Groin Flap Coverage of the Hand and Wrist
Jeffrey B. Friedrich
Nicholas B. Vedder
Indications/Contraindications
The pedicled groin flap is an extremely versatile and reliable flap that was initially described in 1972 by MacGregor and Jackson. It enjoys a revered place in the field of reconstructive surgery because it was one of the first axial-pattern flaps to be described and applied in humans. After several decades, many surgical techniques, including pedicled flaps, have been supplanted by new methods. However, despite the advent of microsurgery, the pedicled groin flap continues to be a venerable technique with a variety of applications.
The groin flap has been used most commonly for upper extremity reconstruction, and is indicated for soft tissue defects in which there is destruction or devitalization of soft tissue on the hand, wrist, and distal forearm. The groin flap is not designed to supplant skin-grafting on wounds that will accept a graft; rather, it is to be used when the injury or resection leaves exposed structures that will not accept a skin graft, such as tendon or bone. It has been described for soft tissue reconstruction of a number of traumatic etiologies including crush injuries, avulsions, gunshots, blast wounds, and burns. Additionally, the flap is warranted for soft tissue defects following elective resection such as contractures, hypertrophic scarring, or tumor, and has even been described as soft tissue coverage following recurrent carpal tunnel syndrome.
In the setting of trauma, the groin flap is most often used for delayed primary coverage of upper extremity wounds. Several groups have employed the flap for very early coverage (within 24–48 hours from injury); however, the complication rate has been found to be high. Therefore, unless a clean and healthy wound bed can be ensured initially, it is generally prudent to thoroughly debride the wound, observe it for a few days, and then apply the groin flap only after a clean, healthy wound surface is ensured.
As noted above, the groin flap will provide reliable soft tissue coverage to practically any portion of the hand as well as the distal forearm. It is particularly well-suited to the dorsal surface of the hand. The flap can certainly be used to provide coverage for the palmar surface of the hand; however, the flap can be bulky, and does not at all approximate the native, adherent, glabrous skin of the palm. This can leave the palm with a bulky flap that is prone to shearing motion when weight is borne on the palmar surface of the hand, such as seen with pushing, gripping, tool use, or twisting motions. For this reason, it is wise to consider other thinner flaps such as the reversed radial forearm flap or free fasciocutaneous flaps such as the anterolateral thigh flap for most palmar reconstructions.
A brief mention must be made of the groin flap for use as a free tissue transfer. The free groin flap was the first free flap described and can be used for many of the same indications for which other free flaps are currently used. Its reliability is somewhat limited because of the variable arterial pedicle and the short length of the pedicle. Furthermore, even in experienced hands, the free groin flap failure rate is notably higher than it is for other free flaps, thus limiting its utility.
Another chief indication for use of the groin flap is in the setting of thumb reconstruction. Often with total or near-total thumb loss, it is necessary to use free digit transfers such as the great or second toe. Unfortunately, traumatic thumb amputations can leave the patient with insufficient soft tissue of the thenar region. In these cases, the groin flap is an excellent choice to provide a soft-tissue “base” on to which the digit transfer can be placed at a later date.
The contraindications for the use of the pedicled groin flap are few. In general, the flap should not be implemented in patients who are deemed to be uncooperative, or who would otherwise not be able to tolerate a 2- or 3-week interval in which their affected hand is immobilized and attached to the groin. In the past, it was felt that elderly patients were not good candidates for this flap because of the risk of shoulder and elbow stiffness. However, a recent study has shown that elderly patients are able to tolerate the procedure with no more complications (including upper extremity stiffness) than the average young patient.
As with any flap, active tobacco use is a concern with the groin flap. Specifically, the flap can be subject to marginal necrosis in active smokers. The surgeon must balance the need for complex reconstruction with the potential morbidity that may be incurred by patients who smoke.
Previous groin surgery may or may not be a contraindication to the use of this flap. In general, inguinal hernia repair does not preclude the use of the groin flap, nor do other scars in the general vicinity such as abdominoplasty or Pfannenstiel incisions. However, a previous inguinal lymph node dissection would render this flap tenuous, or outright unsafe. The potential disruption of superficial vessels in the groin is too high to risk use of a flap based on these vessels. Additionally, patients who have had groin lymph node dissections have quite often had external beam radiation to the same region, further rendering flap dissection in this area a dangerous proposition.
Preoperative Planning
When using the groin flap in the acute posttraumatic setting, wound preparation is of paramount importance. The surgeon must perform any hand or forearm repairs that are necessary in the acute phase. This includes fracture reduction and fixation, as well as tendon, vessel, and nerve repair. Wound debridement must also be complete so as to minimize the infection risk once the site is covered with a flap. Wound debridement and cleansing may need to be done several times in the operating room prior to flap coverage, and several days of dressing changes may be necessary to ensure that the wound bed is as healthy as possible. This is especially true with crush and avulsion injuries.
In the posttraumatic setting, timing of coverage with a groin flap has become an important issue. In general, most published reports advocate use of the flap in a delayed-primary fashion, specifically between 48 hours and 7 days following injury. Others have attempted to employ the flap in a more acute setting (24–48 hours following injury); however, the consensus seems to be that early timing leads to an unacceptably high rate of infection and dehiscence, and is thus not advocated. In the end, timing of flap implementation should be based on the surgeon’s best clinical judgment about the mechanism of injury, and the status of the wound bed.
In the elective setting, the preoperative preparation for a groin flap is somewhat less crucial. The patient must understand that the interval between flap elevation and flap division will entail a moderate amount of disability, and will require a significant amount of diligence in regard to their self-care. Additionally, it is a good idea for the patient to make prior arrangements to have a friend or family member at home who will be able to assist them with various activities of daily living.
Surgery
The groin flap coverage surgery must be done with a general anesthetic. Additionally, it is recommended that a bladder catheter be placed as the operation can be in excess of 3 hours. If the patient is not already being administered intravenous antibiotics for prophylaxis of a traumatic wound, one dose of antibiotics should be administered 30 minutes before skin incision.
Patient Positioning
Once anesthetized, care should be taken with patient positioning. Although an ipsilateral groin flap is most commonly used, a contralateral flap is sometimes acceptable if the ipsilateral side is for some reason unavailable. Regardless of which side is chosen, a small towel roll or “bump” should be placed under the hip of the side that will undergo groin flap dissection to allow extension of the flap
dissection back to the flank. The upper extremity to be reconstructed should be placed on a hand table for initial wound preparation. Additionally, one should leave enough room on the side of the operating table to be able to comfortably lay the upper extremity beside the torso during groin flap inset. The other necessary step before initiating the operation is placement of a pneumatic tourniquet on the upper extremity to be reconstructed.
dissection back to the flank. The upper extremity to be reconstructed should be placed on a hand table for initial wound preparation. Additionally, one should leave enough room on the side of the operating table to be able to comfortably lay the upper extremity beside the torso during groin flap inset. The other necessary step before initiating the operation is placement of a pneumatic tourniquet on the upper extremity to be reconstructed.
Technique
The operation is begun by preparation of the recipient bed. If the flap is being employed for traumatic wound coverage, a final thorough debridement is done at this time. If it is being done for scarring or other elective soft tissue coverage, the creation of the recipient wound to be covered is done in its entirety before moving to the groin.
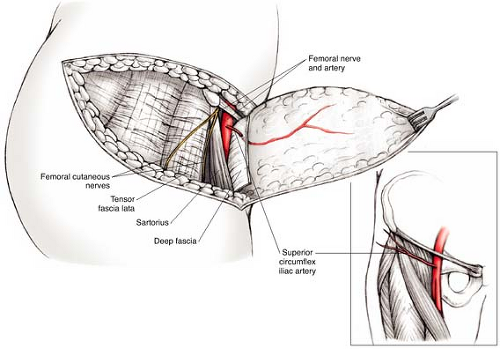
In preparation for flap elevation, measurements are taken to determine the required dimensions of the groin flap. This can be done in several ways. One can simply use a ruler to determine the largest dimensions of the wound, or a template can be fashioned. The paper wrapper from surgical glove packaging makes a nice template material and is readily available. This can be pressed onto the wound so that the wound fluid makes an imprint in the paper. Then the template can be made simply by cutting around the outline of the defect. Alternatively, one can use a piece of the elastic wrap used to exsanguinate the hand (Fig. 19-1). The template is then transferred to the groin. In general, the more ulnar aspects of the wound will be covered by the distal end of the flap.
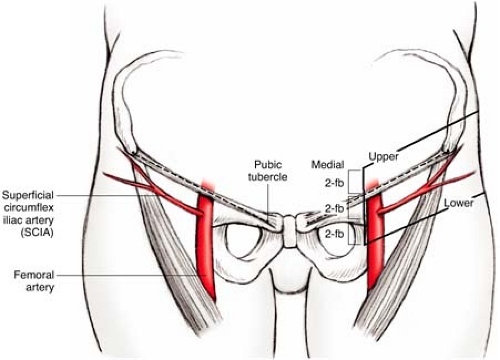
When designing the flap, one must keep in mind the arterial anatomy of the flap. Specifically, the flap is supplied by the superficial circumflex iliac artery and vein (Fig. 19-2). Numerous studies have shown the artery to consistently extend to the level of the anterior superior iliac spine (ASIS) before any significant caliber diminishment. In other words, the flap is an axial pattern flap medial to the ASIS, and a random-pattern flap lateral to this point. The area lateral to the ASIS can be used as part of the flap design; however, its effectiveness is limited by its random nature. Therefore, the operator should generally design a flap that, at the portion lateral to the ASIS, has a width:length ratio between 1:1 to 1:1.5 (although the medial portion needs only be wide enough to include the axial vessels). It is possible to design a flap whose distal extent is more posterior than this limit, but a delay procedure should then be employed for the flap. A delay procedure involves incision, but not elevation
of the desired flap. The incised flap is then left in situ for a week so that the circulation at the distal end of the flap can be augmented during that time. Following that interval, the flap can then be elevated and inset in the upper extremity wound.
of the desired flap. The incised flap is then left in situ for a week so that the circulation at the distal end of the flap can be augmented during that time. Following that interval, the flap can then be elevated and inset in the upper extremity wound.
 FIGURE 19-1 Use of a piece of the elastic exsanguination wrap to create a template of the defect to be covered with a groin flap. |
When beginning the overall design of the flap, it is best to keep in mind the recommendations of Chuang, who published a set of groin flap design rules based on experience amassed via the use of over 200 groin flaps. The mainstay of these guidelines is the “two fingerbreadths” rule (the two fingerbreadths being at the level of the index and long finger distal interphalangeal joint of the operator) (Fig. 19-3). The first step is to estimate the location of the superficial circumflex iliac artery, done by marking a point two fingerbreadths below the junction between the inguinal ligament (which runs along a line between the anterior superior iliac spine and the pubic tubercle) and the femoral artery. Once that artery location is estimated, its true path should be verified by Doppler ultrasound. The upper flap border is marked two fingerbreadths above the inguinal ligament (parallel to the artery), while the lower flap border is a line two fingerbreadths below and parallel to the artery. Also, as will be further discussed following, the superficial branch of the superficial circumflex iliac artery (SCIA) emerges from the deep fascia two fingerbreadths medial to the ASIS, then continues laterally in a subcutaneous plane.
It should be noted that if using the two fingerbreadths rule for flap design, a relatively slender flap will result medially. In reality, when the flap is centered over the SCIA, the cephalad-caudad width of the flap lateral to the ASIS can be quite substantial. However, most authors agree that flap widths up to 10 cm enable primary closure of the groin wound site, while those that are wider stand a good
chance of requiring closure with a split-thickness skin graft because of inability to achieve primary closure. It is usually possible to determine how wide a flap can safely be harvested and closed primarily by pinching the skin and subcutaneous tissue together. Flexing the operating table at the hip to relieve some of the tension can facilitate closure.
chance of requiring closure with a split-thickness skin graft because of inability to achieve primary closure. It is usually possible to determine how wide a flap can safely be harvested and closed primarily by pinching the skin and subcutaneous tissue together. Flexing the operating table at the hip to relieve some of the tension can facilitate closure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree