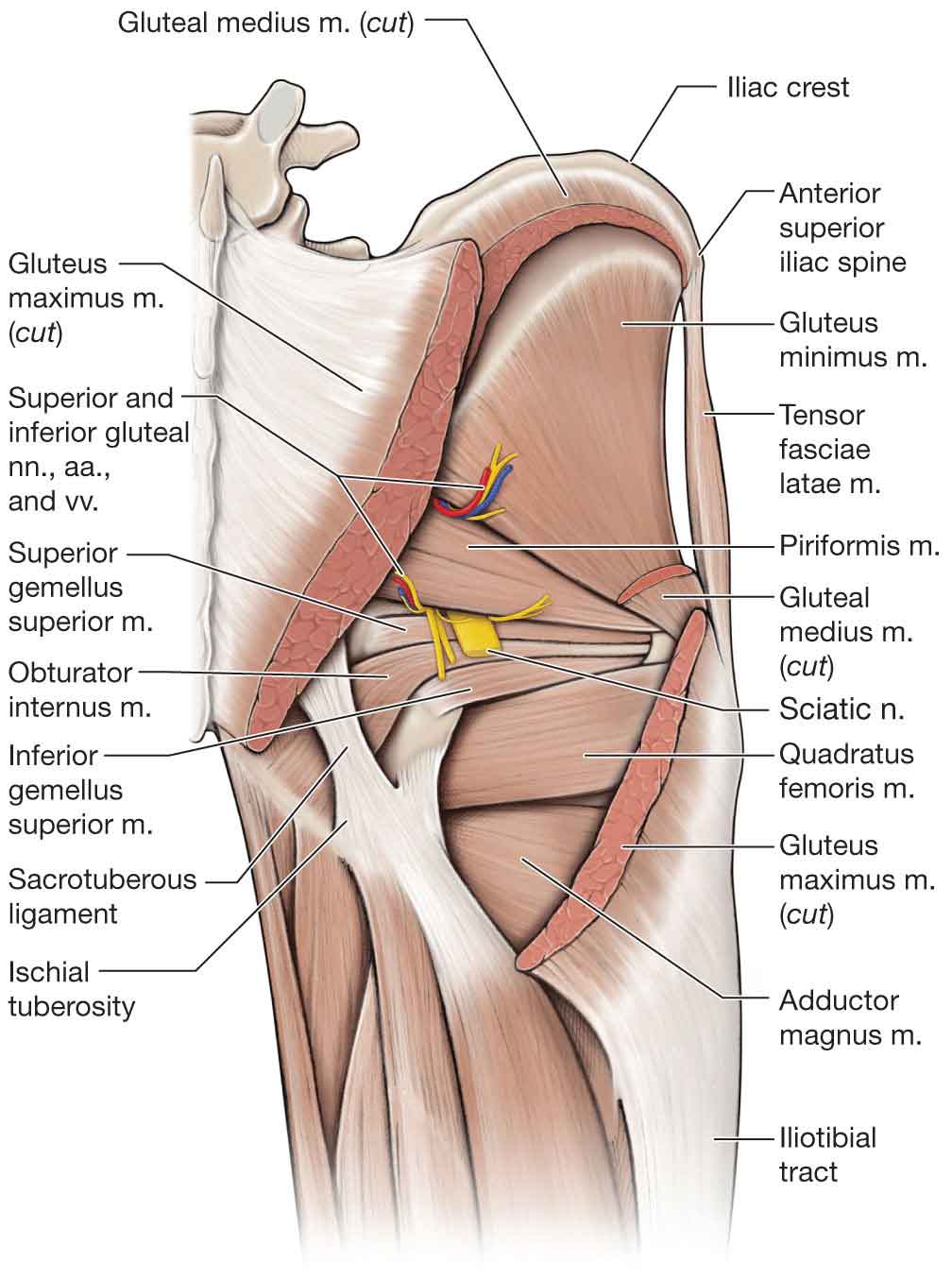
FIGURE 19-6 Deeper muscles of the posterior hip. (Reproduced, with permission, from Chapter 35. Gluteal Region and Hip. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
Piriformis
The piriformis (Fig. 19-6) is an external rotator of the hip at less than 60 degrees of hip flexion. At 90 degrees of hip flexion, the piriformis reverses its muscle action, becoming an internal rotator and abductor of the hip.64 Because of its close association with the sciatic nerve, the piriformis can be a common source of buttock and leg pain (see Chapter 5).65–68
Rectus Femoris
The rectus femoris muscle (Fig. 19-7), one of the four quadriceps muscles (see Chapter 20), is a two-joint muscle that arises from two tendons: one, the anterior or direct, from the AIIS; the other, the posterior or indirect, from a groove above the brim of the acetabulum. The rectus femoris, which is a powerful hip flexor, also contributes to extension of the knee. It functions more effectively as a hip flexor when the knee is flexed, as when a person kicks a ball.60 During athletic function, the rectus femoris prevents excessive hip extension during gait.69
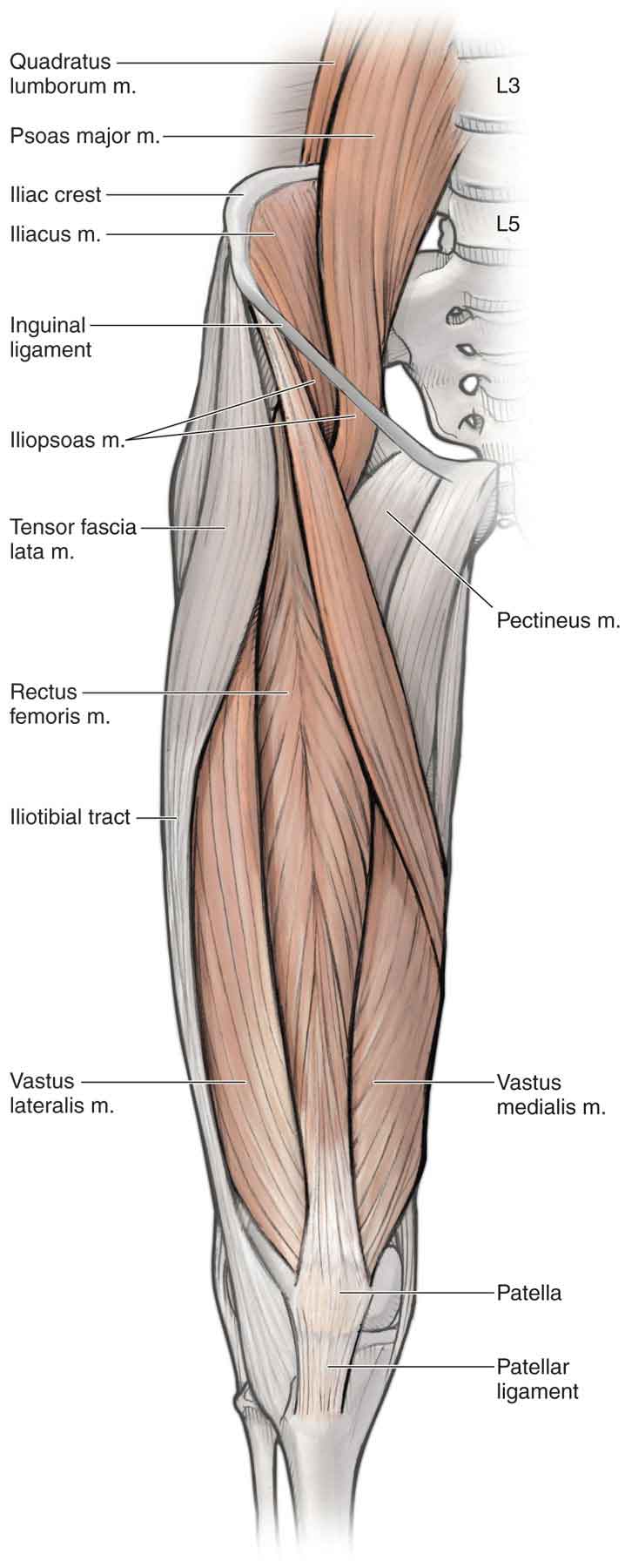
FIGURE 19-7 Muscles of the anterior hip and thigh. (Reproduced, with permission, from Chapter 36. Thigh. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
Obturator Internus
The obturator internus (Fig. 19-6) is normally an external rotator of the hip and an internal rotator of the ilium but becomes an abductor of the hip at 90 degrees of hip flexion.70
Obturator Externus
The obturator externus (Fig. 19-6), named for its location external to the pelvis, is an adductor and external rotator of the hip.17
Gemelli
The superior and inferior gemelli muscles (Fig. 19-6) are considered extensions of the obturator internus tendon. The superior gemellus is the smaller of the two. Both the gemelli function as minor external rotators of the hip.17
Quadratus Femoris
The quadratus femoris muscle (Fig. 19-6), another external rotator of the hip, is a flat, quadrilateral muscle, located between the inferior gemellus and the superior aspect of the adductor magnus. The quadratus femoris and the inferior gemellus share the same innervation (L4–L5).17 The obturator internus and superior gemellus also share the same innervation (L5–S1).17
Pectineus
The pectineus (Fig. 19-7) is an adductor, flexor, and internal rotator of the hip. Like the iliopsoas, the pectineus attaches to and supports the joint capsule of the hip.
Sartorius
The sartorius muscle (Fig. 19-7) is the longest muscle in the body. The sartorius is responsible for flexion, abduction, and external rotation of the hip, and some degree of knee flexion.75
Hamstrings
The hamstrings muscle group consists of the biceps femoris, the semimembranosus, and the semitendinosus.
Biceps Femoris. The biceps femoris (Fig. 19-8), which arises by way of a long and short head, extends the hip, flexes the knee, and externally rotates the tibia. Only the long head, which originates from the ischial tuberosity and lower part of the sacrotuberous ligament, acts on the hip. The short head arises from the lateral linea aspera, lateral supracondylar line, and intermuscular septum. The tibial portion of the sciatic nerve innervates the long head and the fibularis (peroneal) division innervates the short head. The long head is active during conditions that require lower amounts of force, such as decelerating the limb at the end of the swing phase and during forceful hip extension.76 The biceps femoris is the most commonly strained muscle of the hamstring complex (53%).77 The anatomy of the biceps femoris may help to explain its higher rate of injury. First, both the long and the short head have separate nerve supplies. This dual innervation may lead to asynchronous stimulation of the two heads—a mistimed contraction of the different parts of the muscle group may mean a reduced capacity to generate effective tension to control the imposed loads of the muscle.78 There may also be anatomical variations in the attachments of biceps femoris, which may predispose certain people to injury. Due to the origin of the long head of the biceps femoris, it could be argued that the biceps femoris has a triarticular function and is, therefore, more predisposed to injury than the other hamstring muscles.78 The insertion of the biceps femoris into the head of the fibula may also be a predisposing factor to injury—previous knee or ankle injury resulting in alteration in the movement of the superior tibiofibular joint may affect the biomechanics of the biceps femoris although this notion is speculative.78 However, incomplete knee excursion caused by meniscal damage may lead to excessive loading of the biceps femoris.79 In addition to the anatomical reasons, the biceps femoris is susceptible to high rates of injury as it is subjected to the greatest amount of eccentric load during high-speed activities such as sprinting.80 Given the rotational demands of many sports, this function may also predispose the biceps femoris to injury.
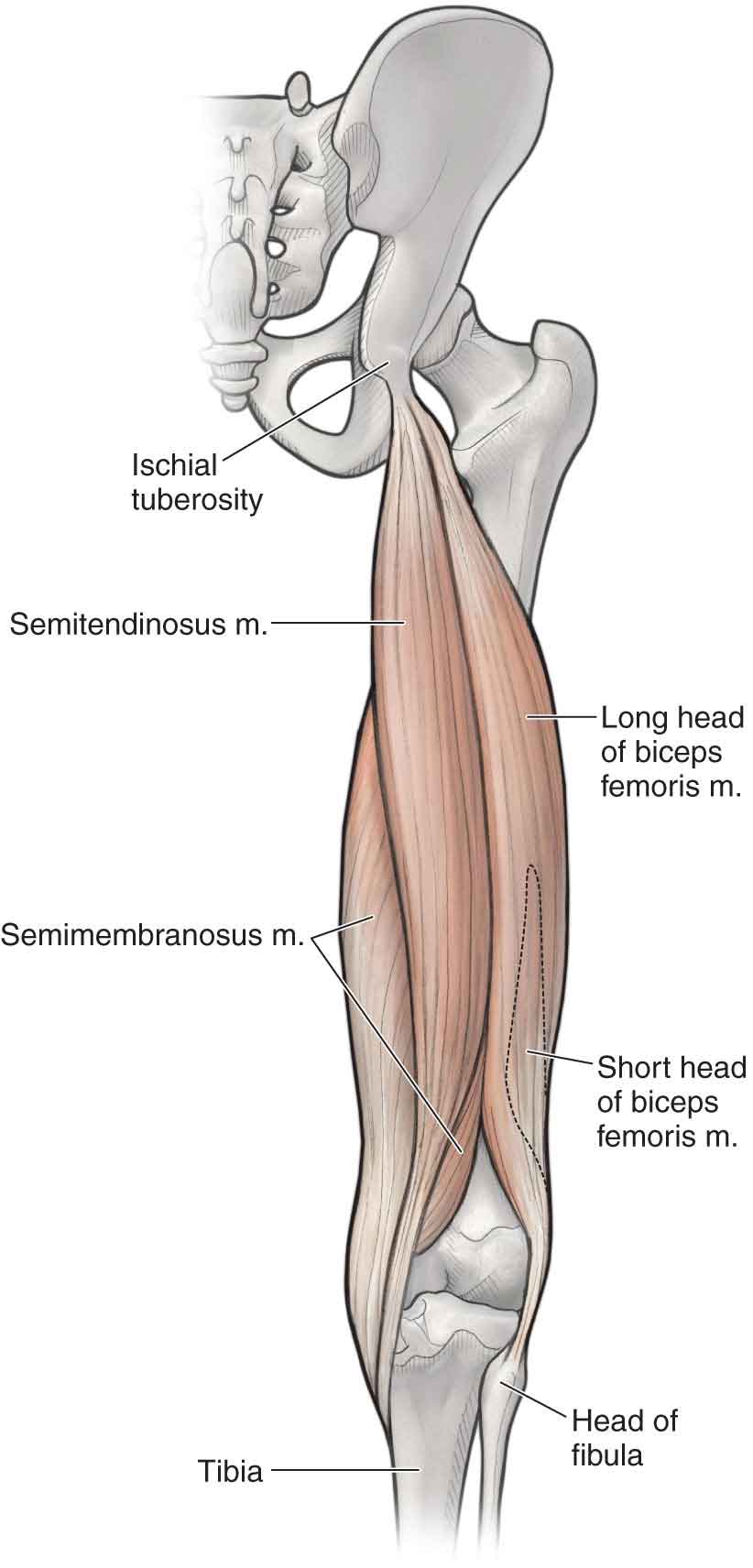
FIGURE 19-8 The hamstrings. (Reproduced, with permission, from Chapter 36. Thigh. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
Semimembranosus
The semimembranosus (Fig. 19-8) gains its name from its membranous origin at the ischial tuberosity beneath the semitendinosus and inserts onto the medial tibial condyle, posterior oblique ligament, arcuate ligament, and posterior joint capsule. The semimembranosus is innervated by the tibial division of the sciatic nerve.
Semitendinosus. The semitendinosus (Fig. 19-8) arises from the ischial tuberosity by a conjoint tendon with the biceps femoris and inserts as part of the pes anserinus on the superior and medial aspect of the tibia, and deep fascia of the leg at Gerdy’s tubercle. The semitendinosus is innervated by the tibial division of the sciatic nerve.
All three muscles of the hamstring complex (except for the short head of the biceps) work with the posterior adductor magnus and the gluteus maximus to extend the hip.84 The hamstrings also flex the knee and weakly adduct the hip. The long head of the biceps femoris helps with external rotation of the thigh and leg; the more medial semimembranosus and semitendinosus muscles assist with internal rotation of the thigh and leg.84 When the hamstrings contract, their forces are exerted on both the hip and knee joints simultaneously; functionally, however, they can actively mobilize only one of the two joints at any one time.84 During gait, prior to heel contact, the hamstrings decelerate knee extension and hip flexion to prepare for foot contact with the ground (see Chapter 6) and are active for the initial 10% of the stance phase to provide hip extension and stability to the knee through coactivation for dynamic stabilization.84 Compared to walking and jogging, running is a stressful activity for the hamstrings and increases the high demands on their tendon attachments, especially during eccentric contractions. While running, the hamstrings have three main functions84:
- They decelerate knee extension at the end of the forward swing phase. Consequently, hamstring injuries are most likely to occur during the terminal swing phase of running, while contracting eccentrically and while the muscle is in the more lengthened position.85 Through an eccentric contraction, the hamstrings decelerate the forward momentum (i.e., leg swing) at approximately 30 degrees short of full knee extension. The length–tension relationship and changing moment arm of the hamstrings decreases torque production near full knee extension when the hip joint is in 90-degree flexion as in the seated position.86
- At foot strike, the hamstrings elongate to facilitate hip extension through an eccentric contraction, thus further stabilizing the leg for weight bearing.
- The hamstrings assist the gastrocnemius in paradoxically extending the knee during the takeoff phase of the running cycle.
- At foot strike, the hamstrings elongate to facilitate hip extension through an eccentric contraction, thus further stabilizing the leg for weight bearing.
Hip Adductors
The adductors of the hip (Fig. 19-9) are found on the medial aspect of the joint.
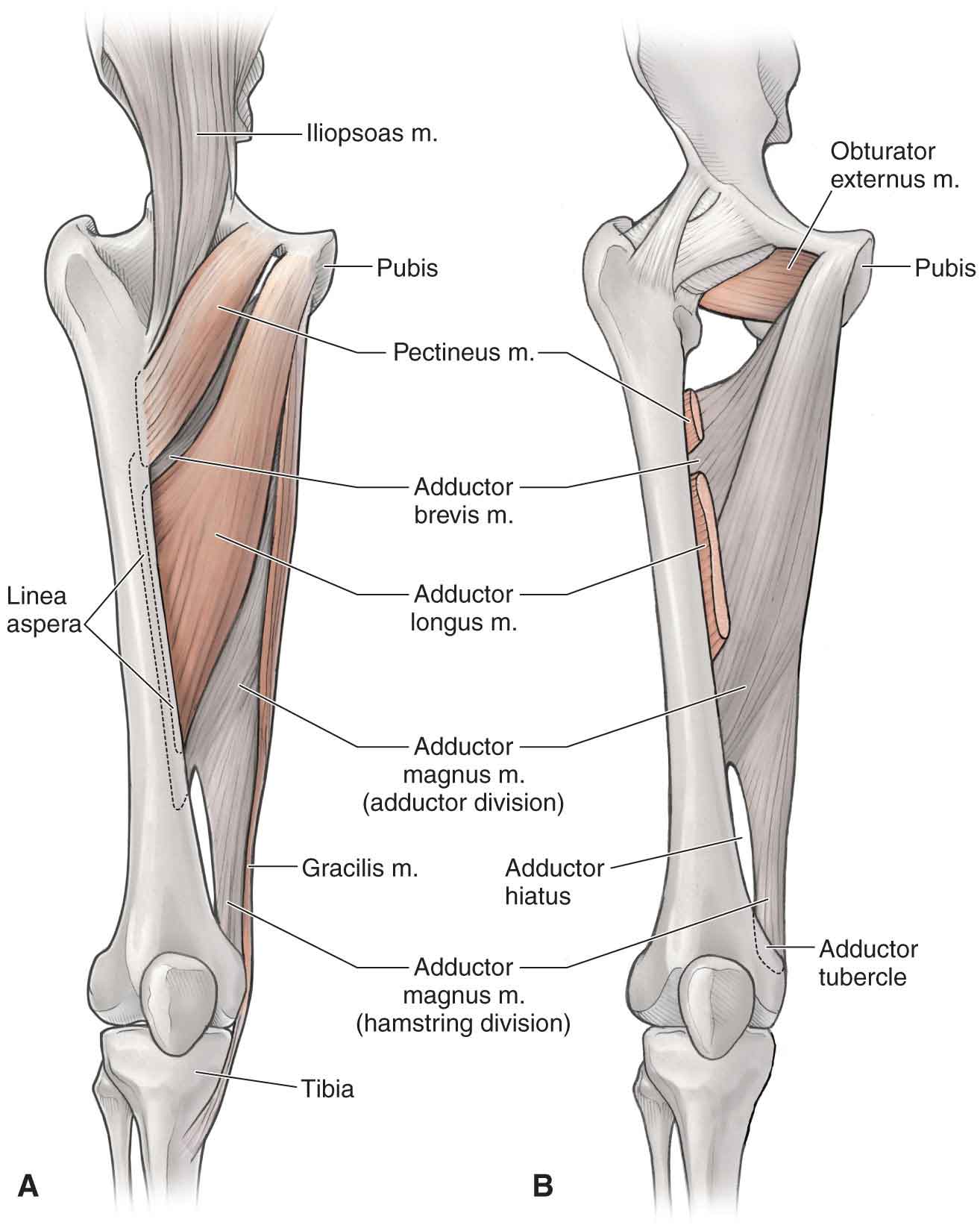
FIGURE 19-9 The hip adductors. (Reproduced, with permission, from Chapter 36. Thigh. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
Adductor Magnus. The adductor magnus is the most powerful adductor, and it is active to varying degrees in all hip motions except abduction. In addition, the adductor magnus has the greatest moment arm for hip extension. The posterior portion of the adductor magnus is sometimes considered functionally as a hamstring because of its anatomic alignment. Because of its size, the adductor magnus is less likely to be injured than the other hip adductors.87
Adductor Longus. The pectineus and adductor longus muscles serve as primary adductors of the hip while contributing to hip flexion. The adductor longus is the most prominent muscle of the adductors during resisted adduction and forms the medial border of the femoral triangle. The adductor longus also assists with external rotation, in extension, and internal rotation in other positions. The adductor longus is the most commonly strained adductor muscle due to its limited mechanical advantage.88,89 This mechanical disadvantage is due to the large distance from the axis of rotation to the center of mass of the lower extremity, resulting in the requirement of a greater force production to achieve the intended movement.59
Gracilis. The gracilis (Fig. 19-9), the longest of the hip adductors, is also the most superficial and medial of the hip adductor muscles. The gracilis functions to adduct and flex the thigh and flex and internally rotate the leg.
The other adductors of the hip include the adductor brevis, obturator externus, and the pectineus muscles. The main action of this muscle group is to adduct the thigh in the open kinetic chain and stabilize the lower extremity to perturbation in the closed kinetic chain. Each individual muscle can also provide assistance in femoral flexion and rotation.90
Bursa
There are more than a dozen bursae in this region.91 The more clinically significant ones are described below.
Iliopsoas Bursa
Many names have been used to describe the iliopsoas bursa (IPB), including the iliopsoas, iliopectineal, iliac, iliofemoral, and subpsoas bursa.92 The IPB is the largest and most constant bursa about the hip, present in 98% of normal adult individuals, usually bilaterally.93 The IPB is situated deep to the iliopsoas tendon and serves to cushion the tendon from the structures on the anterior aspect of the hip joint capsule. Its dimensions may be up to 7 cm in length and 4 cm in width.93 Anatomic boundaries of the bursa include the iliopsoas muscle anteriorly, the pectineal eminence and the hip joint capsule posteriorly, the iliofemoral ligament laterally, and the acetabular labrum medially.94
In 15% of patients, the IPB communicates with the hip joint via a 1-mm–3-cm point of relative capsular thinning between the iliofemoral and pubofemoral ligaments.21,92 While this connection may occur on a congenital basis,92 this number rises to 30–40% of patients with hip joint pathology.95
As with other bursae, the IPB can become inflamed and distended. Inflammation and distension of this bursa are most commonly associated with rheumatoid arthritis, but it is also seen in association with athletic activity, overuse and impingement syndromes, osteoarthrosis, pigmented villonodular synovitis, synovial chondromatosis, infection, pseudogout, metastatic bone disease, and, in rare cases, after Total Hip Arthroplasty (THA) (see “Intervention Strategies”).96
Trochanteric Bursa
Three bursae are consistently present at the greater trochanter, two major bursae, and one minor bursa. The two clinically significant trochanteric bursae are the subgluteus medius bursa, and the more superficial subgluteus maximus bursa.
 Subgluteus medius bursa: located at the superoposterior tip of the greater trochanter and functions to prevent friction between the gluteus medius muscle and the greater trochanter and also between the gluteus medius and gluteus minimus muscles.
Subgluteus medius bursa: located at the superoposterior tip of the greater trochanter and functions to prevent friction between the gluteus medius muscle and the greater trochanter and also between the gluteus medius and gluteus minimus muscles.
 Subgluteus maximus bursa: located between the greater trochanter and the fibers of the gluteus maximus and TFL muscles as they blend into the ITB.
Subgluteus maximus bursa: located between the greater trochanter and the fibers of the gluteus maximus and TFL muscles as they blend into the ITB.
Ischiogluteal Bursa
The ischiogluteal bursa is located between the ischium and the gluteus maximus muscle. It can be painfully squeezed between the ischial tuberosity and the hard surface of a chair while sitting, producing ischial bursitis. This condition is often referred to as weaver’s bottom.
Femoral Triangle
For topographic reasons, it is important to have an understanding of the anatomy of the femoral triangle. The femoral triangle is defined superiorly by the inguinal ligament, medially by the adductor longus, and laterally by the sartorius (Fig. 19-10). The floor of the triangle is formed by portions of the iliopsoas on the lateral side and by the pectineus on the medial side (Fig. 19-10). A number of neurovascular structures pass through this triangle. These include (from medial to lateral) the femoral vein, artery, and nerve (Fig. 19-10). Thus, the clinician should use caution when palpating in this area or applying soft tissue techniques.

FIGURE 19-10 The femoral triangle. (Reproduced, with permission, from Chapter 36. Thigh. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
Neurology
The hip joint is innervated primarily by L3 but also has contributions from L1–S1.9 In addition, many nerves have contributions to the hip, including the iliohypogastric, ilioinguinal, genitofemoral, lateral cutaneous nerve of the thigh, obturator, and femoral nerves.9 The posterior gluteal region receives cutaneous innervation by way of the subcostal nerve; the iliohypogastric nerve; the posterior (dorsal) rami of L1, L2, and L3; and the posterior (dorsal) primary rami (cluneal nerves) of S1, S2, and S3 (Figs. 19-11 and 19-12A).97
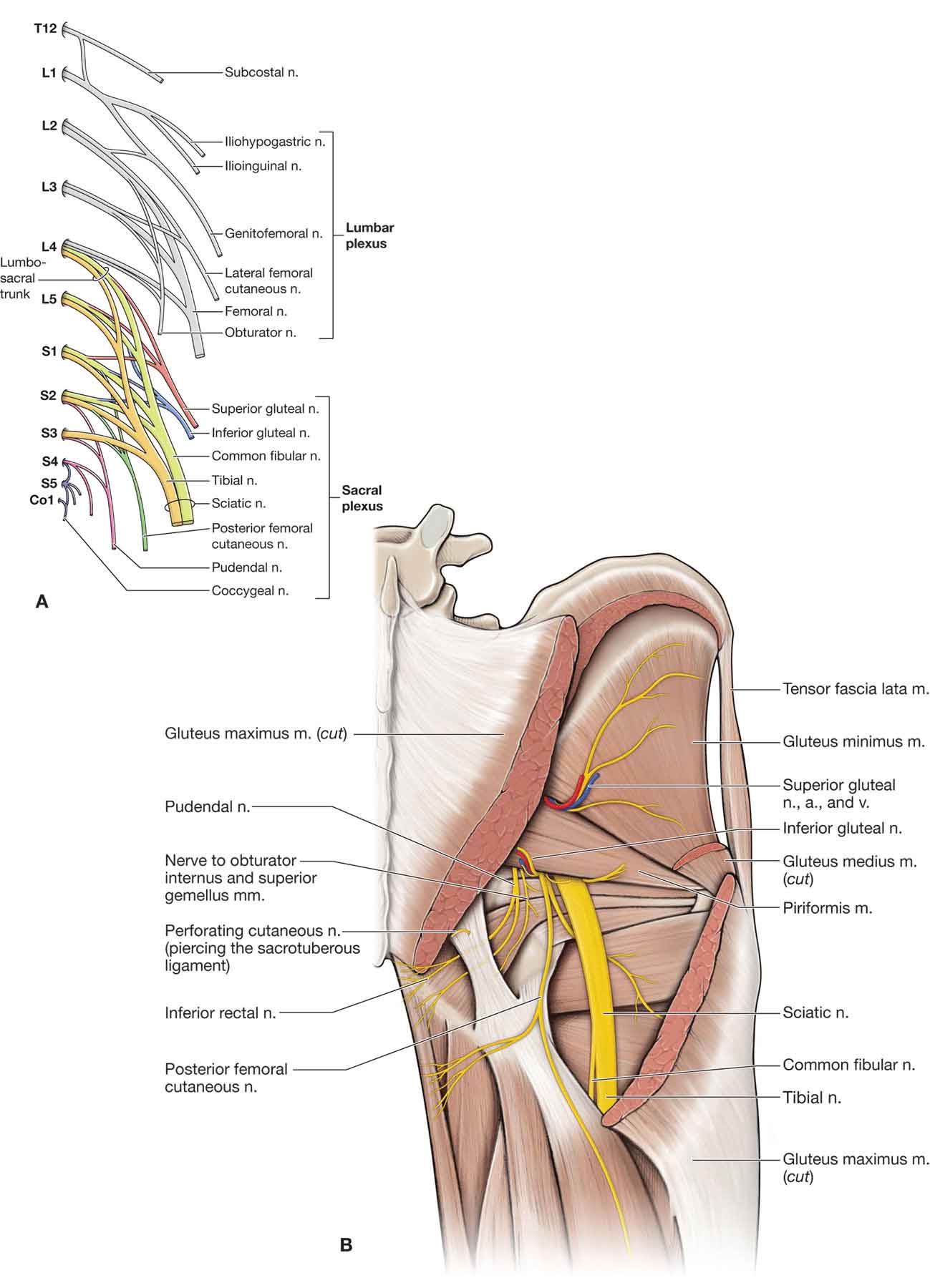
FIGURE 19-11 Neurology and vasculature of the posterior hip. (Reproduced, with permission, from Chapter 35. Gluteal Region and Hip. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
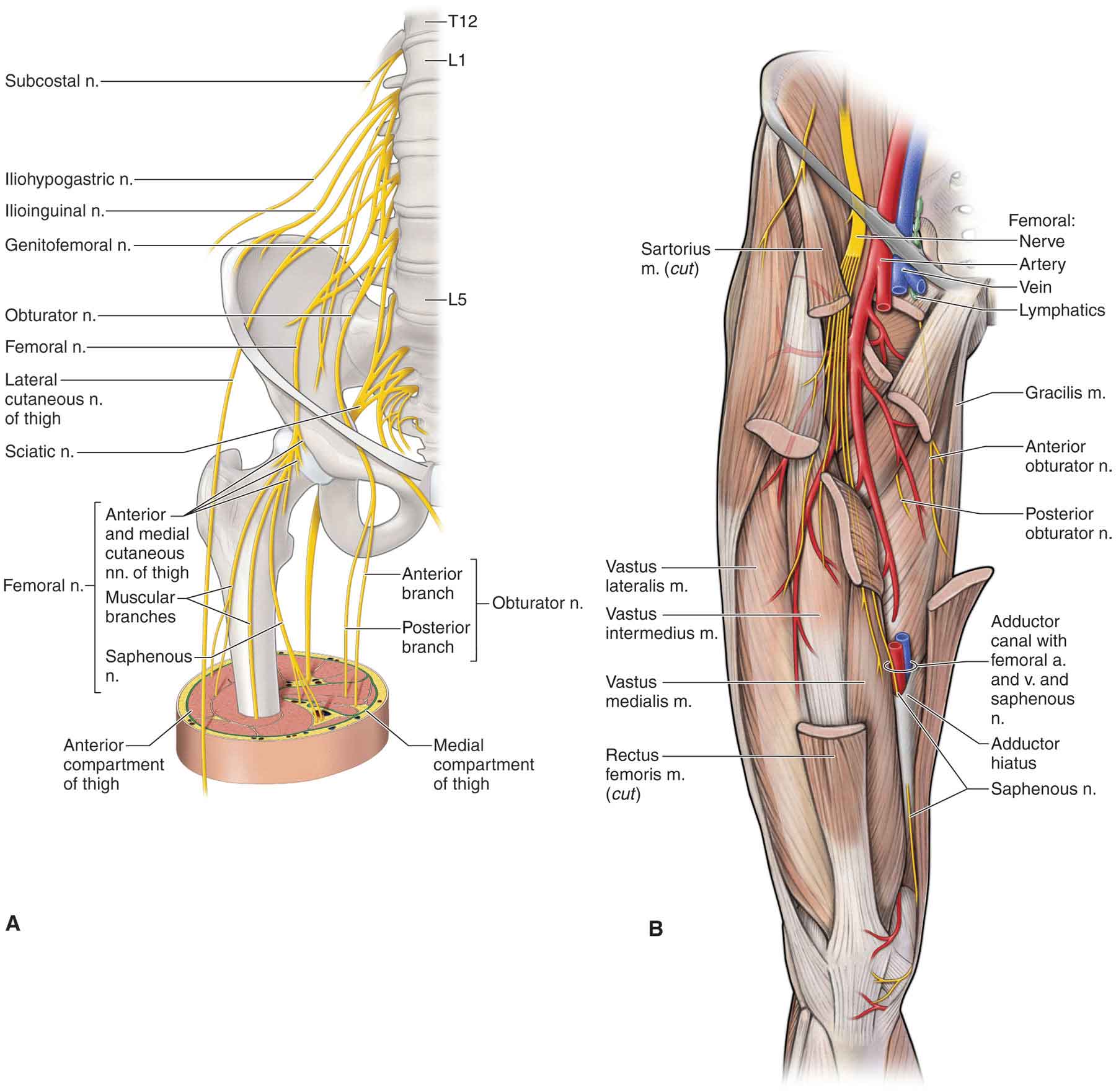
FIGURE 19-12 Neurology and vasculature of the anterior hip. (Reproduced, with permission, from Chapter 36. Thigh. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
The anterior region of the hip has its cutaneous supply divided by the inguinal ligament. The area superior to the ligament is supplied by the iliohypogastric nerve. The area inferior to the ligament is supplied by the subcostal nerve, the femoral branch of the genitofemoral nerve, and the ilioinguinal nerve (see Chapter 3).97
The nerves of the muscles that cross the hip joint (femoral, obturator, superior gluteal, and the nerve to the quadratus femoris) also supply the joint capsule and the joint. Therefore, pain referred from the hip joint may be felt anywhere in the thigh, leg, or foot.
Arthrogenic inhibition, defined as the reflex inhibition of the musculature surrounding the joint following effusion or injury, and which also occurs at the knee joint, is evident in the hip joint.98
Vascular Supply
The internal iliac artery becomes the femoral artery (Figs. 19-12B and 19-13), as it passes underneath the inguinal ligament. The femoral artery forms two branches. The anterior portion of the femoral neck and the anterior portion of the capsule of the hip joint are supplied by the lateral femoral circumflex artery. The medial femoral circumflex artery (MFCA) perforates and supplies the posterior hip joint capsule and the synovium.97 The deep branch of the MFCA gives rise to two to four superior retinacular vessels and, occasionally, inferior retinacular vessels.99,100
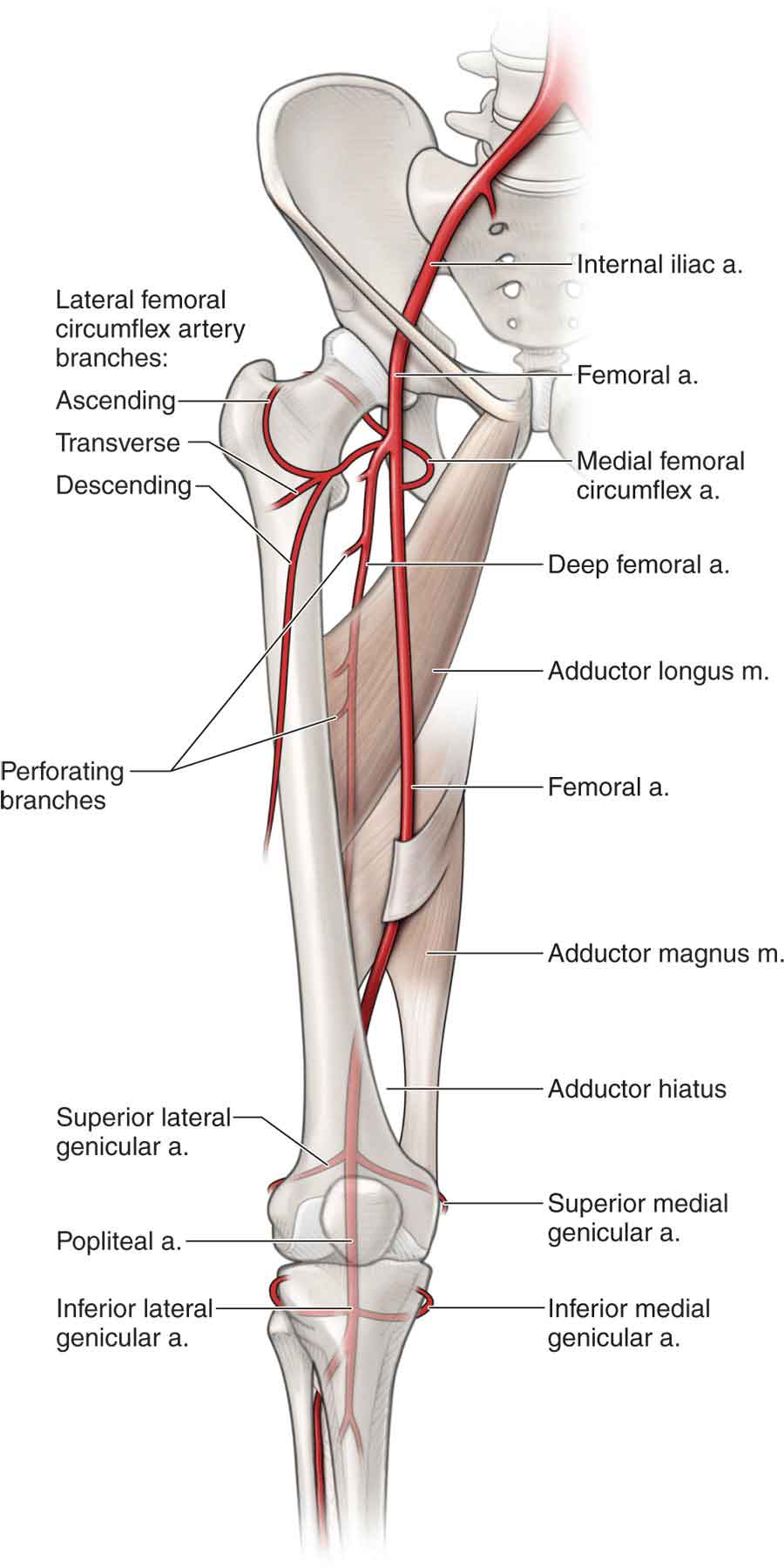
FIGURE 19-13 Vasculature of the hip and thigh. (Reproduced, with permission, from Chapter 36. Thigh. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
Most of the femoral head, comprising its upper one-half or upper two-thirds, is supplied by the obturator artery and a terminal branch of the MFCA (Fig. 19-3).32 The inferior epiphyseal artery, a branch of the lateral circumflex artery, contributes to the vascularization of the lower area of the femoral head. The supply to the femoral head from the ligamentum teres artery is extremely variable.101 The blood supply to the weight-bearing portion of the head of the femur is derived from the MFCA.102
Two other branches are formed from the internal iliac artery: the inferior and superior gluteal arteries. These arteries supply the superior portion of the capsule and the gluteus maximus muscle.
BIOMECHANICS
The hip joint has three degrees of freedom, which permits motion in three planes: sagittal (flexion and extension around a transverse axis), frontal (abduction and adduction around an anteroposterior axis), and transverse (internal and external rotation around a vertical axis) (Fig. 19-14). All three of these axes pass through the center of the femoral head. The normal motion of the hip joint is primarily rotational, and there is very little translation.103 Control of the hip during movement involves complex interactions between the nervous, muscular, and skeletal systems. Motion at the hip joint can occur through movement of the femur on the pelvis or from the motion of the pelvis on the femur (i.e., anterior or posterior pelvic tilt).
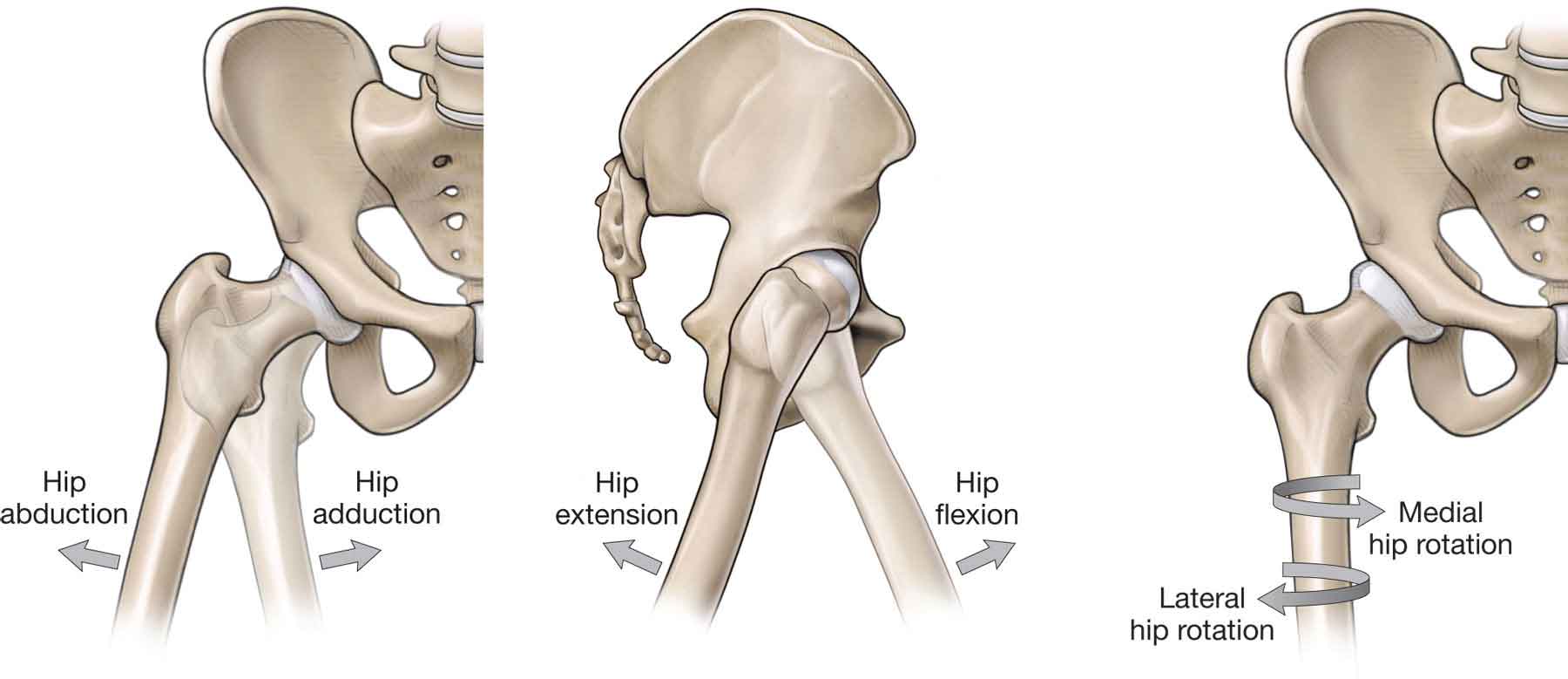
FIGURE 19-14 Movements of the hip. (Reproduced, with permission, from Chapter 35. Gluteal Region and Hip. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.)
The 27 muscles that cross the hip joint act as primary movers and dynamic stabilizers of the hip and lower extremity.104 These muscles provide a myriad of possibilities for compensation and pathology.9 For example, abnormal hip mechanics can result in gluteus medius tendinosis, hip flexor tendinitis, TFL strain, hamstring tendinosis, and ITB syndrome. Musculoskeletal disorders of the lower limbs are often associated with poor hip muscle performance and altered kinematics during dynamic weight-bearing tasks, such as running. For example, patellofemoral pain and Achilles pathology have both been linked to hip dysfunction.105
Active range of motion (AROM) of the hip is variable. Hip flexion averages 110–120 degrees, extension 10–15 degrees, abduction 30–50 degrees, and adduction 25–30 degrees. Hip external rotation averages 40–60 degrees and internal rotation averages 30–40 degrees (Table 19-5). Motions about the hip joint can occur independently; however, the extremes of motion require motion at the pelvis.106
TABLE 19-5 | Normal Ranges and End-Feels at the Hip | ||
Motion | Range of Motion (Degrees) | End-Feel |
Flexion | 110–120 | Tissue approximation or tissue stretch |
Extension | 10–15 | Tissue stretch |
Abduction | 30–50 | Tissue stretch |
Adduction | 25–30 | Tissue approximation or tissue stretch |
External rotation | 40–60 | Tissue stretch |
Internal rotation | 30–40 | Tissue stretch |
Data from Beattie P. The hip. In: Malone TR, McPoil T, Nitz A, eds. Orthopaedic and Sports Physical Therapy. 3rd ed. St. Louis, MO: CV Mosby; 1996:506. | ||
TABLE 19-6 | Hip Motion and Associated Innominate Motions |
Flexion (posterior rotation) Extension (anterior rotation) Abduction (upward) Adduction (downward) Internal rotation External rotation |
The hip joint is a marvel of physics, transmitting truly impressive loads, both tensile and compressive making it the fulcrum for all of the forces. Quantitative and qualitative analyses of the generation of compressive forces at the hip and the muscular mechanisms during weight bearing have been thoroughly documented.107–114 Depending on the length of the moment arm created by the abductor muscles, the added force of the hip abductors acting on the hip joint can increase the pressures translated across the joint. During ambulation, these compressive joint forces are further multiplied by ground reaction forces and inertial forces related to acceleration and deceleration of the lower limb. Because of muscle tension, compression on the hip is approximately the same as body weight during the swing phase.115 However, during the support phase, peak joint forces can range from 300% to 400% of body weight at normal walking speed, to 550% of body weight during fast walking and jogging, and as high as 870% of body weight during stumbling.60,116 Stair climbing and descending increase the loads on the hip by approximately 10% and 20%, respectively.60,117
When body weight is evenly distributed across both legs during upright standing, the forces acting on the hip joint are equivalent to half the partial weight made up of the trunk, head, and upper extremities.118 Were this partial body weight to represent 60% of total body mass, then each hip would be compressed by a force equal to 30% of the total body weight. In a single-limb support, however, shifts in the center of gravity away from the supporting limb dramatically change the equilibrium forces necessary to maintain balance and create a state of disequilibrium. This state of disequilibrium requires the generation of compensatory forces by the hip musculature, in order to maintain balance.
When pain accompanies degeneration of the hip joint articulation, the body compensates by attempting to reduce the forces generated on the articular surfaces. Since the contribution of body mass cannot be changed, the patient attempts to reduce joint pressures by shifting the upper trunk over the supporting limb during the stance phase. While this maneuver decreases the joint compression forces, the energy expended by laterally bending the trunk during stance significantly increases the energy cost of gait. For a patient with a painful hip, the use of a cane or crutch in the hand contralateral to the involved hip can be used to substantially reduce the excessive trunk motion and to decrease pressure on the hip joint.
The relationship between the proximal femur, the greater trochanter, and the overall femoral neck width is affected by muscle pull and the forces transmitted across the hip joint. In addition, normal joint nutrition, circulation, and muscle tone during development play an important role.3,119–121
In the anatomic position, the orientation of the femoral head causes the contact force between the femur and the acetabulum to be high in the anterosuperior region of the joint.122 Since the anterior aspect of the femoral head is somewhat exposed in this position; the joint has more flexibility in flexion than extension.123
The femoral neck is subjected to shearing and torsional strains because of its oblique orientation to the shaft of the femur.8 Downward forces act to displace the femoral head inferiorly and to bend the femoral neck downward. To counter these forces, the femoral neck has developed a unique system of obliquely oriented trabeculae that traverse the head and the neck.8 The angle between the femoral shaft and the neck is called the angle of inclination (Fig. 19-15) and is normally approximately 125 degrees (Fig. 19-15)64 although it can vary with body types. In a tall person, the angle of inclination is larger. The opposite is true with a shorter individual. The angle of inclination has an important influence on the hips. An increase in this angle causes the femoral head to be directed more superiorly in the acetabulum and is often referred to as coxa valga (Fig. 19-15). Coxa valga has the following effects at the hip joint:
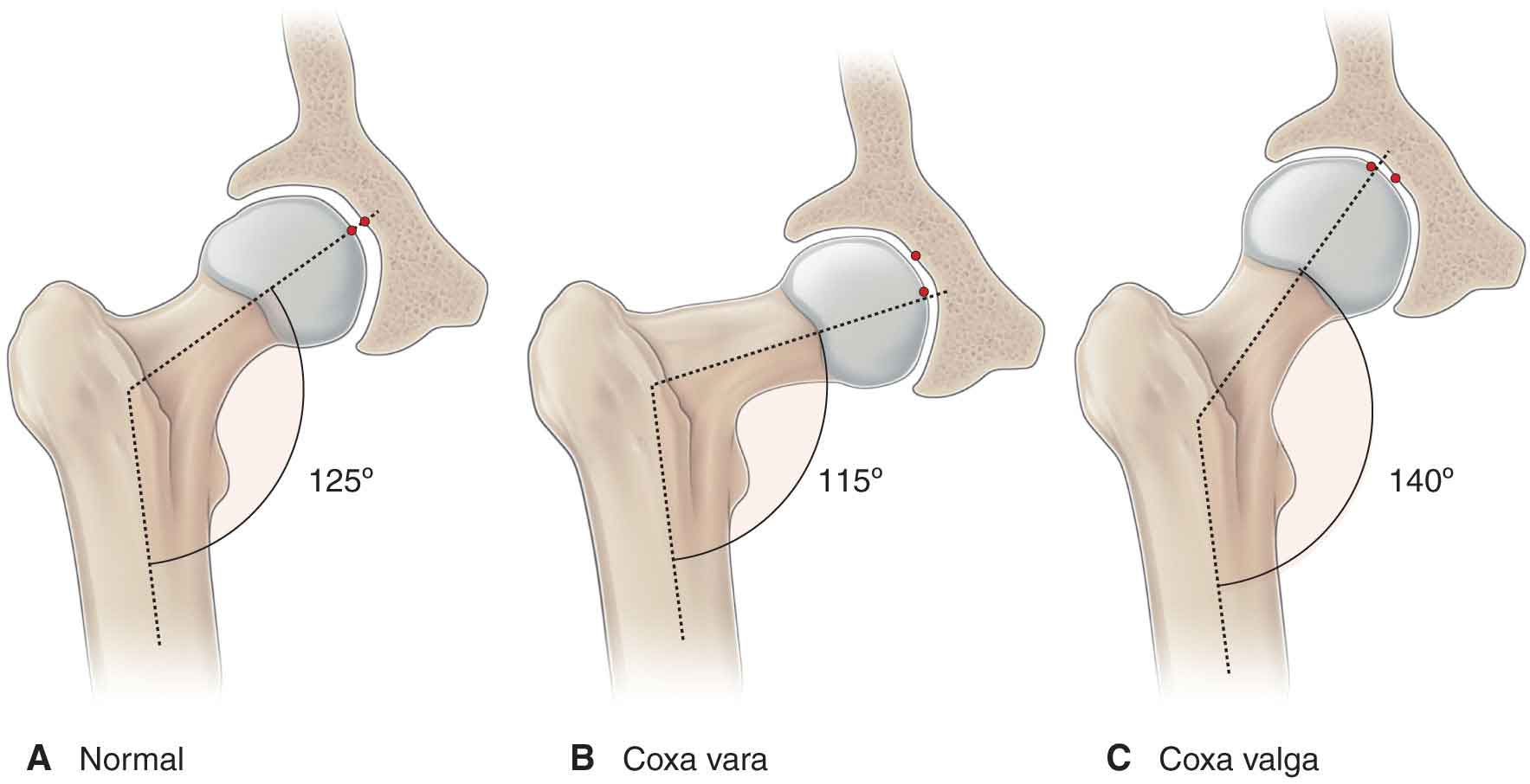
FIGURE 19-15 Angle of inclination and coxa vara/valga.
 It alters the orientation of the joint reaction force (JRF) from the normal vertical direction to one that is almost parallel to the femoral shaft.124,125 This lateral shift of the JRF reduces the available weight-bearing surface, resulting in an increase in stress applied across joint surfaces not specialized to sustain such loads.
It alters the orientation of the joint reaction force (JRF) from the normal vertical direction to one that is almost parallel to the femoral shaft.124,125 This lateral shift of the JRF reduces the available weight-bearing surface, resulting in an increase in stress applied across joint surfaces not specialized to sustain such loads.
 The moment arm of the hip abductors is shortened, placing these muscles in a position of mechanical disadvantage.125 This causes the abductors to contract more vigorously to stabilize the pelvis, producing an increase in the JRF.123
The moment arm of the hip abductors is shortened, placing these muscles in a position of mechanical disadvantage.125 This causes the abductors to contract more vigorously to stabilize the pelvis, producing an increase in the JRF.123
 It increases the overall length of the lower extremity, impacting other components in the kinetic chain. For example, coxa valga decreases the normal physiologic angle at the knee, which places an increased mechanical stress on the medial aspect of the knee joint and more tensile stress on the lateral aspect of the joint.
It increases the overall length of the lower extremity, impacting other components in the kinetic chain. For example, coxa valga decreases the normal physiologic angle at the knee, which places an increased mechanical stress on the medial aspect of the knee joint and more tensile stress on the lateral aspect of the joint.
If the angle of inclination is reduced, resulting in a more horizontal orientation of the femoral neck, it is referred to as coxa vara (Fig. 19-15). This position increases the downward shear forces on the femoral head and the tensile stretching forces through the superior trabecular bone along the lateral portion of the neck.8 In coxa vara, the joint compression forces are significantly reduced as the greater trochanter is displaced lateral and superior, which increases the effective angle of pull and the lever arm of the hip abductors.126 While the reduced compressive forces generated across the joint surfaces serve to decrease the incidence of articular cartilage damage, the increase in shearing and torsional forces at the femoral head/neck junction significantly increases the incidence of damage to the epiphyseal plate.8
Femoral alignment in the transverse plane also influences the mechanics of the hip joint. The torsion angle of the femur describes the relative rotation that exists between the shaft and the neck of the femur. An anterior orientation of the femoral neck to the transverse axis of the femoral condyles, is known as anteversion (Fig. 19-16), or a reverse orientation known as retroversion.25,123,127 Excessive anteversion directs the femoral head toward the anterior aspect of the acetabulum when the femoral condyles are aligned in their normal orientation. Subjects with excessive anteversion usually have more hip internal rotation ROM than external rotation, resulting in an in-toeing gait pattern, and a gravitation toward the typical “frog-sitting” posture as a position of comfort. Some studies have supported the hypothesis that a persistent increase in femoral anteversion predisposes to osteoarthritis (OA) of the hip,126,128–131 and knee,132–134 although other studies have refuted this.135–137 Nyland et al.138 demonstrated that those with increased femoral anteversion had significantly decreased peak electromyographic (EMG) amplitude of the vastus medialis and gluteus medius which they postulated might lead to an increased risk of knee injury due to a decrease in frontal and transverse plane stability.138 A cadaveric study by Sobczak et al.139 found that anteversion decreased the moment arm of the medial musculature including the gracilis and the semitendinosus, whereas retroversion increases the moment arm of the same muscles. Excessive retroversion of the femur will result in the opposite limitation: increased femoral external rotation ROM and decreased femoral internal rotation ROM.39 Retroversion is associated with an out-toeing gait pattern.
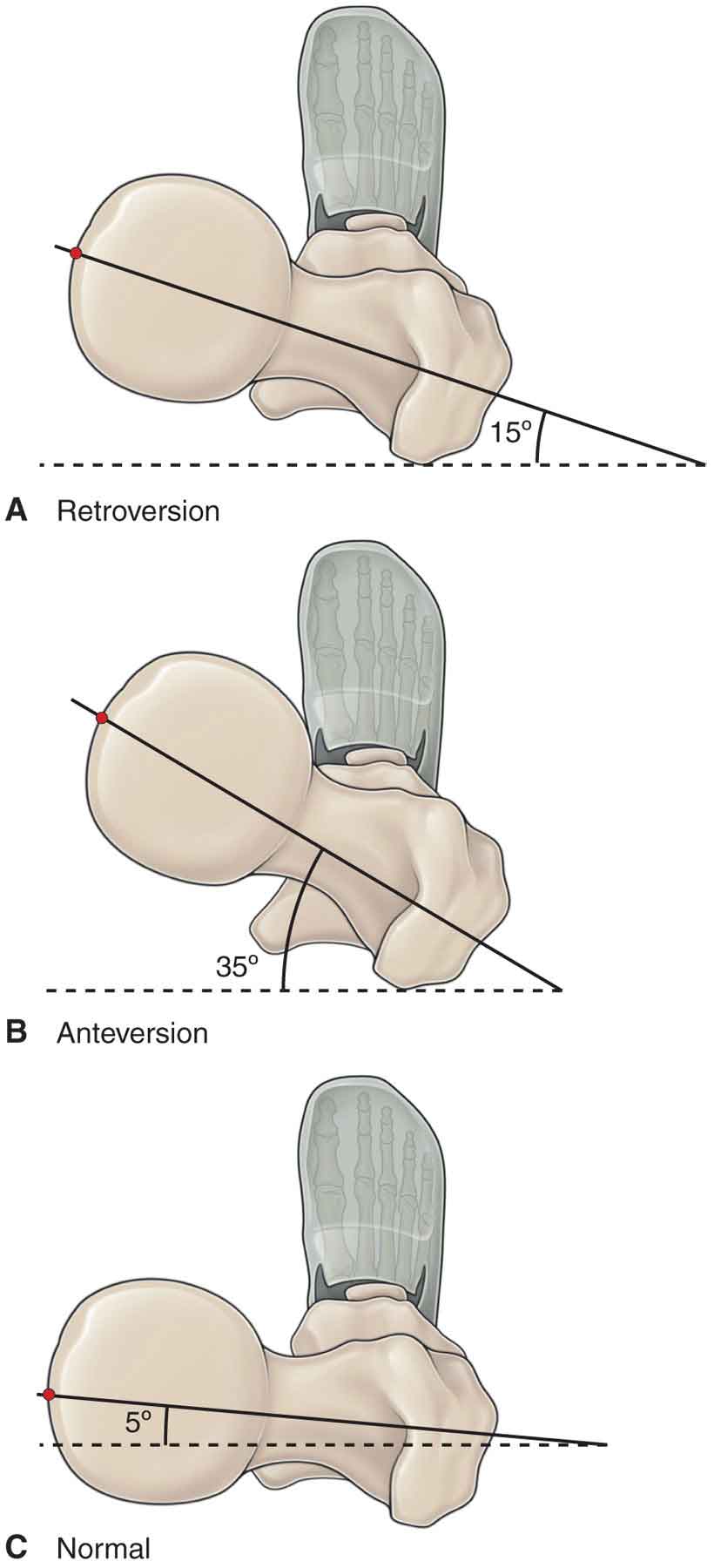
FIGURE 19-16 Angle of torsion: Anteversion and retroversion.
In contrast with most other joints in the body, the close-packed position for the hip is not the position of maximal articular congruency. The position of maximum articular congruence corresponds to a quadruped position: 90 degrees flexed, slightly abducted, and externally rotated. The most stable functional position of the hip is the normal standing position: hip extension, slight abduction, and slight internal rotation, which closely resembles the close-packed position of full extension, internal rotation, and abduction.17,114,140 The commonly cited open-packed (resting) positions of the hip are between 10 and 30 degrees of flexion, 10–30 degrees of abduction, and 0–5 degrees of external rotation.
