Harvesting Semitendinosus and Gracilis for Free Tendon Graft
Nicholas L. Strasser
Diane L. Dahm
INTRODUCTION
There are multiple studies showing that semitendinosus or gracilis composite (STG) grafts provide satisfactory strength and stiffness for anterior cruciate ligament (ACL) reconstruction with minimal loss of function (1, 2 and 3). In anterior talofibular ligament (ATFL) and/or calcaneofibular ligament (CFL) reconstructions, use of a free STG graft can be obtained with minimal additional exposure and without compromising the function of the peroneal tendons (4). For chronic Achilles tendon ruptures, use of STG allows for preservation of other foot tendons (i.e., flexor hallucis longus or peroneus brevis) that if used would cause the foot to be deprived of motor strength (5). Free tendon grafts are useful for peroneal tendon reconstruction particularly when both tendons are diseased or deficient or for revision operations. One can harvest the STG alone or in combination depending on the desired amount of tissue required for the reconstruction. Harvesting the STG is relatively simple and quick with few complications and minimal long-term consequences.
INDICATIONS AND CONTRAINDICATIONS
The primary reason for harvesting a hamstring tendon traditionally has been for use as a free autograft in reconstruction of the ACL. More recently, use of either the semitendinosus or gracilis has been described in the foot and ankle literature to reconstruct chronic ATFL tears (6), combined ATFL and CFL tears (4,7), chronic Achilles tendon ruptures (5), and peroneal tendon ruptures.
Contraindications to harvesting the STG are relatively few. These include previous tendon harvesting either for ACL reconstruction or other ligament/tendon reconstructions. In addition, caution should be used in patients who require strong knee flexors in deep knee flexion for their sport or occupation (2,8,9).
PREOPERATIVE PLANNING
The patient should be examined and their past surgical history reviewed for any previous graft harvest and the presence of a hamstring tendon. If a previous harvest has been performed for a ligament or tendon reconstruction, a contralateral harvest can be considered depending on surgeon preference. A separate table to prepare the graft and closed tendon strippers should be available prior to beginning the surgical procedure. Tendon sizers and a graft table with tensioner should also be available as well as a looped, nonabsorbable braided suture attached to a Keith-needle (Arthrex FiberLoop). Harvesting from the supine position will be described. A description of harvesting both
tendons will be described; however, one or both tendons can be harvested depending on the amount of tissue required for the reconstruction.
tendons will be described; however, one or both tendons can be harvested depending on the amount of tissue required for the reconstruction.
SURGICAL TECHNIQUE
The patient can be positioned supine, lateral, or prone depending on the approach required for the primary surgery. A tourniquet is applied at the thigh and the leg is exsanguinated.
The graft can be harvested with the knee flexed at 90° or in a figure-of-four position, which aids in relaxing tension on the tendons and saphenous nerve as well as improving exposure. Our preference is to use the ipsilateral extremity for harvesting the STG autograft.
A vertical, oblique, or transverse incision can be used. The incision is typically 3 cm in length and is centered 3 to 4 cm distal to the joint line, halfway between the tibial tubercle and posteromedial border of the tibia (Fig. 45.1). We prefer a vertical incision when harvesting an STG autograft in association with an ACL reconstruction. However, an oblique incision may be preferable when harvesting the STG in other cases to minimize risk of injury to the infrapatellar branch of the saphenous nerve (IPBSN) (10). The gracilis is cord-like and, in patients with minimal subcutaneous fat, can often be palpated prior to skin incision.
Dissection is carried down through the subcutaneous fat to expose the sartorius tendon (Fig. 45.2A). Care should be taken to avoid the IPBSN as it courses on the medial aspect of the knee and runs superficial to the sartorius tendon (Fig. 45.2B). Deep to the sartorius, the STG can be palpated as separate structures. The gracilis is a round cord-like structure compared to the flatter and more inferior semitendinosus tendon.
The sartorius, gracilis, and semitendinosus all fuse distally forming the pes anserinus tendon and inserts on the proximal anteromedial aspect of the tibia. The sartorius tendon is carefully incised in parallel fashion to the gracilis and semitendinosus superior to the gracilis (Fig. 45.3). Caution should be exercised not to damage the underlying gracilis and semitendinosus tendons as well as the superficial medial collateral ligament (MCL). By preserving the overlying sartorius tendon, it can serve as a soft tissue cover for the harvest site. The gracilis and semitendinosus often adhere to the overlying sartorius, so care must be exercised to prevent damaging the sartorius while exposing the deeper structures.
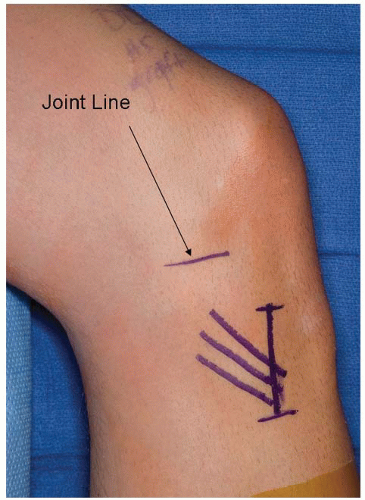
FIGURE 45.1 Skin incision centered 3 to 4 cm distal to joint line and halfway between the tibial tubercle and posterior border of the tibia.
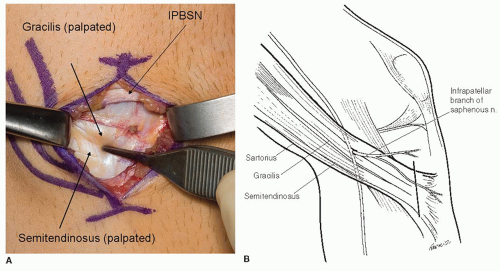
FIGURE 45.2 A: Overlying sartorius is exposed. One can appreciate the IPBSN in the superior aspect of the wound and the gracilis and semitendinosus palpated beneath sartorius. B:Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








