CHAPTER 20 Great Toe Arthroscopy
Arthroscopy of the first metatarsophalangeal joint (MTP-1) was originally described by Watanabe in 1972.1 Because of the small size of the joint, the applicability of arthroscopy has been limited by the small number of clinical results reported in the literature. Advances in technology for visualization and instrumentation and the recent clinical experience of the surgeons have propelled small joint arthroscopy into a new era. Although arthroscopy in the MTP-1 has not been as widely used as arthroscopy in the knee or the shoulder, its value has been demonstrated, and its use continues to grow for the treatment of traumatic and degenerative conditions and for reconstructive procedures. With proper patient selection and familiarity with the technique, MTP-1 arthroscopy can be a useful addition to the surgeon’s armamentarium.
NORMAL AND PATHOLOGIC ANATOMY
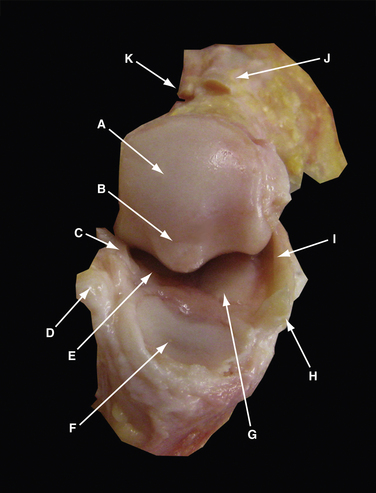
The MTP-1 is composed of the first metatarsal head and neck, proximal phalangeal base, and medial and lateral sesamoids. The first metatarsal articular surface is composed of two fields in continuity, the superior phalangeal and inferior sesamoidal fields. The former is smaller and convex, whereas the latter is larger and separated into two sloped surfaces by a small bony ridge or crista (Fig. 20-1). The proximal phalanx articular surface is oval, concave, and smaller than the corresponding articular surface of the metatarsal head. The base of the proximal phalanx serves as insertions of the extensor hallucis brevis and longus dorsally and the intrinsic muscles of the big toe and plantar plate plantarly.
The dorsomedial aspect of the joint contains a sizable synovial fold, with the average width of 7 mm and covering 29% of the joint.2 It has abundant blood supply, but the nerve supply is found only in the periphery.
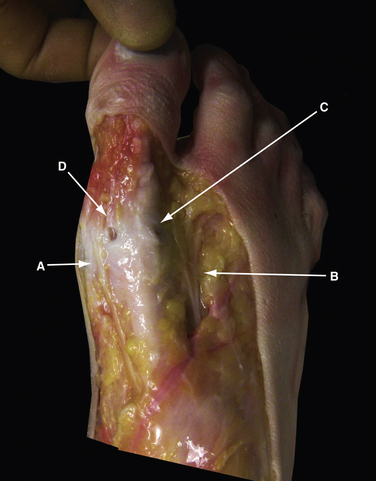
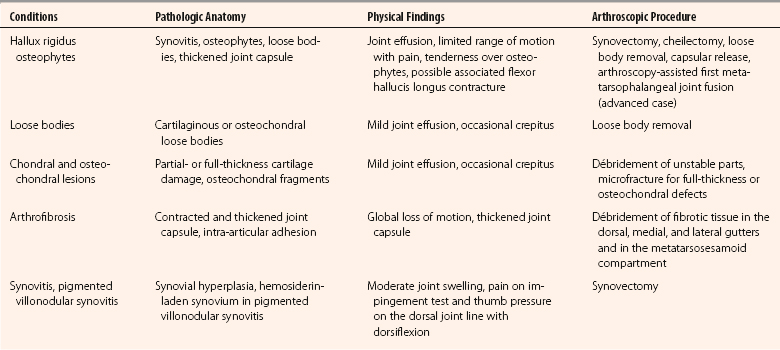
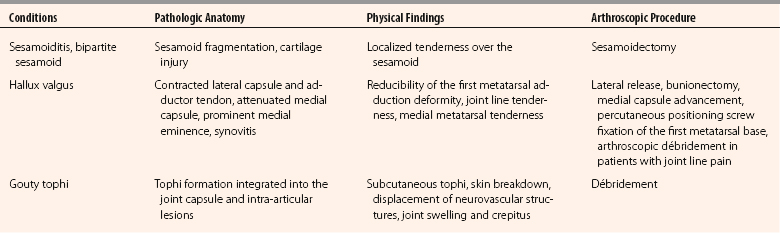
At the level of the MTP-1, the distribution of the cutaneous nerve varies, but the dorsomedial and dorsolateral cutaneous branches usually originate from the medial dorsal cutaneous branch of the superficial peroneal nerve and the deep peroneal nerve, respectively (Fig. 20-2). The plantar medial and plantar lateral branches originate from the medial plantar nerve. The dorsomedial cutaneous nerve lies close to the dorsomedial portal and is on average 13.1 mm medial to the extensor hallucis longus tendon,3 but it has been reported to be 2 to 5 mm from it.4 The plantar medial hallucal nerve is on average 10.6 mm plantar to the midline, which is the location for the medial portal. Because of the variations of the nerves in the foot, all the arthroscopic portals should be handled as if a nerve was located directly underneath. The pathologic anatomy of various conditions of the MTP-1 that can be addressed arthroscopically or endoscopically are listed in Table 20-1.
PATIENT EVALUATION
History and Physical Examination
Patients with MTP-1 problems usually present with forefoot pain. Obtaining a problem-focused history should include the characteristics of pain, swelling, deformities, associated injuries, preexisting diseases, shoewear, prior treatments, and a family history. Athletic activities and expectation are also important factors. Systemic diseases can be associated with increased uric acid and urate crystal arthropathy, which is a common cause of MTP-1 pain.5
Physical examination is the cornerstone of all clinical judgments. We always perform a systematic and thorough examination of all patients with foot and ankle problems, starting with gait, skin, motor, motion, palpation, and special tests. Patients with considerable pain in the MTP-1 may walk on the lateral border of the foot. The forefoot should be observed for deformities, swelling, and discoloration. Active and passive motion of the MTP-1 should be evaluated and compared with the contralateral side. The average passive motion of the MTP-1 in men older than 45 years is 87 degrees, with 67 degrees of dorsiflexion and 20 degrees of plantar flexion.6 Patients with decreased range of motion of the MTP-1 should be differentiated by the characteristics of stiffness. Arthrofibrosis or osteoarthrosis may result in global loss of motion, whereas an early hallux rigidus may produce primarily limited dorsiflexion. Pseudo-hallux rigidus can mimic or be associated with a hallux rigidus, but the tightness from the flexor hallucis longus tendon contracture can usually be decreased by ankle plantar flexion.7 Occasionally, crepitus can be differentiated from arthritis, osteochondral injury, or loose bodies. Pain can be provoked with forced dorsiflexion in patients with hallux rigidus or soft tissue impingement. Bony landmarks, such as the head of the first metatarsal and the base of the proximal phalanx, are superficial and easily palpable. Pain in daily activities often can be reproduced by direct palpation over the osteophytes or the sesamoids.
In hallux valgus, the first metatarsal adduction can be evaluated if it can be manually corrected, which is a requirement for an endoscopic correction of hallux valgus deformity.8 Sometimes, complete correction may not be achieved because of obstruction by the dislocated fibular sesamoid bone in the web space. This is not a contraindication for the procedure, because the sesamoid bone can be reduced after lateral release, and the intermetatarsal space can then be closed. Specific physical examinations for various pathologies of the MTP-1 that are amendable to arthroscopic treatment are listed in Table 20-1.
Diagnostic Imaging
We use standard weight-bearing anteroposterior, lateral, and axial sesamoid views for initial evaluation of all patients with forefoot problems (Fig. 20-3). Osteophytes, joint space narrowing, and loose bodies usually can be demonstrated.
Elevation of the first metatarsal in relation to the lesser metatarsals can be associated with hallux rigidus.9 Inflammatory arthropathy can develop juxta-articular osteopenia or joint destruction in the late stages, whereas gouty tophi often have juxta-articular punch-out lesions and soft tissue thickening. Hallux valgus requires measurements of the hallux valgus angle, intermetatarsal angle, distal metatarsal articular angle, and proximal phalanx articular angle. Oblique views may be helpful in visualizing dorsal MTP-1 osteophytes, the joint space, and the profile of an individual sesamoid.
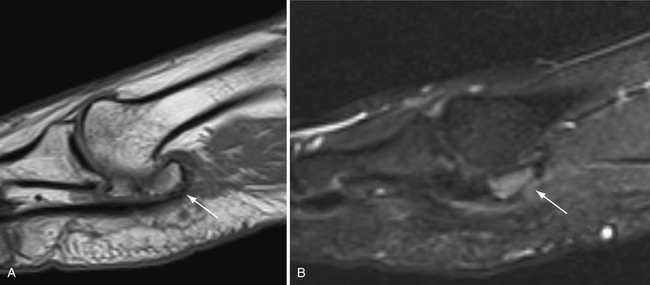
Computed tomography (CT) is rarely indicated, but it can better visualize the osteochondral lesions or loose bodies with an osseous component. Magnetic resonance imaging (MRI) can demonstrate a bone bruise, cartilage defects, and synovial hyperplasia, especially with pigmented villonodular synovitis (PVNS), which has low signal intensity on T1-weighted and T2-weighted images.10 MR images of a symptomatic, bipartite medial sesamoid are shown in Figure 20-4. Ultrasound imaging is advantageous in the forefoot because of its magnification power and real-time visualization.11 It can identify loose bodies and small bone spurs. The probe can also be used to reproduce pain with direct pressure over the suspected location.
TREATMENT
Indications and Contraindications
Contraindications to arthroscopic treatment are as follows:
Arthroscopic Technique
Positioning
We prefer to do the arthroscopy of the MTP-1 with the patient in a supine position and with both hips in abduction (Fig. 20-5). The surgeon has 360-degree access to the forefoot, but most of the procedures can be done with the surgeon at the end of the bed. Plantar portals, if needed, can be approached with the surgeon sitting between the patient’s legs.
Instruments
A 1.9- or 2.7-mm, 30-degree, small joint arthroscope is used for most arthroscopic visualization of the MTP-1. The 1.9-mm arthroscope is used in tight joints, especially when no traction is applied, but it should be handled with care because of its fragility. A 4-mm, 30-degree arthroscope, which provides a wider field of view and easier orientation, is helpful in periarticular endoscopy, such as in a first web space release and gouty tophi excision. The gravity-driven inflow usually is adequate, and the arthroscopic pump is rarely required. An alternative is to use a 50-mL syringe with continuous irrigation controlled by an assistant. Small bone-cutting shavers allow soft tissue and bone débridement, which can minimize instrument switching. Equipment is listed Box 20-1 and Figure 20-6.