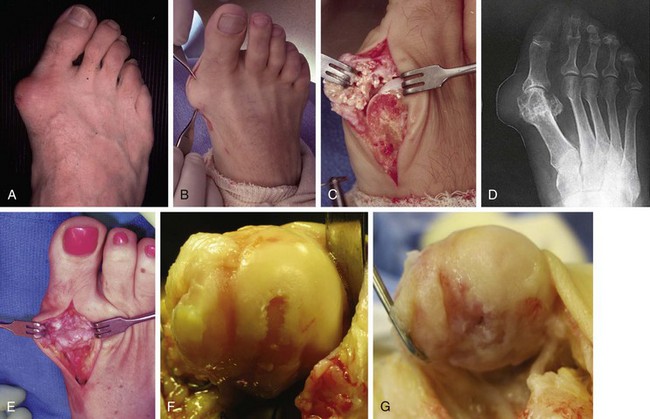
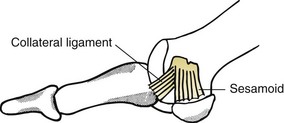
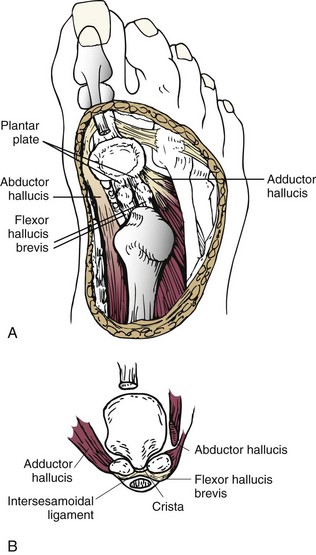
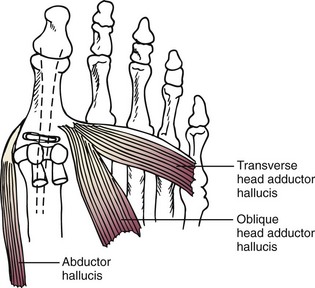
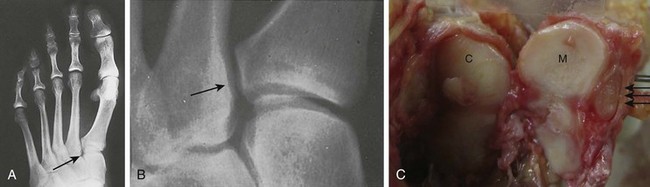
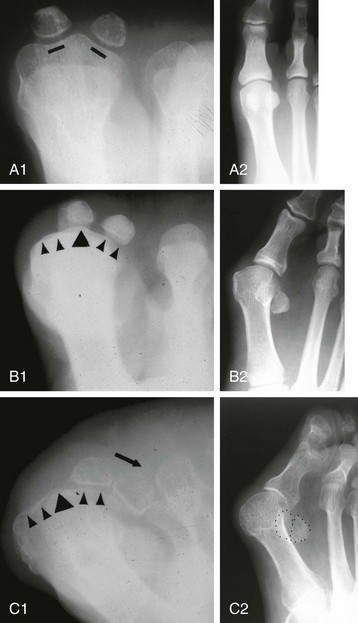
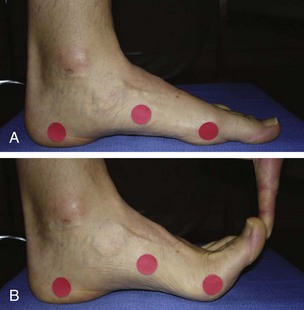
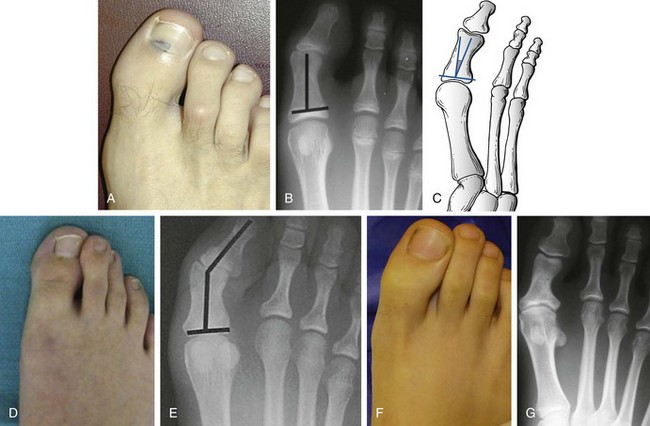
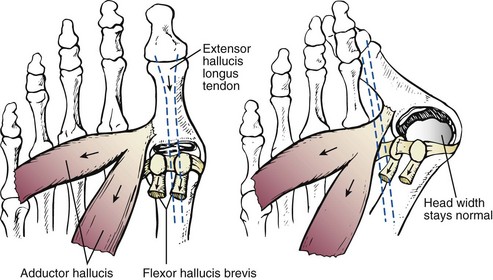
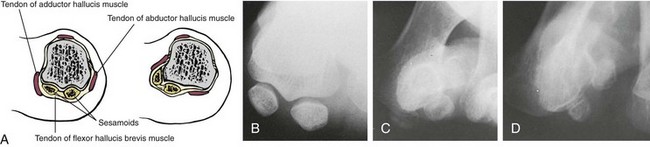
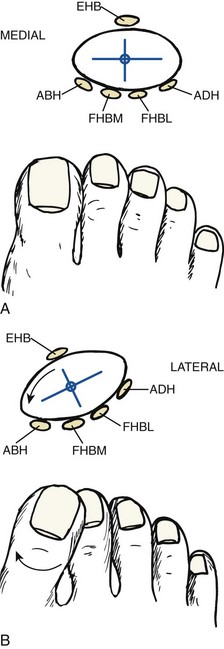
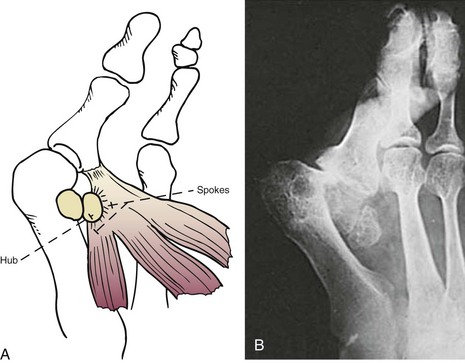
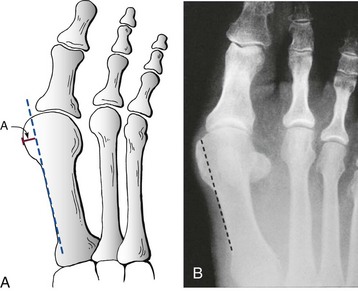
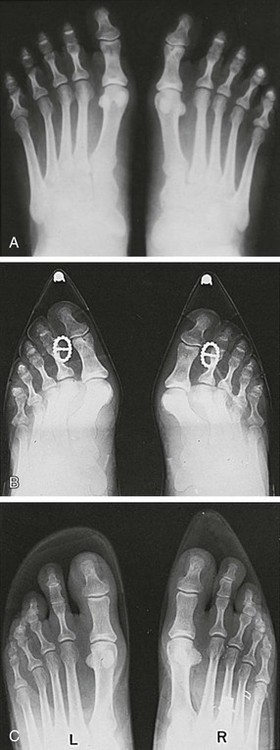
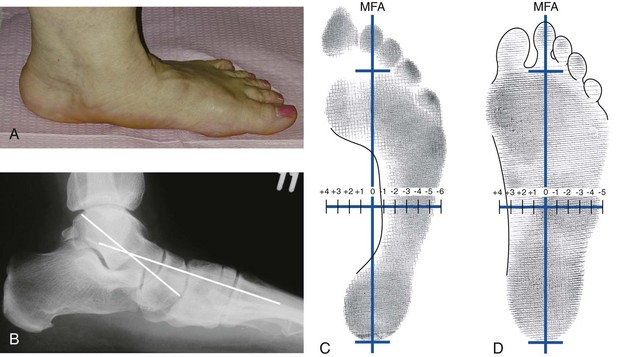
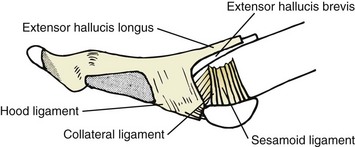
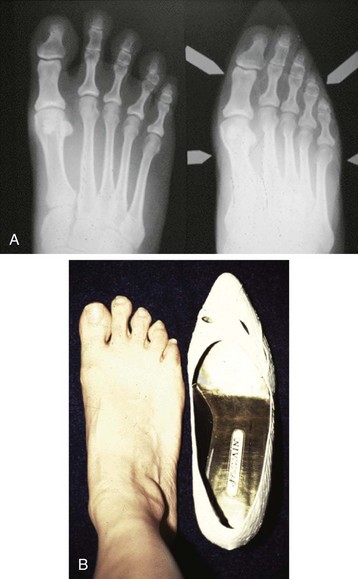
Chapter 6 ANATOMIC AND RADIOGRAPHIC CONSIDERATIONS Metatarsophalangeal Joint Shape Distal Metatarsal Articular Angle and Proximal Articular Set Angle First Metatarsocuneiform Joint Intermetatarsal Facet/Os Intermetatarseum Blood Supply to the First Metatarsal Head Surgical Procedures ( Complications of Hallux Valgus Surgery Complications Affecting the Metatarsal Shaft Complications Affecting the Metatarsal Head Complications Involving the Proximal Phalanx Complications Associated with Capsular Tissue of the First Metatarsophalangeal Joint Recurrent Hallux Valgus Deformity PAIN AROUND THE FIRST METATARSOPHALANGEAL JOINT AFTER BUNION SURGERY The term bunion is derived from the Latin word bunio, meaning turnip, which has led to some confusing misapplications regarding disorders of the first metatarsophalangeal (MTP) joint. The word bunion has been used to denote any enlargement or deformity of the MTP joint, including such diverse diagnoses as an enlarged bursa, overlying ganglion, gouty arthropathy, and hallux valgus, as well as proliferative osseous changes that can develop secondary to MTP joint arthrosis (Fig. 6-1). The term hallux valgus was introduced by Carl Hueter230 to define a static subluxation of the first MTP joint characterized by lateral deviation of the great toe and medial deviation of the first metatarsal. It is now recognized, particularly in juvenile patients, that a hallux valgus deformity can originate because of lateral deviation of the articular surface of the metatarsal head without subluxation of the first MTP joint.97–99 A hallux valgus deformity can also be associated with abnormal foot mechanics, such as a contracted Achilles tendon; severe pes planus; generalized neuromuscular disease, such as cerebral palsy or a cerebrovascular accident (CVA, stroke); or an acquired deformity of the hindfoot secondary to rupture of the posterior tibial tendon. It can likewise be associated with various inflammatory arthritic conditions, such as rheumatoid arthritis (Fig. 6-2). The specialized articulation of the first MTP joint of the great toe differs from that of the lesser toes in that it has a sesamoid mechanism. The head of the first metatarsal is round and covered by cartilage and articulates with the somewhat smaller, concave elliptic base of the proximal phalanx. A fan-shaped ligamentous band originates from the medial and lateral metatarsal epicondyles and constitutes the collateral ligaments of the MTP joint (Fig. 6-3). These ligaments interdigitate with ligaments of the sesamoids. The strong collateral ligaments run distally and plantarward to the base of the proximal phalanx, whereas the sesamoid ligaments fan out plantarward to the margins of the sesamoid and the plantar plate. The two tendons of the flexor hallucis brevis, the abductor and adductor hallucis, the plantar aponeurosis, and the joint capsule condense on the plantar aspect of the MTP joint to form the plantar plate (Fig. 6-4A). Located on the plantar surface of the metatarsal head are two longitudinal cartilage-covered grooves separated by a rounded ridge (the crista). A sesamoid bone is contained in each tendon of the flexor hallucis brevis and articulates by means of cartilage-covered convex facets on its superior surface, with the corresponding longitudinal grooves on the inferior surface of the first metatarsal head. Distally, the two sesamoids are attached by the fibrous plantar plate (sesamoid-phalangeal ligament) to the base of the proximal phalanx; thus the sesamoid complex is attached to the base of the proximal phalanx rather than the metatarsal head. The sesamoids are connected by the intersesamoidal ligament, and this recess conforms to the crista on the plantar surface of the metatarsal head (Fig. 6-4B). The tendons and muscles that move the great toe are arranged around the MTP joint in four groups. The dorsal group is composed of the long and short extensor tendons, which pass dorsally, with the extensor hallucis longus anchored, medially and laterally by the hood ligament (Fig. 6-5). The extensor hallucis brevis inserts beneath the hood ligament into the dorsal aspect of the base of the proximal phalanx. The plantar group contains the long and short flexor tendons, which pass across the plantar surface, with the tendon of the flexor hallucis longus coursing through a centrally located tendon sheath on the plantar aspect of the sesamoid complex. This tendon is firmly anchored by this tunnel within the sesamoid complex. The last two groups are composed of the tendons of the abductor and adductor hallucis, which pass medially and laterally, respectively, but closer to the plantar surface than the dorsal surface. Thus the dorsomedial and dorsolateral aspects of the joint capsule are covered only by the hood ligaments, which maintain alignment of the extensor hallucis longus tendon. Figure 6-5 Collateral ligament structure and extensor mechanism around the first metatarsophalangeal joint. The adductor hallucis, arising from the lesser metatarsal shafts, is made up of two segments, the transverse and the oblique heads, which insert on the plantar lateral aspect of the base of the proximal phalanx and also blend with the plantar plate and the sesamoid complex. The adductor hallucis balances the abductor forces of the abductor hallucis (Fig. 6-6). Acting in a line parallel to this bone and using the head of the first metatarsal as a fulcrum, the abductor hallucis pushes the first metatarsal toward the second metatarsal. The base of the first metatarsal has a mildly sinusoidal articular surface that articulates with the distal articular surface of the first cuneiform. The joint has a slight medial plantar inclination. The medial lateral dimension is approximately half the length of the dorsoplantar dimension. The joint is stabilized by capsular ligaments and is bordered laterally by the proximal aspect of the second metatarsal, which extends more cephalad and offers a stabilizing lateral buttress to the first metatarsocuneiform (MTC) articulation. ElSaid et al,146 in a cadaveric evaluation of 239 specimens, observed a facet to be present in 25% of cases; however, these were not specimens with hallux valgus. Coughlin and Jones101 observed the radiographic presence of a facet between the proximal first and second metatarsals in 7% of 122 cases review with a bunion deformity (Fig. 6-7). The orientation of the MTC joint may determine the amount of metatarsus primus varus, and the shape of the articulation may affect metatarsal mobility. A medial inclination of up to 8 degrees at the MTC joint is normal. Increased obliquity at this joint can increase the degree of metatarsus primus varus. The axis of motion of the MTC joint is aligned to permit motion in a dorsal-medial to plantar-lateral plane. The tarsometatarsal articulation is quite stable in the central portion because of interlocking of the central metatarsals and cuneiforms (Fig. 6-8). This is not necessarily the case for the first and fifth metatarsals, where stability is determined not only by the inherent stability of the tarsometatarsal articulation but also by the surrounding capsular structures. Therefore, when ligamentous laxity is present, the first metatarsal may deviate medially and the fifth metatarsal laterally in the development of a splay foot deformity (Fig. 6-9). Because no muscle inserts on the metatarsal head, it is vulnerable to extrinsic forces, in particular, constricting footwear. Once the metatarsal becomes destabilized and begins to subluxate medially, the tendons about the MTP joint drift laterally. The muscles that previously acted to stabilize the joint become deforming forces because their pull is lateral to the longitudinal axis of the first ray. The plantar aponeurosis and the windlass mechanism contribute significantly to stabilization of the first ray450,460; with progression of a hallux valgus deformity, their stabilizing influence is diminished (Fig. 6-10).102,190 As the hallux valgus deformity progresses, the soft tissues on the lateral aspect of the first MTP joint become contracted, and those on the medial aspect become attenuated. The metatarsal head is pushed in a medial direction by the lateral deviation of the proximal phalanx, thereby progressively exposing the sesamoids, which are anchored in place by the transverse metatarsal ligament and the adductor hallucis muscle. As the metatarsal head continues to deviate medially off the sesamoids, the crista, which normally acts to stabilize the sesamoids, is gradually eroded (see Fig. 6-1F and G).35,449,496 These lesions are rarely seen on the plantar surface of the first metatarsal unless an effort is made intraoperatively to inspect this area. Bock et al35 reported on a large series of patients treat for hallux valgus, and found that 57% had significant plantar erosive lesions. Roukis et al,449 reporting on 166 feet that underwent bunion surgery, noted that almost every joint had some element of articular cartilage erosion on the plantar metatarsal head. In more severe deformities, this erosion becomes more pronounced and extensive.35,449 As the sesamoid sling slides beneath the first metatarsal head, the hallux gradually pronates. As this dynamic joint deformity occurs, the medial eminence often becomes more prominent (Fig. 6-11). The hallux and the first MTP joint play a significant role in the transfer of weight-bearing forces during locomotion. The plantar aponeurosis also plays a key role in this process by plantar flexing the first metatarsal as weight is transferred to the hallux. As the hallux is dorsiflexed at the first MTP joint, the first metatarsal is depressed, which results in increased weight bearing beneath the first metatarsal head and stabilization of the medial longitudinal arch (Fig. 6-12). Certain pathologic conditions, either acquired or iatrogenic, diminish the ability of the first MTP joint and hallux to function as weight-bearing structures. This results in transfer of weight to the lateral aspect of the forefoot, which often leads to the development of a transfer lesion beneath the second or third metatarsal head. As less weight is borne by the first ray, transfer metatarsalgia and lesser toe deformities may develop. Coughlin and Jones100 reported a 48% incidence of second MTP joint symptoms in a prospective study of adult patients undergoing repair of moderate and severe hallux valgus deformity. The dynamics of the hallux valgus deformity can best be understood by first examining the articulation where the deformity occurs, that is, the MTP and MTC joints. The most stable MTP articulation has a flat articular surface, and conversely, the most unstable has a rounded head (Fig. 6-13).88,139,155,336 Coughlin and Jones101 noted this in 71% of patients in a large series of cases of hallux valgus they examined. Okuda et al394 also observed an increased incidence of a rounded first metatarsal head associated with hallux valgus. A congruent MTP joint likewise is more stable than an incongruent or subluxated joint. A congruent joint tends to remain stable, whereas once a joint has begun to subluxate, the deformity tends to progress with the passing of time (Fig. 6-14). In some circumstances, alignment of the first MTP joint is normal but a valgus deformity is present because of a deformity within the proximal phalanx, and a hallux valgus interphalangeus (HVI) deformity results (Fig. 6-15). With an incongruent or subluxated hallux valgus deformity, there is usually a progressive deformity. As the proximal phalanx moves laterally on the metatarsal head, it exerts pressure against the metatarsal head, which pushes it medially and results in an increased IM angle. As this process occurs, there is progressive attenuation of the medial joint capsule, as well as a progressive contracture of the lateral joint capsule (Figs. 6-16 and 6-17). While this deformity is occurring, the sesamoid sling, which is anchored laterally by the insertion of the adductor hallucis muscle and the transverse metatarsal ligament, remains in place as the metatarsal head moves medially and thereby creates pressure on the medial joint capsule. The weakest portion of the medial joint capsule lies just above the abductor hallucis tendon, and with chronic pressure, this portion of the capsule gives way; as a result, the abductor hallucis muscle gradually slides beneath the medially deviating metatarsal head. As this process slowly progresses, atrophy of the crista occurs beneath the first metatarsal head, which normally helps stabilize the sesamoids (Fig. 6-18). Once the abductor hallucis slides beneath the first metatarsal head, two events occur. First, the intrinsic muscles no longer act to stabilize the MTP joint but actually help enhance the deformity. Second, as the abductor hallucis rotates beneath the metatarsal head, because it is connected to the proximal phalanx, it will spin the proximal phalanx around on its long axis and give rise to varying degrees of pronation (Fig. 6-19). It has been well established that as the hallux valgus deformity progresses, so does the degree of pronation.336,344 In rare circumstances, if the progressive deformity of the MTP joint continues unabated, dislocation of the MTP joint may occur over time, with the fibular and tibial sesamoids becoming dislocated into the first IM space (Fig. 6-20). Normally, a small eminence is present on the medial aspect of the first metatarsal head. The size of the medial eminence varies, and sometimes most of the enlargement is on the dorsomedial aspect of the head and is thus not apparent on anteroposterior (AP) radiographs. Volkman540 and Truslow527 both suggested that new bone formation occurred with bunion formation, whereas Lane293 and Haines and McDougall200 suggested that merely a segment of the first metatrsal head had become exposed with lateral deviation of the hallux. Thordarson and Krewer515 and Coughlin and Jones101 have both demonstrated that the size of the medial eminence was similar in subjects with and without bunions, and the authors concluded that bony proliferation was not a component of bunion formation. The overall width of the distal metatarsal head does not enlarge with progression of a hallux valgus deformity. Thordarson and Krewer reported an average width of the medial eminence of 4.4 mm, whereas Coughlin and Jones101 reported the mean width to be 4.6 mm in subjects with bunions (Fig. 6-21). The medial eminence develops with lateral migration of the proximal phalanx, but it is not characterized by new bone formation or hypertrophy of the medial first metatarsal head. As the hallux valgus deformity develops, progressive medial deviation of the metatarsal head occurs and becomes symptomatic because of pressure against the shoe. Individuals who wear a broad, soft shoe or sandal are not usually bothered by the enlarged medial eminence, in contrast to persons who wear dress or high-heeled shoes. At times, an inflamed or thickened bursa may aggravate the problem. On rare occasions and usually in older patients, the skin over the medial eminence can break down and result in a draining sinus. On other occasions, a ganglion arising from the medial side of the joint can erode the joint capsule and make the eventual hallux valgus repair technically much more difficult (see Fig. 6-1D). The splayed appearance of the forefoot in more severe cases of hallux valgus (see Fig. 6-9) occurs primarily because the first metatarsal head is no longer contained within the sesamoid sling and is displaced in a medially deviated position. The middle metatarsals do not splay because of the stable articulation at their tarsometatarsal joints. On occasion, the fifth metatarsal lacks stability and drifts laterally, thereby completing the appearance of a splayed foot. Piggott414 reported on a series of adult patients evaluated for hallux valgus deformities. Fifty-seven percent of the patients interviewed recalled an onset of the deformity during their adolescent years, whereas only 5% recalled development of the bunion deformity after 20 years of age. In a long-term review of patients with hallux valgus deformities, Hardy and Clapham208 reported that 46% of bunion deformities occurred before the age of 20. Although Scranton471 stated that a hallux valgus deformity rarely develops before 10 years of age, Coughlin95 reported on a series of juvenile patients with bunions in whom the average age at onset was 12 years; 40% of these patients noted that the onset of their deformity occurred at the age of 10 years or younger. Thus development probably occurs much earlier than has previously been appreciated.* In contrast, Coughlin91 reported onset by decade in a group of men and noted that 21 of 34 (62%) patients dated the development of their bunion to the third to fifth decade of life. Only 7 of 34 (20%) recalled onset in the adolescent years. Later, Coughlin and Jones101 stated that 65% of adults reported the onset of their deformity in the third through fifth decades and only 4% in the first decade. Although the onset of hallux valgus indeed peaked during the third decade, the incidence of occurrence was almost equal throughout the second through fifth decades. There was not relationship between the severity of the deformity and the decade of onset. At what age a patient recognizes a hallux valgus deformity is obviously dependent on understanding the deformity, the symptoms, magnitude of the deformity, family history, and keenness of a patient’s observation skills. Many deformities can begin in the adolescent years but progress in magnitude in later decades when they become more symptomatic. The date when surgery was performed should not be confused with the age at onset. Coughlin and Jones101 noted that although patients recalled the onset of their bunion deformity at a mean age of 31 years, the average age at which surgery was performed was 50 years. Increasing age was not associated with increasing magnitude of angular deformity. In a retrospective study, Coughlin and Thompson112 reviewed more than 800 cases and reported the mean age at surgery to be 60 years. Of importance is the fact that late development after skeletal maturity occurs in a foot that at one point most likely had a normal structure, whereas an early onset in the juvenile years occurs before maturation in a foot that most likely “never had a normal structure.” Coughlin95 observed, in a series of patients with juvenile hallux valgus, that early onset of hallux valgus (before 10 years of age) was associated with a much higher distal metatarsal articular angle (DMAA), a finding that would probably alter the choice of operative technique in these patients. Although several studies have provided statistical data showing some predilection in the female population for the development of hallux valgus, this may be merely a reflection of a specific person’s choice of footwear. Wilkins,552 in a study of schoolchildren’s feet, reported a female preponderance of 2 : 1. Hewitt et al221 and Marwil and Brantingham,350 in investigating male and female military recruits, found a predilection of approximately 3 : 1 in the female population. Creer114 and Hardy and Clapham,207 in reporting statistics from their surgical practices, found this ratio to be approximately 15 : 1 in adult patients. The reported incidence of females in the juvenile population undergoing surgical correction for hallux valgus deformities varies from 84% to 100%.* Several studies on adult patients report females make up 90% or more of the patient population.† Coughlin and Jones101 found that the proportion of females in their report on moderate and severe hallux valgus deformities was 92% (P < .01). Certainly, shoes worn by women are generally less physiologic than those worn by men, and shoes of any type can lead to hallux valgus in susceptible persons; however, it is also likely that heredity plays a substantial role in the development of bunion deformities (Fig. 6-22). On the contrary, Akinbo et al,3 in a study of young Nigerians, reported close to equal female (56%) and male (44%) involvement in an adolescent population. Pique-Vidal et al419 observed that gender did not effect the severity of the angular deformity. Pique-Vidal419 did not note an association between gender and severity of deformity in his series of 350 subjects. Figure 6-22 A, Normal foot on the left, foot in a fashionable shoe on the right. B, Photograph of the foot and shoe. The authors previously believed that hallux valgus deformities commonly occurred as unilateral deformities.339 This notion was based on reports of the results of surgical procedures in which a majority of patients underwent unilateral surgery.* However, this information does not truly document the incidence of bilaterality. Patients may have bilateral deformities yet have surgery performed on only one side. They may undergo bilateral surgery yet have only the index surgery performed during the period of study. Even though many reports cite unilateral occurrence, the author’s prospective evaluation of moderate and severe hallux valgus deformities demonstrated that although 84% of patients had bilateral hallux valgus deformities, only 18% had both feet corrected during the study period.101 The remaining surgery occurred either before or after the reported study. There was no association between bilateral deformities and handedness, family history, or the magnitude of the preoperative deformity. There was a strong correlation between bilateralism and a family history of bunions (P < .01). Symptoms and varying magnitudes of deformity may lead a person to desire unilateral correction despite having bilateral hallux valgus deformities. The authors believe that the majority of patients have bilateral hallux valgus deformities of differing magnitude. Ninety percent of the population is right handed,550 but how this translates to foot dominance is unknown.549 Coughlin and Jones101 reported that 91% of patients who underwent bunion surgery were right handed and were unable to find a correlation between handedness and foot side involved, age of onset, or severity of the hallux valgus deformity. Although most series report the number of right and left feet involved, it is unknown whether handedness makes a difference in development of the deformity. Myerson384 has suggested that hallux valgus deformities develop in 2% to 4% of the population. Although no published study has reported the frequency of development or the rate of surgical correction of hallux valgus deformities in the United States, Coughlin and Thompson112,513 estimated that more than 200,000 hallux valgus corrections are performed in the United States each year. This figure is probably an underestimate of both the incidence of the deformity and the frequency of surgical correction. Hallux valgus occurs almost exclusively in persons who wear shoes but does occasionally occur in unshod people (Fig. 6-23). The notion of footwear being the principal contributor to the development of hallux valgus was substantiated by a study of Sim-Fook and Hodgson487 in which 33% of shod persons had some degree of hallux valgus as compared with 2% of unshod persons. Owoeye et al3,398 reported a very low incidence of hallux valgus in Nigerian youth in a typically unshod population. Hallux valgus deformities were also extremely rare in the Japanese because of the nature of their traditional footwear, the tabi sandal (Fig. 6-24). When the manufacture of fashionable leather shoes greatly exceeded the manufacture of traditional sandals in the 1970s, the incidence of hallux valgus deformity increased substantially.259 Conversely, physicians in France referred to the development of hallux valgus deformities as early as the 18th century. Before that time, the common footwear was a Greco-Roman style, flat-soled sandal. Studies by Maclennan322 in New Guinea, Wells547 in South Africa, Barnicot and Hardy21 in West Africa, Engle and Morton148 in the Belgian Congo, and James239 in the Solomon Islands found some element of metatarsus primus varus and an occasional asymptomatic hallux valgus deformity in the indigenous populations (Fig. 6-25). Cho et al67 has reported in a study from a rural Korean community, that female subject in the fourth through seventh decades had a higher incidence of deformity. Figure 6-25 Kenyan tribesman with an asymptomatic hallux valgus deformity. (Courtesy J.J. Coughlin, MD.) One can conclude from these studies that an asymptomatic hallux valgus deformity in an unshod person may be attributed to hereditary causes. In shoe-wearing populations, however, a symptomatic and painful bunion would be expected to develop more commonly.113,221 A wide or splayed forefoot forced into a constricting shoe might thus lead to symptoms over the medial eminence. Although shoes appear to be an essential extrinsic factor in the development of hallux valgus, the deformity does not develop in many people who wear fashionable footwear. Therefore some intrinsic predisposing factors must make some feet more vulnerable to the effect of footwear and likewise predispose some unshod feet to the development of hallux valgus. Although high-fashion footwear has been implicated in the progression of hallux valgus deformities in adults,* Hardy and Clapham207 and others95,249 have suggested that in most cases a juvenile hallux valgus deformity does not appear to be influenced by a history of constricting footwear. Poorly fitting shoes play a small role in juvenile hallux valgus. In a prospective study of adults with hallux valgus, Coughlin and Jones101 reported that only 34% of patients undergoing surgical correction implicated constricting footwear as a cause of their deformity. In an earlier report, Coughlin91 found that 60% of men with hallux valgus who had undergone surgical correction implicated ill-fitting shoes as a cause of their deformity. Cathcart62 and Creer114 have implicated occupation as a cause of hallux valgus. Again, objective evidence in the small percentage of patients who claim that their occupation contributed to their hallux valgus deformity is lacking. Coughlin and Jones101 reported that patients considered occupation an infrequent cause of their deformity, with 17% implicating their job as a cause of their hallux valgus deformity. However, there was not a correlation between the magnitude of the angular deformity and those who attributed their deformity to either occupation or constricting shoewear. Trauma to the forefoot may be a cause of acute deformity or chronic deviation to the MTP joint. Rupture of the medial joint capsule has been recognized as a cause leading to development of a bunion deformity.151 Johal et al241 reported a bunion deformity that followed a tibial shaft fracture with entrapment and injury to the medial plantar nerve. Bohay et al37 reported seven cases in which a Lisfranc joint injury led to first MTC joint instability and later bunion deformity. Surgical correction with a standard bunion correction in several of these cases led to realignment of the first ray. The notion that a hallux valgus deformity is inherited has indeed been suggested by many authors.* A positive family history of hallux valgus in 58% to 88% has been reported in five different series of adult patients.73,184,207,370,427 Coughlin and Jones101 stated that 86 of 103 adult patients (84%) reported a family history (parents, grandpartents) of hallux valgus deformities. In 1956, Johnston248 reported an in-depth genetic history on subjects with hallux valgus. Based on a single-family case report, he proposed that this trait was autosomal dominant with incomplete penetrance. Juvenile hallux valgus deformities have been characterized by their familial tendency. Coughlin95 reported a family history in 72% of patients in his retrospective study on juveniles and noted that a bunion was identified in 94% of 31 mothers of children with a family history of hallux valgus deformity. Of the 31 patients with a positive family history for the deformity, four females noted an unbroken four-generation history of hallux valgus transmission from maternal great-grandmother to maternal grandmother to mother to patient (Fig. 6-26). Eleven females reported a three-generation history of transmission from maternal grandmother to mother to patient, and 11 patients noted a two-generation history of mother-to-patient transmission. Of three males with hallux valgus in this same series, two reported their mothers to have had a bunion and one reported a three-generation history of maternal transmission to the patient. Thus 29 of 31 patients (94%) with a family history showed a pattern consistent with maternal transmission. The preoperative hallux valgus deformity in these patients was reported to be 5 degrees greater in those with a family history, although the average postoperative hallux valgus correction was similar in patients with and without a family history. Pique-Vidal et al,419 in a report of 350 patients with hallux valgus, constructed a three-generation pedigree. The gender ratio was male : female 1 : 15; juveniles comprised only 5% of the series. Ninety percent of the subjects had at least one other relative with a bunion; 70% of the subjects had at least three relatives with bunion involvement. The authors also observed that severity of the deformity was not affected by gender or the magnitude of deformity in other relatives. Both Bonney and Macnab38 and Coughlin95 observed an earlier onset of deformity in patients with a family history of hallux valgus. The high rate of maternal transmission noted in previous reports95,207 makes it difficult to avoid a conclusion that there is a genetic predisposition for hallux valgus deformities in the female population. However, the chapter authors believe that although this trait can be associated with X-linked dominant transmission or polygenic transmission, it more commonly is an autosomal dominant transmission with incomplete penetrance.95,419 The association of pes planus with the development of a hallux valgus deformity is controversial. A low incidence of advanced pes planus in adults with hallux valgus led Mann and Coughlin to conclude that the occurrence of hallux valgus with pes planus is uncommon in patients without neuromuscular disorders.336 The incidence of pes planus in the general population was defined in a review of normal adult military recruits by Harris and Beath.210 They reported a 20% incidence of pes planus. Half of these cases represented an asymptomatic “simple depression of the longitudinal arch.” In general, pes planus may be no more common in those with hallux valgus than in the general population.* Pouliart et al427 did not observe any relationship between the degree of pes planus and the severity of hallux valgus. Kilmartin and Wallace272 found that the incidence of pes planus in the normal population and in those with a hallux valgus deformity was essentially the same. They concluded that pes planus in juveniles had no significant association either with the magnitude of the preoperative hallux valgus deformity or with the postoperative success or failure rate of a surgical repair. This finding was confirmed by Coughlin95 and Trott,526 and McCluney and Tinley,359 who all noted no increased incidence of pes planus in juvenile patients. Studies by Canale et al,58 Coughlin95 and Kilmartin and Wallace272 have reported no correlation between pes planus and the success rate of surgical repair of a hallux valgus deformity. Coughlin and Jones100,101 reported a 15% incidence of moderate and severe pes planus in their surgical series of 122 feet with hallux valgus. Arch height has been quantified by both Harris mat imprints and radiographic measurements (Fig. 6-27).103,110 Coughlin and Kaz103 reported good correlation between Harris mat imprints and physical examination and angular measurements, such as the lateral talometatarsal angle, lateral talocalcaneal angle, calcaneal pitch, and the AP taolnavicular angle. Grebing and Coughlin192 used Harris mat imprints to assess arch height and demonstrated that a low arch was significantly more common in an adult group with hallux valgus than in a control group. They reported an 11% incidence of pes planus in a normal control group and a 24% incidence in a group with hallux valgus but also found no correlation between the hallux valgus angle and pes planus or between pes planus and first-ray mobility. Saragas and Becker459 did not find an increased incidence of pes planus when they examined the calcaneal pitch angle and found no association between the degree of pes planus and the severity of hallux valgus deformity. King and Toolan275 observed an association between the hallux valgus angle and both the Meary line (lateral talometatarsal angle) and the AP talonavicular coverage angle in those with pes planus. Other authors have suggested that a hallux valgus deformity tends to develop in a pronated foot.* Hohmann225 was the most definitive and asserted that hallux valgus was always associated with pes planus and that pes planus is always a causative factor in hallux valgus. In attempting to resolve this contradiction, the chapter authors believe that a patient with a pes planus deformity in whom hallux valgus develops will have more rapid progression of the deformity. However, hallux valgus does not develop in most patients with pes planus. Models and radiographs can demonstrate the role of pronation in the pathophysiology of hallux valgus in a normal foot (Figs. 6-28 to 6-31). Although an excellent demonstration of the effect of pronation on the foot and hallux. They do not enable determination of what initiates a hallux valgus deformity. In Figure 6-28, a pendulum has been attached to the nail of the great toe. As the foot is pronated, rotation of the first ray around its longitudinal axis is clearly seen. In Figure 6-29, a skeletal model has been photographed. With longitudinal rotation of the first metatarsal head, the fibular sesamoid becomes visible on the lateral side of the first metatarsal head. Figure 6-30 shows a dorsoplantar weight-bearing radiograph; with the pronated position of the sesamoids, they appear to have been displaced laterally. The fibular sesamoid is now visible in the interval between the first and second metatarsals, as would be anticipated from the skeletal model in Figure 6-31. Tangential or sesamoid views of the foot show that this appearance is caused solely by longitudinal rotation of the first metatarsal, not by actual lateral displacement; the sesamoids remain in a normal relationship with their facets located on the plantar surface of the metatarsal head (see Fig. 6-31).
Hallux Valgus
![]() Video Clips 33-36 and 52-62)
Video Clips 33-36 and 52-62)
Overview
Anatomy
Pathoanatomy
Pathophysiology
Demographics
Age of Onset
Gender
Bilaterality
Handedness
Frequency of Occurrence
Etiology
Extrinsic Causes
Footwear

Occupation
Trauma
Intrinsic Causes
Heredity
Pes Planus
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Hallux Valgus