Hand
EPIDEMIOLOGY
Metacarpal and phalangeal fractures are common, comprising 10% of all fractures; >50% of these are work related.
The 1998 United States National Hospital Ambulatory Medical Care Survey found phalangeal (23%) and metacarpal (18%) fractures to be the second and third most common hand and forearm fractures following radius fractures. They constitute anywhere from 1.5% to 28% of all emergency department visits, depending on survey methods.
Location: Border digits are most commonly involved. The small finger axis is the most commonly injured and may constitute 37% of total hand fractures. Studies present conflicting data on incidence. A 1996 study in Injury indicated a series of 1,358 hand fractures were distributed as follows: 57.4% proximal phalanx, 30.4% middle phalanx, 12.2% metacarpal.
Male-to-female ratios run from 1.8:1 to 5.4:1, with higher ratios seen in the age groups associated with the greatest incidence (sports injuries in the early third decade, workplace injuries in the fifth decade, and falls in the seventh decade).
ANATOMY
Metacarpals
They are bowed, concave on palmar surface.
They form the longitudinal and transverse arches of the hand.
The index and long finger carpometacarpal (CMC) articulation is rigid.
The ring and small finger CMC articulation is flexible.
Three palmar and four dorsal interosseous muscles arise from metacarpal shafts and flex the metacarpophalangeal (MCP) joints.
These muscles create deforming forces in the case of metacarpal fractures, typically flexing the fracture (apex dorsal angulation).
Phalanges
Proximal phalanx fractures usually angulate into extension (apex volar).
The proximal fragment is flexed by the interossei.
The distal fragment is extended by the central slip.
Middle phalanx fractures are unpredictable.
MECHANISM OF INJURY
A high degree of variation in mechanism of injury accounts for the broad spectrum of patterns seen in skeletal trauma sustained by the hand.
Axial load or “jamming” injuries are frequently sustained during ball sports or sudden reaches made during everyday activities such as to catch a falling object. Patterns frequently resulting from this mechanism are shearing articular fractures or metaphyseal compression fractures.
Distal phalanx fractures usually result from crush injuries and are comminuted tuft fractures.
Axial loading along the upper extremity must also make one suspicious of associated injuries to the carpus, forearm, elbow, and shoulder girdle.
Diaphyseal fractures and joint dislocations usually require a bending component in the mechanism of injury, which can occur during ball-handling sports or when the hand is trapped by an object and is unable to move with the rest of the arm.
Individual digits can easily be caught in clothing, furniture, or workplace equipment to sustain torsional mechanisms of injury, resulting in spiral fractures or more complex dislocation patterns.
Industrial settings or other environments with heavy objects and high forces lead to crushing mechanisms that combine bending, shearing, and torsion to produce unique patterns of skeletal injury and associated soft tissue damage.
Ring avulsion injuries result in severe soft tissue injury ranging from laceration to complete amputation.
CLINICAL EVALUATION
History: A careful history is essential because it may influence treatment. It should include the patient’s:
Age
Hand dominance
Occupation
Systemic illnesses
Mechanism of injury: crush, direct trauma, twist, tear, laceration, etc.
Time of injury (for open fractures)
Exposure to contamination: barnyard, brackish water, animal/human bite
Treatment provided: cleansing, antiseptic, bandage, tourniquet
Financial issues: workers’ compensation
Physical examination includes:
Digital viability (capillary refill should be <2 seconds)
Neurologic status (documented by two-point discrimination [normal is 6 mm] and individual muscle testing)
Rotational and angulatory deformity
Range of motion (documented by goniometer)
Malrotation at one bone segment is best represented by the alignment of the next, more distal segment. This alignment is best demonstrated when the intervening joint is flexed to 90 degrees. Comparing nail plate alignment is an inadequate method of evaluating rotation.
RADIOGRAPHIC EVALUATION
Posteroanterior, lateral, and oblique radiographs of the affected digit or hand should be obtained. Injured digits should be viewed individually to minimize overlap of other digits over the area of interest.
CLASSIFICATION
Descriptive
Open versus closed injury
Bone involved
Location within bone
Fracture pattern: comminuted, transverse, spiral, vertical split
Presence or absence of displacement
Presence or absence of deformity (rotation and/or angulation)
Extra-articular versus intra-articular fracture
Stable versus unstable
Open Fractures
Swanson, Szabo, and Anderson
Type I: Clean wound without significant contamination or delay in treatment and no systemic illness
Type II: One or more of the following:
Contamination with gross dirt/debris, human or animal bite, warm lake/river injury, barnyard injury
Delay in treatment >24 hours
Significant systemic illness, such as diabetes, hypertension, rheumatoid arthritis, hepatitis, or asthma
Rate of infection: Type I injuries (1.4%)
Type II injuries (14%)
Neither primary internal fixation nor immediate wound closure is associated with increased risk of infection in type I injuries. Primary internal fixation is not associated with increased risk of infection in type II injuries.
Primary wound closure is appropriate for type I injuries, with delayed closure appropriate for type II injuries.
Orthopaedic Trauma Association Classification of Metacarpal and Phalangeal Fractures
See Fracture and Dislocation Classification Compendium at http://www.ota.org/compendium/compendium.html.
TREATMENT: GENERAL PRINCIPLES
“Fight-bite” injuries: Any short, curved laceration overlying a joint in the hand, particularly the MCP joint, must be suspected of having been caused by a tooth. These injuries must be assumed to be contaminated with oral flora and should be addressed with broadspectrum antibiotics (need anaerobic coverage) and irrigation and debridement.
Animal bites: Antibiotic coverage is needed for Pasteurella and Eikenella.
There are essentially six major treatment alternatives:
Immediate motion
Temporary splinting
Closed reduction and internal fixation (CRIF)
Open reduction and internal fixation (ORIF)
Immediate reconstruction
External fixation
The general advantages of entirely nonoperative treatment are lower cost and avoidance of the risks and complications associated with surgery and anesthesia. The disadvantage is that stability is less assured than with some form of operative fixation.
CRIF is expected to prevent overt deformity but not to achieve an anatomically perfect reduction. Pin tract infection is the prime complication that should be mentioned to patients in association with CRIF, unless K-wires are buried.
Open treatments are considered to add the morbidity of surgical tissue trauma, titrated against the presumed advantages of the most anatomic and stable reduction.
Critical elements in selecting between nonoperative and operative treatment are the assessments of rotational malalignment and stability.
If carefully sought, rotational discrepancy is relatively easy to determine.
Defining stability is somewhat more difficult. Some authors have used what seems to be the very reasonable criterion of maintenance of fracture reduction when the adjacent joints are taken through at least 30% of their normal motion.
Contraction of soft tissues begins approximately 72 hours following injury. Motion should be instituted by this time for all joints stable enough to tolerate rehabilitation.
General indications for surgery include:
Open fractures
Unstable fractures
Irreducible fractures
Multiple fractures
Fractures with bone loss
Fractures with tendon laceration, neurovascular injury, or soft tissue injury requiring coverage
Treatment of stable fractures:
Buddy taping or splinting is performed, with repeat radiographs in 1 week.
Initially unstable fractures that are reduced and then converted into a stable position: External immobilization (cast, cast with outrigger splint, gutter splint, or anterior-posterior splints) or percutaneous pinning which prevents displacement and permits earlier mobilization.
Treatment of unstable fractures:
Unstable fractures that are irreducible by closed means or exhibit continued instability despite closed treatment require CRIF or ORIF, including Kirschner wire fixation, interosseous wiring, tension band technique, interfragmentary screws alone, or plates and screws.
Fractures with segmental bone loss
These continue to be problematic. The primary treatment should be directed to the soft tissues, maintaining length with Kirschner wires or external fixation. These injuries usually require secondary procedures, including bone grafting.
MANAGEMENT OF SPECIFIC FRACTURE PATTERNS
Metacarpals
Metacarpal Head
Fractures include:
Epiphyseal fractures
Collateral ligament avulsion fractures
Oblique, vertical, and horizontal head fractures
Comminuted fractures
Boxer’s fractures with joint extension
Fractures associated with bone loss
Most require anatomic reduction (if possible) to reestablish joint congruity and to minimize posttraumatic arthrosis.
Stable reductions of fractures may be splinted in the “protected position,” consisting of metacarpal-phalangeal flexion >70 degrees to minimize joint stiffness (Fig. 24.1).
Displaced metacarpal head fractures usually require open reduction internal fixation with K-wires or headless compression screws.
Early range of motion is essential.
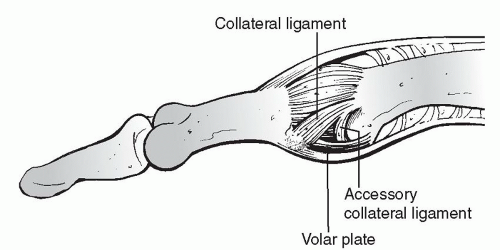 FIGURE 24.1 Left: The collateral ligaments of the MCP joints are relaxed in extension, permitting lateral motion, but they become taut when the joint is fully flexed. This occurs because of the unique shape of the metacarpal head, which acts as a cam. Right:
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|





