Chapter 23 Growth and Development
Knowledge of normal as well as abnormal patterns of growth and development enables the physician to assist the child in maximizing his or her fullest potential. Growth in height and weight is a sensitive reflection of a child’s general health. Deviations from normal can reflect the presence of physical illness or a disturbance in the child’s environment. Box 23-1 lists some significant causes of growth abnormalities.
Box 23-1 Significant Causes of Growth Abnormalities in Children
Care of Children in Family Medicine
Family physicians have the opportunity to provide family-centered pediatric care in the context of the child’s family and community. The office should be “child friendly” and child safe with at least one room equipped to evaluate the child’s physical growth. Blood pressure cuffs should be available to measure a child’s blood pressure, at least from age 36 months and older. Electrical outlets and cords should be secured and potentially hazardous chemicals and biohazard bins stored either out of reach or under lock and key from curious young toddlers. Guidelines for the frequency of “well child” or “well teen” visits are available from the American Academy of Pediatrics (AAP) Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents (Hagan et al., 2008).
Blood Pressure Monitoring
Hypertension has become increasingly common in children and adolescents. Since 1988, the prevalence of high blood pressure has increased, especially for certain populations, such as Mexican-Americans and blacks (Din-Dzietham et al., 2007). The rising rate of obesity, particularly truncal obesity, at least partly accounts for this. Because of potential end-organ damage and cardiovascular risk in adulthood, auscultatory monitoring of blood pressure (BP) is recommended during health care visits for all children 3 years and older and for younger children with certain high-risk features (Box 23-2). Automatic devices may be needed to measure BP in young infants. Elevated BP should be confirmed on repeat visits. The guidelines define hypertension as average systolic or diastolic BP of 95% or higher for gender, age, and height on three or more occasions. Prehypertension is defined as values of 90% or greater and less than 95%. For adolescents, BP greater than or equal to 120/80 mm Hg but less than 95% is defined as prehypertensive. Because of the inclusion of a diverse population, these guidelines and tables appear applicable to all ethnic groups (see eTables 23-1 and 23-2 online at www.expertconsult.com).
Box 23-2 Indications for Blood Pressure (BP) Measurement in Children Under 3 Years Old
Data from National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents: The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Pediatrics 2004;114:555-576.
The approach to confirmed hypertension in children should be individualized and should consider variables such as comorbidities and family history. In overweight or obese children, the possibility of metabolic syndrome should be investigated. Lifestyle changes, including diet and exercise, may be sufficient for overweight children with stage 1 hypertension (BP at 95% to 99% plus 5 mm Hg). Children with stage 2 hypertension (BP >99% plus 5 mm Hg) and those with end-organ damage likely require medical therapy (National High Blood Pressure Education Program Working Group, 2004).
Measuring Physical Parameters of Growth
Proper Use and Interpretation of Growth Charts
Although careful measuring and plotting of growth parameters is the most accurate method by which to follow a child’s physical growth, approximate growth guidelines are helpful to the physician in remembering and forming an overall impression of the child’s progress (Table 23-1).
Table 23-1 Approximate Growth Guidelines for Children
| Age | Length or Height (ht) | Weight (wt) |
|---|---|---|
| Newborn | 50 cm (20 inches) average | 3.4 kg (7.5 pounds) average |
| Newborn to 3 months | — | 1 kg/month (1 oz/day) average wt gain |
| 3-12 months | — | |
| 12 months | 75 cm (30 in) average | Triples birth weight |
| 12-24 months | Increases by >10 cm/yr | 0.25 kg/month |
| >5 years | >5 cm (2 in)/yr until adolescent growth spurt | 2.3 kg (5 lb)/yr until adolescent growth spurt |
| 2-12 years | ||
| Puberty | 8-14 cm/yr |
∗ Modified from Needleman RD. The first year. In Behrman RE, Kliegman RM, Jenson HB (eds). Nelson Textbook of Pediatrics, 17th ed. Philadelphia, Saunders, 2004, p 31.
Familial Short Stature and Constitutional Growth Delay
Each child has a different rate of maturation, or what Boas termed “tempo of growth” (Tanner, 1986). Persons with short stature are more than 2 standard deviations (SD) below the mean in height and constitute approximately 2.5% of children (Miller and Zimmerman, 2004). If a child’s growth falls outside the range of normal, it is useful to obtain a bone-age radiograph, usually of the left hand and wrist, and compare it to age-specific standards. Children must be at least 2 years of age to reliably identify epiphyseal ossification centers. Box 23-3 lists some causes of retarded or accelerated bone age. Calculation of mean predicted adult height is also useful in determining whether a child is fulfilling her or his genetic potential. The mean predicted adult height is calculated as follows (Rogol, 2004):
Box 23-3 Causes of Short Stature and Relationship to Bone Age and Growth Rate
Pubertal Growth and Development
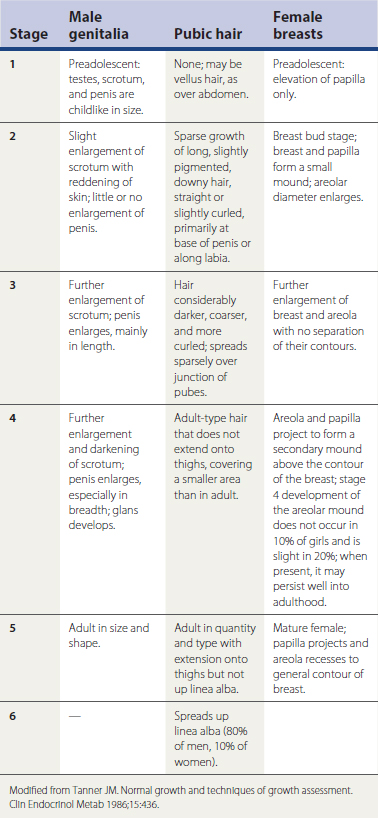
All children grow at a different tempo, with some maturing earlier than others and some later. This difference is most apparent during puberty. The NCHS growth charts now extend to age 20 years. Tanner and Davies (1985) took the earlier NCHS data and constructed height and weight velocity curves for American boys and girls that account for those groups who mature earlier and later. These charts also allow for notation of the various stages of puberty described by Tanner (1986) (Table 23-2).
The adolescent growth spurt in skeletal and body dimensions is associated closely with the development of the reproductive system. Although the onset and rate of maturation vary according to the individual, the sequence is usually the same within genders (Figs. 23-1 and 23-2). Girls who demonstrate signs of puberty before 7 to 8 years of age and boys who show signs before 9 years should be evaluated for precocious puberty. Conversely, girls who do not show signs of puberty by age 13 and boys by age 14 should be evaluated for pubertal delay (Plotnick, 1999).
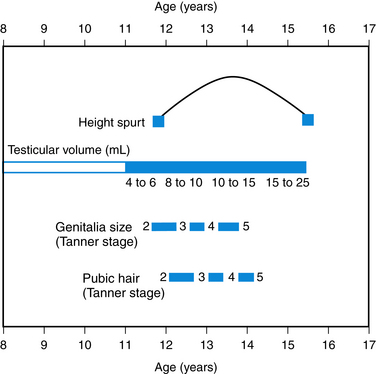
Figure 23-1 Sequence of pubertal events in average American boys.
(Modified from Brookman RR, Rauh JL, Morrison JA, et al: The Princeton Maturation Study; 1976, unpublished data for adolescents in Cincinnati, Ohio. In Copeland KC, Brookman RR, Rauh JL [eds]: Assessment of Pubertal Development. Columbus, Ohio, Ross Products Division, Abbott Laboratories, 1986, p 4.)
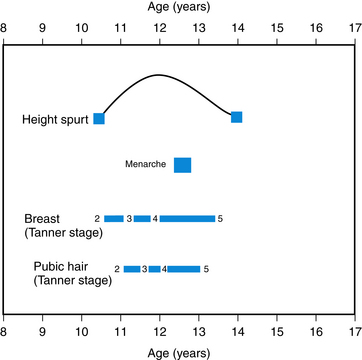
Figure 23-2 Sequence of pubertal events in average American girls.
(Modified from Brookman RR, Rauh JL, Morrison JA, et al: The Princeton Maturation Study, 1976 unpublished data for adolescents in Cincinnati, Ohio. In Copeland KC, Brookman RR, Rauh JL [eds]: Assessment of Pubertal Development. Columbus, Ohio, Ross Products Division, Abbott Laboratories, 1986, p 4.)
Screening Healthy Children
Preventive care services for children often include screening for health conditions in which early detection and early treatment can prevent or ameliorate more serious disease in the future. Screening tests should detect most persons with the condition (sensitivity) while excluding most persons who do not have the condition (specificity) in a cost-effective manner. In an inner-city Medicaid population, high continuity of care in infancy was associated with improved screening for anemia, lead, and tuberculosis (Flores et al., 2008).
Hearing and Vision Screening
Early detection and intervention for hearing and vision deficits are important for maximal long-term functioning. Without appropriate opportunities to learn language, children with significant hearing deficits fall behind peers in terms of communication, cognition, reading, and social-emotional development, with long-term effects on educational attainment and adult employment (AAP Joint Committee on Infant Hearing, 2007). It is now recommended that all infants be screened for hearing loss by 1 month of age, regardless of risk factors. Those who do not pass the screening should have a complete audiologic evaluation by 3 months of age, and those with confirmed hearing loss should receive appropriate treatment by 6 months to ensure optimal outcome. Regardless of the outcome of newborn screening, ongoing surveillance of hearing status is recommended. Developmental delays and other risk factors (Box 23-4), particularly in language, as well as the presence of parental concern about hearing, should prompt referral for a complete audiologic evaluation, even if the newborn screen was normal and there are no risk factors for hearing impairment (Hagan et al., 2008). Gradations of hearing loss are presented in Table 23-3.
Box 23-4 Risk Factors for Delayed Onset of Hearing Loss in Young Children
Modified from Hagan JF, Shaw JS, Duncan PM (eds). Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents, 3rd ed. Elk Grove Village, Ill, American Academy of Pediatrics, 2008, p 232.
| Hearing impairment | Hearing threshold (dB) |
|---|---|
| None | 10-25 |
| Mild | 26-40 |
| Moderate | 41-55 |
| Moderate to severe | 56-70 |
| Severe | 71-90 |
| Profound | >91 |
Eyesight evaluation is a recommended part of routine health maintenance examinations in children beginning in the newborn period. In young children (<3 years) the evaluation, besides the actual eye examination, is somewhat subjective and based on parental history. Children with risk factors, such as prematurity, family history of retinoblastoma or glaucoma, or significant developmental delays or neurologic difficulties, should be referred to an experienced pediatric ophthalmologist. More formal testing of visual acuity should begin at age 3 years, using standardized systems such as the Allen Cards, which have easily recognized pictures (AAP Committee on Practice and Ambulatory Medicine, 2003). Normal visual acuity is in the 20/30 to 20/40 range for children 3 to 4 years old, but increases to 20/20 by early school age. Eye-specific screening should be attempted in an effort to detect amblyopia (more than one line difference on the chart) (SOR: B). The suspicion of amblyopia or strabismus requires further evaluation to prevent long-term visual loss (AAP Committee on Practice and Ambulatory Medicine, 1996). Routine screening should be done at least through early school age, at puberty and whenever there are other signs, such as squinting or complaints of inability to see the board at school (Hagan et al., 2008).
Screening for Lead Toxicity
Lead is neurotoxic and affects both intellectual and behavioral function, even below the 10 μg/dL level established by the U.S. Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO) (Canfield et al., 2003). Federal Medicaid law has required lead screening of young children eligible for Medicaid at ages 12 months and 24 months, and for children ages 36 to 72 months not previously tested. However, 1999−2004 NHANES data demonstrate that the percentage of children with blood lead levels of 10 μg/dL or higher had decreased to 3.4% for black and 1.2% for white children age 1 to 5 years. The USPSTF finds insufficient evidence to recommend for or against screening asymptomatic children 1 to 5 years old who are at increased risk. The CDC recommends targeted screening of specific groups of children, except in areas where universal screening is still recommended because of a prevalence of elevated lead levels. Specific state information can be obtained at http://www.cdc.gov/nceh/lead. Children considered at risk who require screening include (1) those suspected by a parent or health care provider to be at risk for exposure; (2) those with a sibling or frequent playmate with an elevated blood lead level; (3) those with a parent or caregiver who works professionally or recreationally with lead; (4) a household member uses traditional folk or ethnic remedies or cosmetics; or (5) family designated at increased risk for lead exposure by the health department because of local risk factors for lead exposure, such as residing in a high-risk zip code (Wengrovitz and Brown, 2009).
Discipline
Parents frequently ask their primary care physician about discipline. Discipline should be a priority topic for anticipatory guidance at 15 months and 18 months (Hagan et al., 2008). Effective discipline requires three essential components: (1) a positive, loving relationship between the parent(s) and child, (2) positive reinforcement strategies to increase desired behaviors, and (3) punishment or removal of reinforcement to reduce or eliminate undesired behaviors (AAP Committee on Psychosocial Aspects, 1998). Although often confused with punishment, discipline actually means to teach. All children benefit from guidance and structure, and most children require occasional discipline. The best discipline is consistent and considers the child’s developmental level as well as the child’s point of view. Effective strategies include environmental modifications (e.g., childproofing the house), distraction, redirection, giving appropriate choices, and time-out. Although many parents spank (Regalado et al., 2004), corporal punishment is controversial and has potential long-term negative effects (Smith, 2006). Other methods of discipline are more effective over time and should be used. Some families may require more intensive assistance, and clinicians should be aware of local resources for teaching parents.
Nutrition
Infants and Toddlers
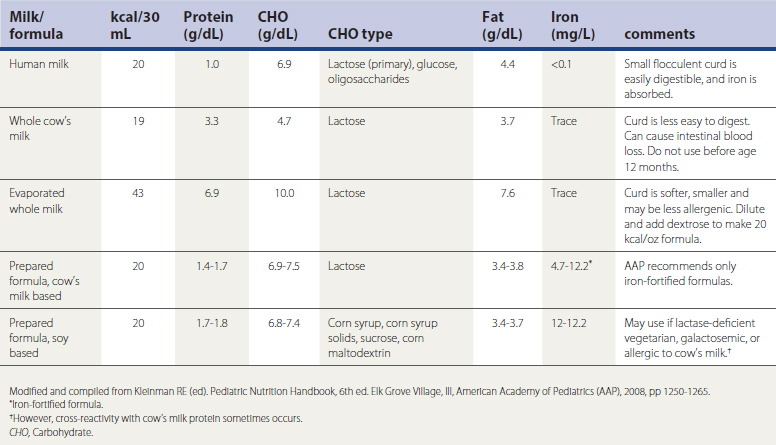
The composition of human milk varies by time, day, and maternal nutrition and from woman to woman. Infant formulas contain about 50% more protein than human milk and, like breast milk, provide 40% to 50% of energy as fat (Table 23-4). Beginning at 2 years of age, fat calories should decrease to approximately 30% of total energy consumption, with less than 10% of calories from saturated fat, and dietary cholesterol less than 300 mg/day (AAP, 2009).
Commercial cow’s milk and soy-based formulas must contain higher levels of protein to compensate for their lower quality (see Table 23-4). However, they are quite acceptable for mothers who are unable to nurse their infants or for parents who wish to bottle-feed their children. Soy formulas are recommended for infants with hereditary lactase deficiency or galactosemia and may be tried in infants intolerant to cow’s milk, but soy formula should not be used in preterm infants. Because some infants allergic to cow’s milk protein will develop an allergy to soy protein, it is advisable to use an extensively hydrolyzed protein formula in cases of true milk allergy or malabsorption. These are lactose free and may contain medium-chain triglycerides to improve fat absorption (AAP, 2009).
A toddler’s food intake may be quite variable from day to day or even meal to meal. Because young children cannot choose a well-balanced diet, parents must provide nutritious, safe, developmentally appropriate foods at regular meals and snacks. Children should be sitting in a designated area for mealtime, without distractions such as television (AAP, 2009). Small portions of food should be offered to preschool children, allowing the child to determine how much he or she will eat and offering more as necessary. Excessive portion sizes can contribute to obesity later in life. Guidelines about types and quantities of foods from the basic food groups are available from the U.S. Department of Agriculture (USDA) MyPyramid website (www.mypyramid.gov), which provides recommendations on the amount of grain products, vegetables, fruits, and milk products based on the person’s age, gender, and activity level.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree