Growing Rod Instrumentation for Early-Onset Scoliosis
Christine M. Goodbody
John M. Flynn
DEFINITION
Early-onset scoliosis (EOS) is defined by the diagnosis of scoliosis at or before the age of 5 years.
The many etiologies of EOS include the following:
Congenital vertebral or spinal anomalies: for example, vertebral bars, hemivertebrae
Neuromuscular diseases: for example, cerebral palsy, spinal dysraphism, muscular dystrophy
Syndromes associated with scoliosis: for example, neuro-fibromatosis
Idiopathic causes
Progressive and severe curves can be associated with deformity, thoracic insufficiency, restrictive pulmonary disease, pulmonary hypertension, cardiac disease, and increased mortality.
ANATOMY
Two periods of increased growth velocity are associated with increased incidence of curve progression. T1 to S1 growth velocity is greatest from birth until the age of 5 years (more than 2 cm per year), and by the age of 5 years, two-thirds of the final sitting height is achieved. Growth rate slows between ages 5 and 10 years (1 cm per year) before increasing again during puberty and the adolescent growth spurt (1 to 2 cm per year).5,14
The increased spinal growth during the first years of life is paralleled by an increase in thoracic and lung dimensions. Thoracic volume at birth is about 5% of the adult volume; by 5 years of age, it equals 30% of adult volume. A slower rate of thoracic growth occurs from 5 to 10 years of age, by which time it has reached 50% of the adult volume. The final 50% of adult volume is achieved during the adolescent growth spurt from 10 to 15 years of age.
PATHOGENESIS
The pathogenesis of EOS depends on its etiology.
Vertebral anomalies cause scoliosis by an imbalance in bone growth, secondary to either an increase in growth on a side associated with a hemivertebrae or growth retardation on the side associated with a vertebral bar.
In neuromuscular and central nervous disorders, an imbalance in muscular forces is pathogenic, likely following the Heuter-Volkmann principle that the physeal growth rate is related to the forces it is exposed to, with compression inhibiting growth and tension promoting it.
The etiology and pathogenesis of infantile idiopathic scoliosis (IIS) (0 to 3 years of age) is, by definition, unknown, but there is likely a component of genetic susceptibility. The external factors resulting in scoliosis are not yet clearly delineated but may include intrauterine molding as well as infant positioning. The etiology of IIS most likely differs from that of adolescent idiopathic scoliosis (AIS).
NATURAL HISTORY
The natural history of EOS also depends on the etiology.
The natural history of EOS due to IIS is favorable when compared with late-onset scoliosis (LOS). Spontaneous resolution occurs in a large number of patients. Progression of congenital curves depends on the type of anomaly and growth potential.
EOS due to neuromuscular etiologies usually follows the natural history of said neuromuscular disease, in addition to specific problems associated with progressive curves in this age group.
Regardless of the etiology, progression of scoliosis during the first 5 years of life adversely affects growth as well as pulmonary function.
A history of EOS is associated with a higher risk of cardiopulmonary decompensation in middle-aged patients, which can lead to disabling and even fatal respiratory failure.
PATIENT HISTORY AND PHYSICAL FINDINGS
Evaluation of the patient with EOS includes a complete history, including the family history, prenatal history, birth history, and developmental history.
IIS has been associated with breech presentation and, in boys, with premature birth.
Physical examinations includes observation of gait (if patient is ambulatory), respiration, truncal and pelvic balance in the coronal and sagittal planes, cutaneous lesions, and any prominence on Adams forward bending test.
Any deficits in motor, sensory, or reflex function, including abdominal reflexes, may indicate central nervous system pathology and should be thoroughly evaluated with advanced diagnostic studies.
Flexibility of the curve can be assessed either by the manual application of traction through the cervical spine or by applying a three-point bending force at the apex of the curve.
Examination techniques unique for EOS include the thumb excursion test for thoracic expansion and sitting height measurement.
IMAGING AND OTHER DIAGNOSTIC STUDIES
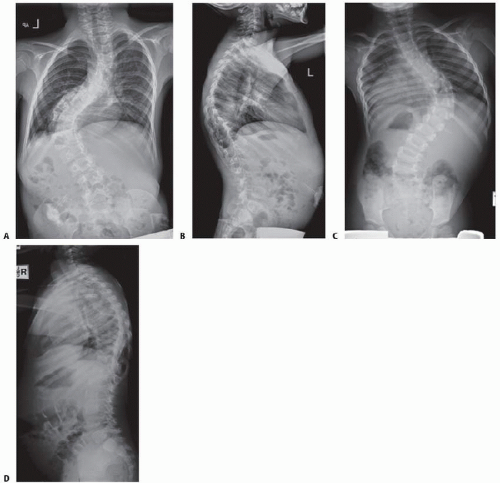
All patients should have full-length standing anteroposterior (AP) and lateral radiographs (FIG 1) covering the cervical spine to the pelvis, including the entire thorax. For patients who are unable to stand, supine radiographs encompassing the same area should be taken.
The cervical spine, lumbosacral spine, pelvis, and hips all may need to be studied to elicit whether or not developmental hip
dysplasia or other vertebral anomalies are contributing to the scoliosis.
Bolster bending, side-bending, or traction radiographs are necessary to help delineate the degree of flexibility of the curves.
The Cobb angle is used to assess initial curve severity and is followed over successive visits to evaluate for curve progression.
Spinal height is obtained by measuring the distance from the top of T1 to the top of S1 on the AP view of the spine.
Coronal balance is measured by the distance from the center of C7 to a line drawn up from S1.
The sagittal balance is measured from the posterior cranial corner of S1 to a line drawn down from the center of C7.
All of these measurements should be recorded and compared on successive visits to document any change in curve magnitude or growth of the spine.
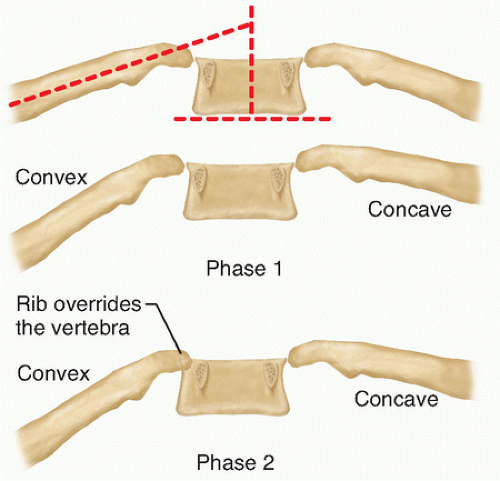
The rib-vertebral angle difference (RVAD) of Mehta (FIG 2), first described in 1972, measures the amount of rotation at the apex vertebra and has some prognostic value.10
The angles formed by a line perpendicular to the vertebra and a line drawn down the center of the rib is compared between the convex and concave side. If the difference calculated by subtracting the convex angle to the concave angle is 20 degrees or less, there is an 85% to 90% chance the curve will resolve; when there is a difference of 21 degrees or more, it will likely progress.
The phase of the rib head is determined by whether or not the head of the convex rib overlaps the vertebral body.
If there is no overlap (phase 1), then the RVAD is calculated as previously mentioned.
If there is overlap (phase 2), the risk of progression is high, regardless of RVAD.
The space available for the lung (SAL) is calculated by taking the ratio of the distance from the apex of the most cephalad rib to the highest point of the hemidiaphragm of the concave side divided by the convex side.
A lower SAL points toward a poorer prognosis for lung function.
Magnetic resonance imaging (MRI) is recommended to evaluate for spinal cord anomalies in children with rapidly progressive spinal deformities, clinical findings concerning for spinal cord anomalies, or preoperative patients. Before embarking on a repetitive distraction technique such as growing rods, it is particularly valuable to know whether there is a tethered spinal cord.
MRI is also used to measure lung volume and assess thoracic architecture when thoracic insufficiency is an issue.
In severe congenital deformity, the ribs may spiral around the vertebrae, causing the thoracic volume on one side to be severely diminished while the other is larger, creating what Campbell4 calls a “windswept thorax.”
Computed tomography (CT) scanning is not routinely used, particularly in an era where we are increasingly concerned about high levels of medical radiation in very young patients.
DIFFERENTIAL DIAGNOSIS
Congenital vertebral or spinal anomalies
Vertebral bars
Hemivertebrae
Syrinx
Tethered cord
Neuromuscular diseases
Cerebral palsy
Myelodysplasia
Muscular dystrophy
Syndromes associated with scoliosis
Beel syndrome
Trisomies
IIS
NONOPERATIVE MANAGEMENT
Nonoperative treatment for EOS is indicated in curves that are not expected to progress.
Patients with a curve of less than 25 degrees and RVAD less than 20 degrees may be followed with serial radiographs every 4 to 6 months to document any progression.
Active treatment is warranted in the following:
Progression greater than 10 degrees
Phase 2 rib-vertebral relationship, RVAD greater than 20 degrees, or a Cobb angle greater than 25 degrees in any skeletally immature patient
Nonoperative treatment generally starts with casting or bracing.
Brace treatment should be abandoned in favor of surgical management when unacceptable curve magnitude or progression is seen.
SURGICAL MANAGEMENT
Surgical treatment of EOS attempts to stop progression of the scoliosis, allowing improvements in growth of the spine, thorax, and lungs.
Surgery is recommended for progressive curves with a Cobb angle greater than 45 degrees.
The age of the patient helps to determine the type of surgery needed.
Adolescents and more skeletally mature patients may do well with spine fusions, which stabilize the spine but also stop growth.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree