13 Guidelines for Exercise after Stroke service design
Introduction
The growing evidence of the benefits of Exercise after Stroke and its incorporation into UK and international clinical guidelines and policy (e.g. Gordon et al. 2004, Royal College of Physicians 2008, Scottish Government 2009, Scottish Intercollegiate Guidelines Network 2008, 2010) means there is a strong impetus for new Exercise after Stroke service development. For this reason, it is timely to provide some direction as to how service development should progress, based on existing research evidence, clinical and occupational standards and professional experience.
Firstly, we will clarify the scope of the best practice guidance in terms of where the Exercise after Stroke services are placed in the stroke pathway, the range of services covered and the target audience for these guidelines. Then we will outline the key best practice elements of Exercise after Stroke. The best practice guidelines are based on in-depth analysis of the content and organisation of existing services in Scotland (Best et al. 2010a, 2011), current research evidence in this field, plus relevant stroke and exercise guidelines and National Occupational Standards in the UK health and fitness sector (SkillsActive 2010a,b). The full text of the guidelines, full details of the multiprofessional team who wrote the full guidelines and further background details can be found at www.exerciseafterstroke.org.uk.
Scope of the Guidelines
Exercise after Stroke Services in the Patient Journey
There are three key elements of stroke care, as described in chapter 2:
1. Acute treatment: medical care immediately following stroke.
2. Rehabilitation: restoration of function and minimisation of long-term disability after stroke.
3. Secondary prevention: preventing further strokes through medication and lifestyle advice.
Rehabilitation after stroke is very important for maximising quality of life and independence after stroke. Normally, a multidisciplinary team of professionals is involved in providing post-stroke rehabilitation. However, due to resource issues, rehabilitation is generally time-limited, and the majority of patients will eventually come to a stage where the focus of care shifts from professional input to self-management. As highlighted in chapter 5, research has shown that exercise has a vital role to play in improving and maintaining physical fitness and function after stroke (Brazzelli et al. 2011, Saunders et al. 2009, English and Hillier 2010). Exercise is, therefore, an important way in which stroke survivors can continue to improve their own fitness and function after, or in addition to, formal rehabilitation (Mead and van Wijck 2011). Exercise reduces the risk of first-ever stroke and can also potentially play an important role in secondary stroke prevention; although there are no data linking exercise with the risk of recurrent stroke, there is evidence that exercise has important biological effects that are likely to reduce recurrent stroke, e.g. stimulation of endogenous fibrinolysis (Ivey et al. 2003). This chapter describes how to provide services in the community that support safe, effective exercise after stroke.
Exercise after Stroke Services
The Exercise after Stroke services described here are community services, which means they are for people who are not inpatients in a hospital. Although clinical guidelines recommend that exercise be incorporated into the early management of stroke, there are challenges to engaging inpatients in exercise. For example, medical complications such as infection are common in the early post-stroke period, as is fatigue (Morley et al. 2005). Ongoing research will, however, provide further evidence about the feasibility, safety and effectiveness of exercise training during inpatient rehabilitation. These guidelines focus on delivery of community Exercise after Stroke services that could be accessed by stroke survivors once they are discharged from hospital.
Best Practice Guidelines for Exercise after Stroke
Readers are referred to the ‘Best practice guidance for the development of Exercise after Stroke services in community settings’ (Best et al. 2010b) for the full guidelines. This chapter describes the key requirements for best practice for Exercise after Stroke; these are listed in Box 13.1. Each of these elements will be detailed below.
Box 13.1 Key requirements for best practice for Exercise after Stroke services
Service Governance and Management
Working group
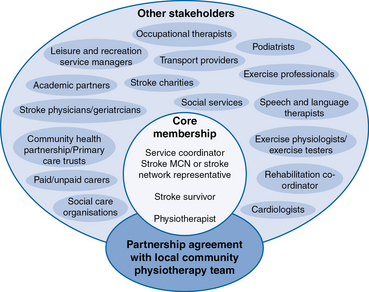
Although many of the existing Exercise after Stroke services in the UK are led by a single organisation, for optimum delivery all organisations and professional groups involved in delivering stroke services should be involved in the planning of Exercise after Stroke services. In this way, the service would benefit from the perspective of all these different stakeholders (e.g. medical knowledge, experience of delivering as well as participating in community services). Figure 13.1 indicates the possible membership of the working group. The diagram shows the ‘core’ or minimum membership in the centre circle and the large oval indicating the other professionals that would ideally also be involved, such as these would include all local stakeholders in stroke service provision, including doctors, physiotherapists, specialist stroke and practice nurses, occupational therapists, speech and language therapists, orthotists, podiatrists, exercise professionals, health, leisure and voluntary sector service managers, social services, transport providers and service users, including stroke survivors and carers.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree