Head and Neck
16.1 Anatomy
William M. Falls
Gail A. Shafer-Crane
The skull is the skeleton of the head, which encloses the brain and its coverings as well as the 12 cranial nerves connected to the brain; houses the organs of special senses (sight, hearing, taste, and smell); and surrounds the openings into the digestive and respiratory tracts. The cervical spine, consisting of seven cervical vertebrae, furnishes stability and support for the head, permits motion of the head and neck, and provides protection and housing for the cervical spinal cord and nerve roots as well as the vertebral artery (Figs. 16.1.1 and 16.1.2). The cervical spine is convex anteriorly. Anatomy of the head and neck is presented in detail in major anatomic textbooks (1,2,3,4,5,6).
Several important bony and cartilaginous structures can be palpated as one examines the head and neck. Beginning anteriorly, the horseshoe-shaped hyoid bone can be palpated in the crease of the neck superior to the thyroid cartilage at the level of the C3 vertebral body. Inferior to the hyoid bone in the midline of the neck is the thyroid cartilage. The superior notch can be palpated as well as the bulging central region, commonly referred to as the “Adam’s apple.” The thyroid cartilage lies at the level of the C4 and C5 vertebral bodies. The cricoid cartilage lies inferior to the thyroid cartilage at the level of the C6 vertebral body. It forms a complete ring, which is narrower anteriorly and considerably wider posteriorly. The cricothyroid membrane can be palpated between the thyroid and cricoid cartilages. Inferior to the cricoid cartilage is the first tracheal ring. The carotid tubercle lies about 2.5 cm lateral to the cricoid cartilage. This is the small anterior tubercle on the transverse process of the C6 vertebra and is covered by overlying muscles. The common carotid artery runs adjacent to the tubercle, and locating this tubercle is frequently used as a landmark for approaching the inferior cervical (stellate) sympathetic ganglion. The transverse process of the atlas (C1) can be palpated inferior to the ear between the angle of the mandible and the styloid process of the temporal bone.
On the lateral aspect of the skull, about 4 cm superior to the midpoint of the zygomatic arch, is the pterion. This is an H-shaped formation of sutures that unite the frontal, parietal, sphenoid, and temporal bones. The pterion is important clinically because it overlies the anterior branches of the middle meningeal artery, and a blow to this vulnerable area may rupture the underlying vessels. Posterior landmarks begin with the occipital bone (occiput). On the occipital bone one can palpate the external occipital protuberance (inion) on the midline and the superior nuchal line extending laterally from the external occipital protuberance. These structures mark the line of separation between the neck inferiorly and the head superiorly. At the lateral end of the superior nuchal line, the rounded mastoid process of the temporal bone can be palpated (Fig. 16.1.3). Beginning at the external occipital protuberance and proceeding inferiorly, the spinous processes of the cervical vertebrae can be palpated along the midline of the neck. The midline of the neck is indented due to the presence of the nuchal ligament lying immediately over the spinous processes and the laterally located paraspinal muscles and the overlying trapezius muscle. The first cervical spinous process that can be palpated is C2 and the rest can be palpated sequentially to C7. The C7 spinous process, at the base of the neck, is the longest of the cervical spinous processes and serves as an important landmark for the end of the neck and the beginning of the thorax. Moving laterally from the spinous process of C2, the zygapophyseal joints of the cervical vertebrae, lying deep to the trapezius muscle, can be palpated sequentially as one proceeds inferiorly until the articulation between C7 and T1 is reached.
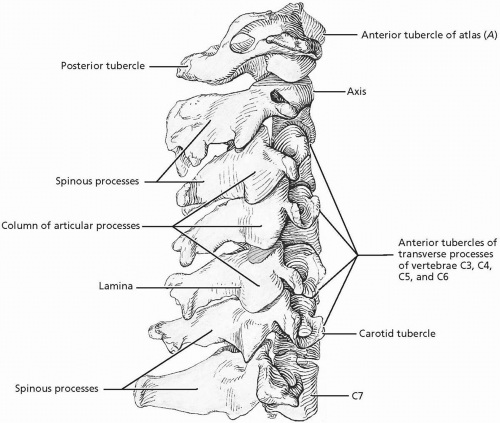 FIGURE 16.1.1. The cervical vertebrae. (From Agur AMR, Lee ML. Grant’s Atlas of Anatomy, 10th ed. Baltimore: Lippincott Williams & Wilkins, 1999.) |
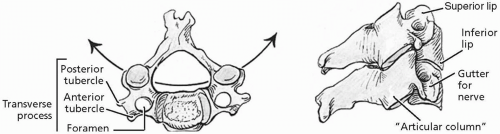 FIGURE 16.1.2. Cervical vertebrae, superior (left) and lateral (right) segmental views. (From Agur AMR, Lee ML. Grant’s Atlas of Anatomy, 10th ed. Baltimore: Lippincott Williams & Wilkins, 1999.) |
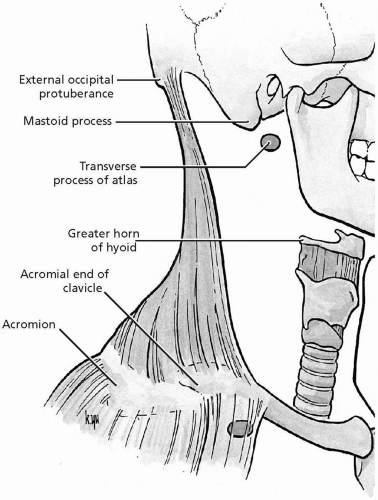 FIGURE 16.1.3. Bony landmarks of the neck, lateral view. (From Agur AMR, Lee ML. Grant’s Atlas of Anatomy, 10th ed. Baltimore: Lippincott Williams & Wilkins, 1999.) |
All seven cervical vertebrae are easily identified by the presence of a transverse foramen in each transverse process. These foramina transmit the vertebral artery and accompanying sympathetic nerve plexus. Cervical vertebrae C3-C7 share common anatomic features. Their relatively small cell body is wider side to side than front to back. The vertebral foramen is large in comparison to its size in other regions of the spine in order to accommodate the enlarged cervical spinal cord. The superior margin of the body curves up as an uncus (lip). The uncus articulates with beveled reciprocal facets on the inferior surface of the vertebral body above to form the uncovertebral joints (of Luschka). The pedicles are short and, along with the lateral aspect of the body, serve as the origin for the broad transverse processes. The superior and inferior vertebral notches are shallow, thus creating a very narrow intervertebral foramen. The superior and inferior articular processes are large, and their facets are oriented in the coronal plane. The facets of the superior articular
processes face posteriorly and slightly superior, while the facets of the inferior articular processes face anteriorly and slightly inferior. The spinous processes of C2-C6 may or may not be bifid. The C7 spinous process is the longest and most prominent cervical spinous process.
processes face posteriorly and slightly superior, while the facets of the inferior articular processes face anteriorly and slightly inferior. The spinous processes of C2-C6 may or may not be bifid. The C7 spinous process is the longest and most prominent cervical spinous process.
The first two cervical vertebrae are adapted for movements of the head. The atlas, C1, is attached to and “holds up” the skull. The axis, C2, provides the axis upon which the atlas and the attached skull can rotate. The atlas lacks a body and is composed of an anterior and posterior arch connected on each side to lateral masses. The lateral masses contain superior and inferior articular facets. The superior facets face superiorly and articulate with the occipital condyles of the occipital bone, while the inferior facets face inferiorly and articulate with the superior facets on the body of the axis. The internal surface of the anterior arch contains a small facet for articulation with the dens of the axis. Projecting off of the anterior arch is an anterior tubercle, while projecting off of the posterior arch is the posterior tubercle, which replaces the spinous process. The transverse processes are prominent and contain the vertebral foramina. On the superior surface of the posterior arch is a groove for the vertebral artery as it crosses the arch to enter the vertebral canal. The axis consists of a body and a vertical dens projecting superiorly off of the body. The dens has anterior and posterior facets for articulation with the facet on the anterior arch of the atlas and the transverse ligament of the atlas. The axis has no superior articular processes but does have superior articular facets on each side of the body. Its inferior articular processes, spinous process, and transverse processes resemble those of other cervical vertebrae.
In the cervical spine two types of joints, other than the uncovertebral joints described previously, unite cervical vertebrae C2-C7. These include facet joints (zygapophyseal joints) and intervertebral body joints (intervertebral discs). The facet joints are synovial joints between the articular processes of adjacent vertebrae. A thin, loose articular capsule surrounds each joint. The facet joints permit gliding movements between the vertebrae, and the shape of the articular surfaces limits the range of motion possible. Branches arising from the posterior primary rami of the spinal nerves innervate these joints. The intervertebral discs are fibrocartilaginous joints, designed for weight bearing and strength, situated between the bodies of adjacent vertebrae. Each intervertebral disc consists of an outer anulus fibrosus, composed of concentric lamellae of fibrocartilage, which surrounds a gelatinous nucleus pulposus. The anuli insert into the rounded rims on the articular surfaces of adjacent vertebral bodies. Branches arising from the anterior primary rami of the spinal nerves innervate the intervertebral discs. The intervertebral discs are avascular structures, which receive their blood supply by diffusion from the vertebral bodies.
Ligaments reinforce and stabilize the facet joints and the intervertebral discs between the C2-C7 vertebrae. The anterior and posterior longitudinal ligaments resist anterior and posterior displacement of the vertebral bodies on one another. The anterior longitudinal ligament limits extension of the vertebral column. The posterior longitudinal ligament runs within the vertebral canal beginning at C2 and limits flexion of the vertebral column. The strong, highly elastic, flattened ligamenta flava attach to the laminae of adjacent vertebrae to preserve the normal curvature of the vertebral column and straighten the vertebral column after it has been flexed. Short interspinous ligaments join adjacent spinous processes. In the cervical spine, the supraspinous ligament is replaced by the ligamentum nuchae, which separates the muscles on each side of the posterior neck and provides attachment for them. On its deep service, it attaches to the spinous processes of the cervical vertebrae, while superiorly it attaches to the external occipital protuberance and median nuchal line. Its posterior margin spans the distance between the external occipital protuberance and the spinous process of C7. This ligament helps to support the weight of the head when it is flexed.
The atlanto-occipital facets are obliquely positioned and permit nodding of the head and some lateral bending with practically no rotation.
The three atlantoaxial joints are specialized for head rotation. The median atlantoaxial joint is a pivot, with the atlas pivoting around the dens and carrying the head with it. Several strong ligaments provide the stability of the atlanto-occipital and atlantoaxial joints, most importantly the transverse ligament of the atlas, which converts the anterior arch of the atlas into a complete ring around the dens. The dens is connected to the occipital condyles of the occipital bone by the alar ligaments, which limit flexion and rotation. Extending superiorly and inferiorly from the transverse ligament of the atlas are superior and inferior crura, which together form a ligamentous complex referred to as the cruciform ligament. All of these ligaments lie deep to an upward extension of the posterior longitudinal ligament called the tectorial membrane.
The three atlantoaxial joints are specialized for head rotation. The median atlantoaxial joint is a pivot, with the atlas pivoting around the dens and carrying the head with it. Several strong ligaments provide the stability of the atlanto-occipital and atlantoaxial joints, most importantly the transverse ligament of the atlas, which converts the anterior arch of the atlas into a complete ring around the dens. The dens is connected to the occipital condyles of the occipital bone by the alar ligaments, which limit flexion and rotation. Extending superiorly and inferiorly from the transverse ligament of the atlas are superior and inferior crura, which together form a ligamentous complex referred to as the cruciform ligament. All of these ligaments lie deep to an upward extension of the posterior longitudinal ligament called the tectorial membrane.
The vertebral artery, which traverses the transverse foramina of the cervical vertebrae, typically arises from the subclavian artery at the base of the neck medial to the anterior scalene muscle. It runs superiorly and slightly posterior and usually enters the transverse foramen of the sixth cervical vertebra. Along with the artery are postganglionic sympathetic nerve fibers derived from the cervicothoracic or stellate ganglion and the vertebral vein. In the neck, small branches of the vertebral artery supply adjacent deep muscles of the neck and spinal branches enter the intervertebral foramina to supply the spinal cord and its coverings.
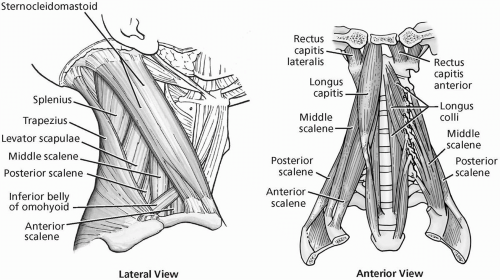 FIGURE 16.1.4. Superficial muscles of the neck. (From Agur AMR, Lee ML. Grant’s Atlas of Anatomy, 10th ed. Baltimore: Lippincott Williams & Wilkins, 1999.) |
Muscles help to stabilize the spine and control the effects of gravity (Fig. 16.1.4). In the cervical spine two major functional groups of muscles are present: extensors and flexors. Each group is also capable of rotating and lateral bending the cervical spine. The extensor muscles are situated posterior to the laminae and transverse processes of the cervical vertebrae. These muscles also lie deep to the cervical portion of the thoracolumbar fascia, which separates them from more superficial muscles (trapezius and rhomboids) attaching the spine to the upper limb.
The extensor muscles can be divided into four groups: the splenius, erector spinae, transversospinalis,
and suboccipital muscles. These muscles are arranged in three layers. The superficial layer contains the erector spinae and the splenius muscles. The intermediate layer contains the semispinalis and multifidus muscles of the transversospinalis group. The deep layer contains the interspinal, intertransverse, and rotator muscles of the transversospinalis group and the suboccipital muscles. The splenius muscles consist of the broad splenius capitis and the narrow splenius cervicis. The erector spinae muscles in the neck include the following from superficial to deep:
and suboccipital muscles. These muscles are arranged in three layers. The superficial layer contains the erector spinae and the splenius muscles. The intermediate layer contains the semispinalis and multifidus muscles of the transversospinalis group. The deep layer contains the interspinal, intertransverse, and rotator muscles of the transversospinalis group and the suboccipital muscles. The splenius muscles consist of the broad splenius capitis and the narrow splenius cervicis. The erector spinae muscles in the neck include the following from superficial to deep:
Iliocostalis cervicis
Longissimus capitis
Longissimus cervicis and capitis
Semispinalis cervicis and capitis
The multifidus muscles, lying deep to the semispinalis muscles, are thin in the cervical region. They arise from the articular processes of the lower four cervical vertebrae, run medially and superiorly and attach into the spinous processes of the axis and the upper two or three cervical vertebrae below the axis. The interspinous, intertransverse, and rotator muscles lie deep to the multifidus and are fairly well developed in the cervical region.
The suboccipital muscles connect the atlas and the axis to each other and to the skull and function in rotating and extending the head. This muscle group is composed of major and minor rectus muscles and superior and inferior oblique muscles. The rectus muscles produce extension of the atlanto-occipital joints, whereas the oblique muscles rotate the atlas and the skull on the axis. The major and minor oblique muscles and the major rectus muscle form the borders of the suboccipital triangle. This triangle contains the vertebral artery, suboccipital nerve, which supplies all of the suboccipital muscles and sensory greater occipital nerve.
The flexor muscles of the cervical spine are important in raising the head from a supine position. These prevertebral muscles in the cervical region are in close apposition to the vertebral column, directly flex the spine, and are represented by the longus colli and scalene muscles. The sternocleidomastoid muscle, attaching superiorly to the mastoid process of the skull and inferiorly to the manubrium of the sternum and the clavicle, is a more powerful flexor of the cervical spine than the prevertebral muscles because of its more anterior position. Not only does it draw the head forward but it also flexes the cervical spine. The sternocleidomastoid is also the most powerful rotator of the cervical spine but it works in combination with other muscles. The prevertebral muscles are innervated by the anterior primary rami of the cervical spinal nerves, while the sternocleidomastoid muscle is innervated by the accessory nerve (CN XI).
The spinal cord and its coverings (meninges) are located in the vertebral canal of the cervical spine. The cervical spine contains eight cervical spinal cord segments along with their anterior and posterior nerve roots. Cervical spinal nerves (eight pairs) are formed just outside the intervertebral foramina by the union of the anterior and posterior roots. In the cervical spine, the spinal nerves are formed above the vertebra they correspond to in number. Thus, the C1 spinal nerve is formed between the skull and the atlas, while the C8 spinal nerve is formed just outside the intervertebral foramen between the C7 and T1 vertebrae. After the spinal nerve is formed, it divides almost immediately into anterior and posterior primary rami. The posterior primary rami innervate segmentally skin and muscles of the back as well as the facet joints of the cervical spine. Communications between the anterior primary rami of the C1-C4 spinal nerves form the cervical plexus deep to the internal jugular vein and the sternocleidomastoid muscle in the neck. The phrenic nerve is the motor nerve to the diaphragm; it arises from the C3-C5 roots and descends through the neck on the anterior surface of the anterior scalene muscle down to the diaphragm.
The brachial plexus is derived from the anterior primary rami of the C5-T1 spinal nerves and provides motor and sensory innervation to the upper limb (Fig. 16.1.5). The
plexus extends from the neck into the axilla and is composed of roots, trunk divisions, cords, and branches. The roots and trunks with their branches lie in the posterior triangle of the neck, with the roots situated between the anterior and middle scalene muscles along with the subclavian artery. Branches in the neck include the dorsal scapular nerve (C5) to the rhomboid and levator scapulae muscles, the long thoracic nerve (C5-C7) to the serratus anterior muscle, and the suprascapular nerve (C5 and C6) running laterally across the posterior triangle of the neck to supply the supraspinatus and infraspinatus muscles and the shoulder joint.
plexus extends from the neck into the axilla and is composed of roots, trunk divisions, cords, and branches. The roots and trunks with their branches lie in the posterior triangle of the neck, with the roots situated between the anterior and middle scalene muscles along with the subclavian artery. Branches in the neck include the dorsal scapular nerve (C5) to the rhomboid and levator scapulae muscles, the long thoracic nerve (C5-C7) to the serratus anterior muscle, and the suprascapular nerve (C5 and C6) running laterally across the posterior triangle of the neck to supply the supraspinatus and infraspinatus muscles and the shoulder joint.
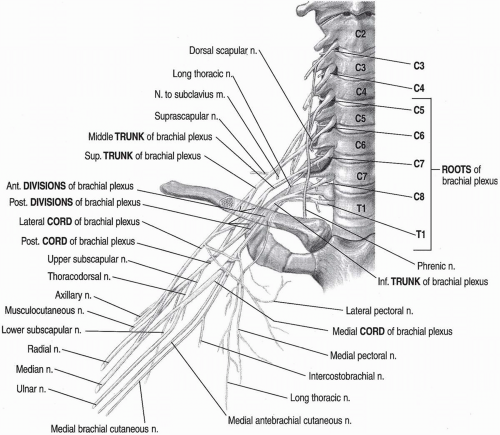 FIGURE 16.1.5. Brachial plexus, anterior view. (From Altcheck DW, Andrews JR. The athlete’s elbow: surgery and rehabilitation. Baltimore: Lippincott Williams & Wilkins, 2001.) |
There are several important soft tissue landmarks in the neck (Fig. 16.1.4.) The sternocleidomastoid muscle extends from the mastoid process of the skull to the manubrium of the sternum and clavicle, and divides the neck into anterior and posterior triangles. The muscle is palpable along its entire length. A lymph node chain is situated along the medial border of the sternocleidomastoid muscle. The trapezius muscle extends from the external occipital protuberance to the T12 vertebra and attaches laterally into the clavicle, the acromion, and the spine of the scapula. The muscle can be palpated along its superior border from its origin to its distal attachment. The trapezius and the sternocleidomastoid share a continuous attachment along the base of the skull to the mastoid process as well as a common nerve supply by way of the accessory nerve (CN XI). The superior border
of the trapezius forms the posterior boundary of the posterior triangle of the neck. The thyroid gland lies in the anterior triangle of the neck at the level of the C5-T1 vertebrae. It consists of right and left lobes located anterolateral to the larynx and trachea. An isthmus connects the lobes across the trachea on the midline of the neck at the level of the second to third tracheal rings. The esophagus, posterior to the trachea, begins at the inferior border of the thyroid cartilage and passes inferiorly through the superior thoracic aperture into the thorax. The carotid sheath is a fascial tube that extends from the base of the skull to the root of the neck deep to the sternocleidomastoid muscle in the anterior triangle of the neck. It contains the common and internal carotid arteries, internal jugular vein, and vagus nerve (CN X). At the level of the superior border of the thyroid cartilage, the common carotid artery divides into the internal and external carotid arteries. The root of the neck (supraclavicular fossa) is at the junction between the neck and the superior thoracic aperture. It is bounded anteriorly by the manubrium of the sternum, laterally by the first rib, and posteriorly by the body of the T1 vertebra. The sternocleidomastoid muscle, as it approaches its distal attachment, and covered by the platysma muscle, can be palpated.
of the trapezius forms the posterior boundary of the posterior triangle of the neck. The thyroid gland lies in the anterior triangle of the neck at the level of the C5-T1 vertebrae. It consists of right and left lobes located anterolateral to the larynx and trachea. An isthmus connects the lobes across the trachea on the midline of the neck at the level of the second to third tracheal rings. The esophagus, posterior to the trachea, begins at the inferior border of the thyroid cartilage and passes inferiorly through the superior thoracic aperture into the thorax. The carotid sheath is a fascial tube that extends from the base of the skull to the root of the neck deep to the sternocleidomastoid muscle in the anterior triangle of the neck. It contains the common and internal carotid arteries, internal jugular vein, and vagus nerve (CN X). At the level of the superior border of the thyroid cartilage, the common carotid artery divides into the internal and external carotid arteries. The root of the neck (supraclavicular fossa) is at the junction between the neck and the superior thoracic aperture. It is bounded anteriorly by the manubrium of the sternum, laterally by the first rib, and posteriorly by the body of the T1 vertebra. The sternocleidomastoid muscle, as it approaches its distal attachment, and covered by the platysma muscle, can be palpated.
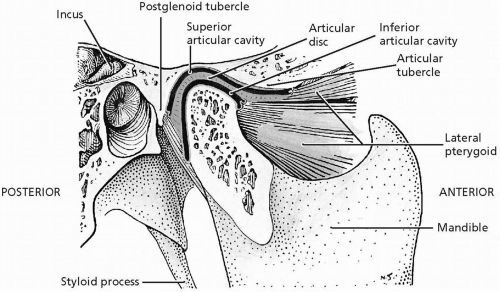 FIGURE 16.1.6. Temporomandibular joint. (From Agur AMR, Lee ML. Grant’s Atlas of Anatomy, 10th ed. Baltimore: Lippincott Williams & Wilkins, 1999.) |
The temporomandibular joint (TMJ) is a synovial joint, anterior to the auricle of the ear, where the head of the condyle of the mandible articulates with the articular tubercle and the mandibular fossa of the temporal bone (Fig. 16.1.6). An articular disc divides the joint cavity into superior and inferior compartments each lined by a synovial membrane. The fibrous capsule attaches superiorly to the margins of the articular area on the temporal bone and around the neck of the condyle. The capsule is thickened laterally to form the lateral ligament, which strengthens the TMJ. Two additional ligaments connect the mandible to the skull but add little strength to the TMJ. The stylomandibular ligament extends from the styloid process of the temporal bone to the posterior aspect of the angle of the mandible. The sphenomandibular ligament, medial to the TMJ, runs from the spine of the sphenoid bone to the lingula of the mandible.
REFERENCES
1. Basmajian JV, Slonecker CE. Grant’s method of anatomy, 11th ed. Baltimore: Williams & Wilkins, 1989.
2. Clemente CD. Gray’s anatomy of the human body, American 30th ed. Philadelphia: Lea & Febiger, 1985.
3. Moore KL, Agur AM. Essential clinical anatomy. Baltimore: Williams & Wilkins, 1996.
4. Rosse C, Gaddum-Rosse P. Hollinshead’s textbook of anatomy, 5th ed. Philadelphia: Lippincott-Raven, 1997.
5. Williams PL, Warwick R, Dyson M, Bannister LH. Gray’s anatomy, British 37th ed. London: Churchill Livingstone, 1989.
6. Woodburne RT, Burkel WE. Essentials of human anatomy, 9th ed. New York: Oxford University Press, 1994.
16.2 Physical Examination
Kendra Mccamey
Derek Olson
Steven J. Karageanes
OBSERVATION
The head examination begins with inspection. The athlete’s disposition alerts the examiner to the level of distress of the athlete. Note any lacerations, lesions, or swelling. Patterns of bruising should also be noted, although bruising may take up to 24 hours to appear. Bruising of the eyelids and orbital region is typically associated with an orbital fracture, basilar skull fracture, or fracture of the base of the anterior cranial fossa. Battle’s sign is demonstrated by bruising behind the ear and along the hairline, which is associated with a basilar skull or temporal bone fracture (1). Evaluate for asymmetry of the athlete’s facial features. Although many people do not have perfectly aligned eyes, pronounced asymmetry may be a sign of a zygomatic bone fracture.
Evaluate the athlete’s eyelids for significant ptosis, which may be associated with cranial nerve damage. Normally, the athlete’s upper eyelid should not cover the pupil. If the athlete has significant swelling of the eyelids that prevents him or her from opening the eye, assume the globe is ruptured and get an ophthalmologic referral immediately. Palpate and inspect the rest of the skull, noting any hematoma, deformity, and areas of pain to palpation.
While examining the oral cavity, ask the athlete to close the teeth together and examine the bite, noting alignment and pain with biting. Malaligned teeth are common, so that is not necessarily diagnostic for a fracture. Check to see if there are any teeth missing, and tap them to see if they are loose or if there is any pain. Evaluate the integrity of the gingiva, buccal mucosa, and tongue. While you are evaluating the athlete’s bite, examine the temporomandibular joint (TMJ) by placing your index fingers over the joint and noting motion and position. Crepitus or pain over the TMJ is a sign of degeneration or significant injury of the joint (1). The TMJ is often the cause of severe headaches or earaches, so examine it carefully, particularly when you find evidence of mandibular trauma.
A common deformity seen in wrestlers is “cauliflower ear,” in which the auricular cartilage hypertrophies and thickens from subcutaneous bleeding due to recurrent friction and twisting of the ear. An otoscopic examination
can visualize the ear canals and tympanic membranes. Evaluate for both clear and bloody discharge. As with the nose, clear discharge may be the sign of a cerebrospinal fluid (CSF) leak and skull fracture. Also, the ear tips should align with the corner of the eyes, so any discrepancy should be evaluated further.
can visualize the ear canals and tympanic membranes. Evaluate for both clear and bloody discharge. As with the nose, clear discharge may be the sign of a cerebrospinal fluid (CSF) leak and skull fracture. Also, the ear tips should align with the corner of the eyes, so any discrepancy should be evaluated further.
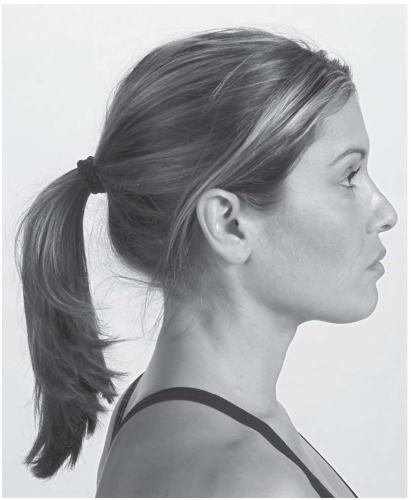
Inspection of the cervical spine should reveal sufficient cervical lordosis, or a backward curve (Fig. 16.2.1). Loss of this curve may be a clue to the source of pain, such as degenerative disc disease or spondylosis. Poor posture, particularly in more mature athletes with early spinal osteoarthritis or disc degeneration, leads to increased “humping” at the C6-T2 region (2). The head should sit between the shoulders, not in front of them. Note any abnormal rotation or side bending. When inspecting the athlete from the front, the nose should be in line with the sternum. From the side, the earlobe should be in line with the acromion process. The muscle bulk of the trapezius, deltoid, and sternocleidomastoid muscles should be symmetrical; however, often the athlete’s dominant shoulder will lie lower than the nondominant shoulder.
PALPATION
Starting at the anterior cervical region superiorly, palpate the hyoid bone, thyroid cartilage, first cricoid cartilage ring, and carotid tubercle. The thyroid gland is just inferior and lateral to the thyroid cartilage (Fig. 16.2.2), while the sternocleidomastoid lies one fingerbreadth laterally from the thyroid gland. Palpate these structures, noting pain or deformity.
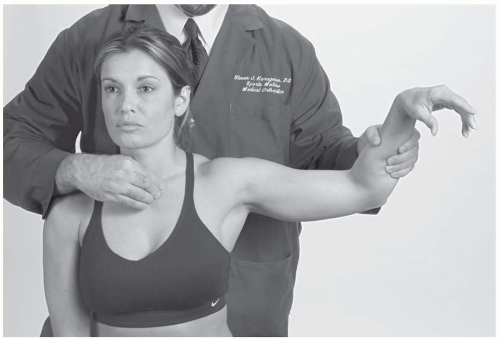
At the base of the neck anteriorly, palpate the sternoclavicular (SC) joints and the length of the clavicles bilaterally, noting position, joint play, and motion. The position of the SC joints can be gauged by resting the index finger on the anterior and superior surfaces and comparing position. Passively elevate, rotate, and extend the athlete’s arm while monitoring the SC joint to further evaluate joint motion (Fig. 16.2.3). The sternocleidomastoid inserts here as well, so palpate its enthesis for pain or disruption.
The cervical spine examination can be done with the athlete supine to allow the neck muscles to relax, although the examination can also be done with the athlete seated. The examiner should palpate the suboccipital fossae and note tenderness and somatic dysfunction. Traveling superolaterally from the fossae are the greater occipital nerves, which may be tender in athletes with chronic headaches and in those with atlantoaxial and occipitoatlantal dysfunctions.
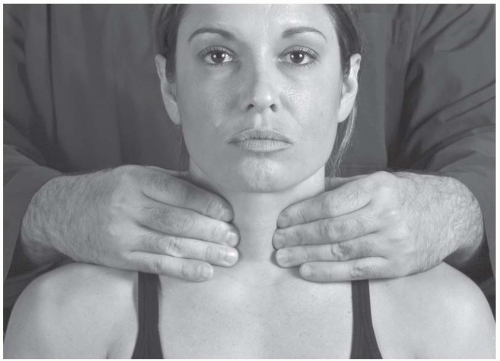 FIGURE 16.2.2. Palpating the thyroid gland, with the athlete sitting up. The examiner’s fingers reach around the sternocleidomastoid. |
The skull should be examined for tenderness, depressions, or bony movement, particularly with any evidence of blunt trauma. An athlete with an obvious open skull fracture should be immediately transported to emergency services. Prominent posterior landmarks to examine include the occiput, mastoid processes, inion, and superior nuchal line. Anteriorly, palpate the orbital rim and zygomatic bone for crepitus, pain, or a stepoff, which can be associated with a fracture. Care must be taken to palpate gently throughout this examination in case an unstable fracture exists, lest the examiner displaces any fracture into a disadvantageous position.
Inspect and palpate the athlete’s nose for deviation, depression of the nasal bridge, or nasal discharge. Plug one nostril by pressing on the side of the naris and ask the athlete to gently blow out through his or her nose, noting the ease and amount of air flow. If the athlete does have discharge, determine if the discharge is CSF secondary to an ethmoid fracture. If the discharge is bloody, use a piece of white gauze to soak up the discharge. If there is a yellowishorange halo surrounding the central bloody discharge, then a CSF leak is likely. Athletes often complain of a salty taste in the mouth when they have a CSF leak; also ask the athlete if his or her sense of smell has changed, because fracture of the frontobasal or nasoethmoid bones can result in an altered sensation of smell.
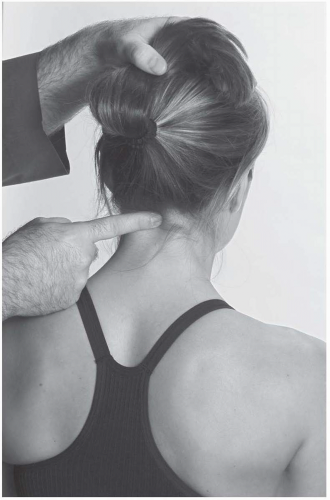
The first palpable vertebral structure below the occiput is the spinous process of C2. Palpate along the spinous processes of C2 through C7, noting pain, swelling, stepoffs, and any differences in interspinous distance (Fig. 16.2.4). Note the superior nuchal ligament and the interspinous ligaments during palpation, especially in injuries involving sudden hyperflexion of the neck. Palpate with the neck flexed as well.
The spinous processes of C6 and C7 should be more prominent than those of C3-C5, but the C6 prominence disappears when the neck is in extension. Any cervical spine with spinous processes that show either a stepoff or a significant difference in interspinous distance needs radiographs taken to rule out instability or fracture. The transverse process of C1 can be palpated inferior and anterior to the mastoid process.
Move laterally and palpate along the facet joints, noting any prominent pillars or tender
points (Fig. 16.2.5). Note whether one facet is more prominent than the one on the contralateral side, for this can help identify a somatic dysfunction. Finally, continue to move laterally and palpate the musculature in the posterior neck.
points (Fig. 16.2.5). Note whether one facet is more prominent than the one on the contralateral side, for this can help identify a somatic dysfunction. Finally, continue to move laterally and palpate the musculature in the posterior neck.
RANGE OF MOTION
Active
The examiner asks the athlete to perform four motions:
Bend the head backward.
Bring the chin to the chest.
Look over the left and right shoulders.
Bring each ear to each shoulder.
Normal range of motion of the cervical spine is 60 to 90 degrees in flexion, 70 degrees in extension, 20 to 45 degrees in side bending, and 70 to 90 degrees in rotation. Cervical flexion primarily occurs at the occipitoatlantal joint and centers on the C5 and C6 vertebrae, while cervical extension centers around the C6 and C7 vertebrae. Rotation occurs primarily at the atlantoaxial joint, and normal range of motion is between 70 and 90 degrees. Side bending occurs primarily at the occipitoatlantal and atlantoaxial joints. Vertebrae C3 through C7 move in flexion and extension as one continuous group. While the athlete is flexing, pay close attention to the spinous processes and note if any vertebral body is more prominent than the others (3).
Passive
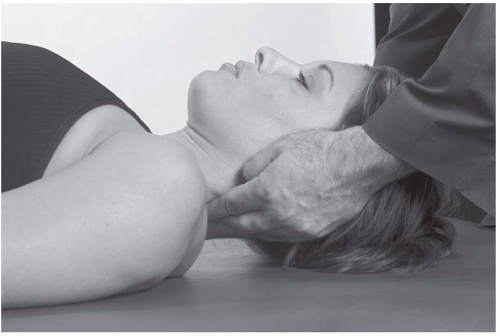
Passive range of motion (PROM) should be evaluated and compared with active range of motion. By placing the athlete in a supine position, the cervical postural muscles relax, and PROM can be more accurately assessed. Both of the examiner’s hands should be on the athlete’s head as it is moved through the ranges of motion. Painful barriers, muscle guarding, and anatomic restrictions should be noted.
Intersegmental Motion Testing
Occipitoatlantal Motion
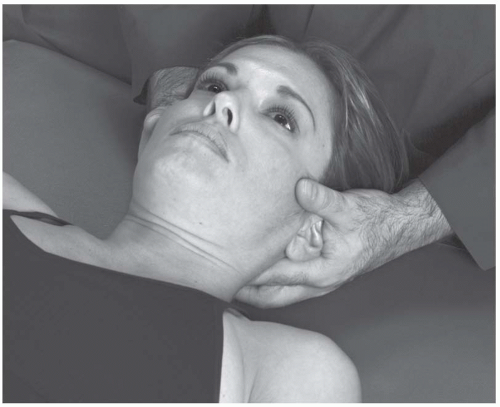
The athlete lies supine with the examiner sitting at the head of the table. The examiner’s hands hold the athlete’s head while the index and middle fingers are placed on the suboccipital space. The examiner introduces lateral translation to the left and right, noting ease of motion or restriction (Fig. 16.2.6A). Testing is repeated in flexion and extension of the head. Note any motion restriction or palpable dysfunction in the occipital articulation.
Atlantoaxial Motion
With the athlete supine, the examiner flexes the head while monitoring the lateral masses of the atlas with the index finger pads (flexion locks out the C2-C7 vertebrae). The head is rotated left and right, while the examiner notes any restriction or pain (Fig. 16.2.6B).
C2 through C7 Vertebrae
Intersegmental motion is more difficult to assess in the C2-C7 vertebrae, and the examiner will have more success palpating for joint play and tissue spring in each level. The examiner places the pads of the index fingers along the lateral side of the posterior pillars of the specific segment, while the rest of the hand supports the athlete’s head. The fingers introduce side bending into that segment, translating it left and right. Note spring, tenderness, and amount of play. Translation is alternated between the fingers, even lightly “bouncing” the segment
four or five times before the examiner can get a feel for the restriction. This helps to identify whether a segmental lesion is restricted in left or right side bending (Fig. 16.2.7).
four or five times before the examiner can get a feel for the restriction. This helps to identify whether a segmental lesion is restricted in left or right side bending (Fig. 16.2.7).
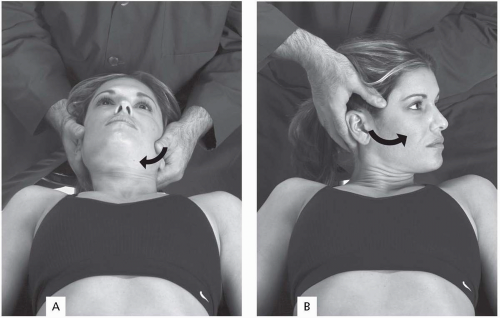 FIGURE 16.2.6. Upper cervical motion with athlete supine: occipitoatlantal motion (A); atlantoaxial motion (B). |
The examiner then moves the index finger pads to touch the posterior aspect of the facets and introduces anterior translation, noting spring, tenderness, and amount of play. This helps to identify whether a segmental lesion is restricted moving in extension. The vertebrae follow type II mechanics, so side bending and rotation are on the same side. Therefore, if a segment resists flexion and side bending to the left, it is classified as a vertebral segment that is positionally extended, and side-bent and rotated to the right.
STRENGTH
Evaluate strength with resisted isometric movements. The examiner can evaluate flexion, extension, side bending, and rotation by resisting the athlete’s head with a stabilizing hand while the athlete is seated. This is usually done with minimal spine motion in order to minimize any opportunity for injury (1,4).
TEMPOROMANDIBULAR JOINT
Inspect the athlete opening and closing his or her mouth. This motion should be smooth,
and there should be no deviation of the jaw to the left or right. If the athlete’s jaw does deviate, it usually will deviate to the side of TMJ pathology. Movements of the TMJ include opening of the mouth; closing of the mouth; and protrusion, retrusion, and lateral deviation of the mandible. Normal range of motion on opening of the mandible is from 35 to 50 mm. Functionally, only 25 to 35 mm of opening is needed for activities of daily living. To assess normal range of opening, have the athlete place two or three flexed proximal interphalangeal (PIP) joints into the mouth. An inability to perform the PIP test may indicate a TMJ problem.
and there should be no deviation of the jaw to the left or right. If the athlete’s jaw does deviate, it usually will deviate to the side of TMJ pathology. Movements of the TMJ include opening of the mouth; closing of the mouth; and protrusion, retrusion, and lateral deviation of the mandible. Normal range of motion on opening of the mandible is from 35 to 50 mm. Functionally, only 25 to 35 mm of opening is needed for activities of daily living. To assess normal range of opening, have the athlete place two or three flexed proximal interphalangeal (PIP) joints into the mouth. An inability to perform the PIP test may indicate a TMJ problem.
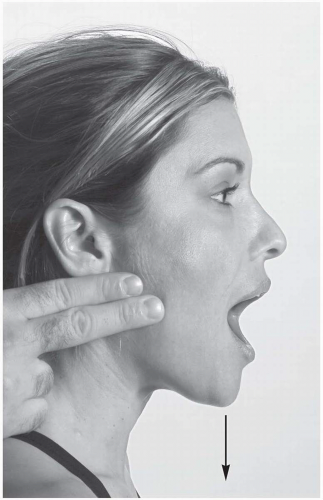
To palpate the TMJ, place your fingers either anterior to the tragus over the mandibular condyles or directly over the external auditory meatus. Ask the athlete to open and close his or her mouth while you palpate for clicking, grinding, or popping, noting any pain with this movement (Fig. 16.2.8).
Normal range of motion on protrusion of the mandible is from 3 to 6 mm and on retrusion it is from 3 to 4 mm; however, this may vary greatly for the athlete with a significant overbite or underbite. Normal lateral deviation is from 10 to 15 mm to each side.
Test TMJ strength by resisting mandibular movement. While testing these movements, note strength and any pain that is referred to the TMJ itself. Place your fingers under the athlete’s mandible and have him or her open the mouth against your resistance to test depression of the jaw. To test occlusion of the mandible, place your fingers on the athlete’s lower teeth and have him or her close the mouth against your resistance. Make sure you tell the athlete that you are testing strength and that full closing of the jaw is not necessary so that he or she does not bite your fingers. To test lateral deviation, place one hand on the temple of the athlete’s head opposite the side that you want to test and place the other hand on the athlete’s jaw on the side you want to test and ask the athlete to move the mandible toward the hand that is on his or her jaw.
Jaw Reflex. This tests cranial nerve V, which is important in TMJ motion. The athlete gently opens his or her mouth while the examiner places his or her thumb on the athlete’s chin. The examiner uses a reflex hammer to tap the thumb. A normal reflex response is closing of the mouth (4).
Positive test: Absence or hyperreactivtity is considered loss of the jaw reflex.
Indicates: Fifth cranial nerve injury.
Chvostek’s Test. This test evaluates for seventh cranial nerve (facial) pathology. Irritation to the seventh cranial nerve will often refer pain to the area of the TMJ. The examiner taps on the parotid gland and observes for a reaction (4).
Positive test: The facial muscles twitch as a result of the tapping.
Indicates: Seventh cranial nerve palsy or injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree