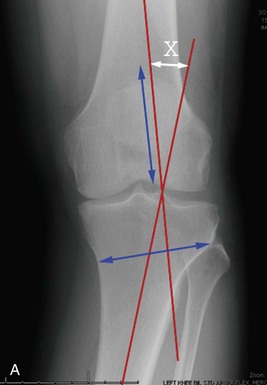
Chapter 70 1. The usual deformity is proximal tibia vara; therefore the osteotomy directly addresses the anatomic deformity. 2. Preservation of bone to the proximal tibia restores anatomy and potentially makes future arthroplasty procedures less technically challenging. 3. Disruption of the proximal tibiofibular joint and anterior compartment of the leg are prevented. 4. The peroneal nerve can be avoided. 5. Only one bone cut is required. 6. The correction can be modified intraoperatively. 7. It is relatively easy to combine the HTO with other procedures (e.g., ACL reconstruction, meniscal allograft). The disadvantages of the medial-sided procedure include the following: 1. Theoretically higher risk of nonunion as a result of the creation of a bony gap 2. Potential donor site morbidity if autograft is used or infectious disease transmission if allograft is used A number of potential methods can be used to calculate the size of the osteotomy.1–3 We currently employ the method described by Dugdale and colleagues,2 which corrects the weight-bearing axis to 62.5% of the width of the plateau, or 3 to 5 degrees of mechanical valgus. An example of the calculation can be seen in Figure 70-1. If there is excess varus malalignment because of soft tissue laxity, the difference in congruence angle on the affected and unaffected legs noted on the bilateral standing full-length AP radiograph is subtracted from the correction. Indications for an HTO include clinical and radiographic varus and (1) medial compartment arthrosis with or without mild to moderate asymptomatic radiographic patellofemoral arthrosis; (2) symptomatic ligamentous instability with medial compartment arthrosis; (3) recurrent ACL rupture with significant joint deformity; and (4) medial compartment pain in the setting of previous total medial meniscectomy, osteochondritis dissecans, or significant chondral damage.4 Isolated medial-sided degenerative joint disease with varus malalignment remains the most common indication for opening wedge HTO. The patient should be motivated and aware that pain relief may not be complete or permanent. Patients under the age of 50 and with a body mass index (BMI) of less than 25 are good candidates and demonstrate improved survivorship.5,6 An HTO in a patient with an unstable knee and malalignment may improve pain and instability symptoms and potentially delay the onset of cartilage degeneration.7,8 Absolute contraindications to HTO for medial compartment osteoarthritis include inflammatory arthritis and significant lateral tibiofemoral joint disease. Poorer outcomes after HTO have been correlated with severe articular destruction,9 significant patellofemoral disease,10 increased age,6,9,11 lateral tibial thrust,6 decreased range of motion,6 or joint instability.12 Recent literature presents evidence that ACL deficiency correlates with higher likelihood of long-term survival, suggesting that joint instability may not predict a poorer outcome.5 The preceding findings should be considered with each patient’s clinical picture, serve as a basis to counsel each patient on the potential for a good functional outcome, and should not be thought of as definitive reasons to avoid performing an osteotomy.
High Tibial Osteotomy
Preoperative Considerations
History
Imaging
Indications and Contraindications
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine