Chapter 94 Glucosamine
 General Description
General Description
Glucosamine is a simple molecule, manufactured in the body from glucose and an amine. One of the primary physiologic roles of glucosamine is in the joints, where it stimulates the manufacture of glycosaminoglycans (GAGs), key structural components of cartilage. Glucosamine also promotes the incorporation of sulfur into cartilage. Because of this effect, glucosamine sulfate (GS) is thought to be the best source of glucosamine (Figure 94-1).
 Available Forms
Available Forms
When authors or manufacturers discuss glucosamine hydrochloride or NAG, they often cite references of clinical studies that used GS or the combination of glucosamine hydrogen chloride (HCl) and chondroitin sulfate. On the basis of currently available clinical evidence, it appears that only GS provides proven clinical effectiveness when administered as an isolated agent (numerous studies showed the combination of glucosamine HCl and chondroitin sulfate to be effective). It does not appear to matter, however, if the GS is stabilized with either sodium or potassium.1
 Glucosamine Sulfate Versus N-Acetylglucosamine
Glucosamine Sulfate Versus N-Acetylglucosamine
NAG differs from GS in that instead of a sulfur molecule, NAG has a portion of an acetic acid molecule attached to it. GS and NAG are different molecules and appear to be handled by the body differently. Companies marketing NAG claim that this form is better absorbed, more stable, and better used than GS. These contentions are without support in the scientific literature. Detailed human studies on the absorption, distribution, and elimination of orally administered GS show an absorption rate as high as 98% and that, once absorbed, it is then distributed primarily to joint tissues, where it is incorporated into the connective tissue matrix of cartilage, ligaments, and tendons.2,3 In addition, there are impressive clinical studies on thousands of patients. In contrast, the only clinical study with NAG used was as a polymer that is not yet available commercially.4 Polymerization is thought to be necessary due to the poor oral availability of unbound NAG.
Further evidence of the superiority of GS to NAG is offered by studies on laboratory animals. Several studies demonstrated that glucosamine absorption and utilization are at least twice that of NAG.5–16 The researchers concluded that glucosamine was a more efficient precursor of macromolecular hexosamine (GAG) than NAG. It is possible that NAG does not penetrate the cell membranes and, as a result, is unavailable for incorporation into glycoproteins and mucopolysaccharides.7 The body preferentially uses GS rather than NAG. This preference appears largely due to the active processes that enhance absorption of GS in the intestines.17
The absorption of NAG by humans is poor for several reasons:
• NAG is quickly digested by intestinal bacteria.
• NAG binds with dietary lectins in the gut, resulting in a lectin-NAG complex, which is excreted in the feces.
• A large percentage of NAG is metabolized by intestinal cells.
In addition to the question of absorption, several studies showed that the articular tissue cannot use NAG as well as it does glucosamine.6,7 These absorption and utilization problems suggest NAG is highly unlikely to possess the same kind of antiarthritic and anti-inflammatory properties that GS has been shown to possess.
 Glucosamine Sulfate Versus Glucosamine Hydrogen Chloride
Glucosamine Sulfate Versus Glucosamine Hydrogen Chloride
Research showed that sulfur is an extremely important component in the therapeutic effect of GS, and its substitution is likely to decrease the efficacy of supplemental glucosamine.18 Sulfur is an essential nutrient for joint tissue, where it functions in the stabilization of the connective tissue matrix of cartilage, tendons, and ligaments. Even healthy humans have low serum sulfate (0.3 to 0.4 mM) and synovial sulfur levels, but in OA these concentrations are even lower. As far back as the 1930s, researchers demonstrated that individuals with arthritis were commonly deficient in this essential nutrient.19,20 Restoring sulfur levels brought about significant benefit to these patients.19 In addition to sulfur playing a critical role in the manufacture of GAGs like chondroitin sulfate and keratan sulfate, sulfur was shown to inhibit the various enzymes that lead to cartilage destruction in OA (e.g., collagenase, elastases, and hyaluronidase).18,21
Results from double-blind studies indicated that glucosamine HCl might be no more effective than a placebo in relieving OA. One double-blind, placebo-controlled, 10-week study examined the effects of glucosamine HCl in patients with OA of the knee.22 Patients received either 500 mg of glucosamine HCl or a placebo three times daily. Forty-five patients received glucosamine HCl, whereas 53 received the placebo. The results indicated that 49% of patients who received glucosamine HCl felt they had improved compared with 45% of the placebo group, who said they felt improved. However, the difference between the two groups was not statistically significant. What these results call into question is the viability of glucosamine HCl as an effective form of glucosamine. Unfortunately several large, well-publicized studies utilized this form. For example, the Glucosamine/chondroitin Arthritis Intervention Trial (GAIT) study involved 1583 patients with symptomatic knee OA.23 Patients were randomized to receive 1500 mg of glucosamine daily, 1200 mg of chondroitin sulfate daily, both glucosamine and chondroitin sulfate (same dosages as the single arms), 200 mg of celecoxib daily, or placebo for 24 weeks. Mean age of the patients was 59 years, and 64% were women. Overall, glucosamine and chondroitin sulfate were not significantly better than placebo in reducing knee pain by 20%. Compared with the rate of response to placebo (60.1%), the rate of response to glucosamine was 3.9% higher, the rate of response to chondroitin sulfate was 5.3% higher, and the rate of response to combined treatment was 6.5% higher. The rate of response in the celecoxib control group was 10.0% higher than that in the placebo control group. For patients with moderate-to-severe pain at baseline, the rate of response was significantly higher with combined therapy than with placebo (79.2% vs. 54.3%).
In an analysis of GAIT subjects with a radiographic confirmation of OA, the odds of achieving a 20% reduction in Western Ontario and McMaster Osteoarthritis Index (WOMAC) pain score, compared with placebo, were celecoxib: 1.21, glucosamine: 1.16, combination glucosamine/chondroitin sulfate: 0.83, and chondroitin sulfate alone: 0.69. These rates were not statistically significant.24,25
 Clinical Applications
Clinical Applications
The primary use for GS is in the treatment of OA. This application has significant support in the medical literature because numerous double-blind studies have shown GS to produce much better results compared with non-steroidal anti-inflammatory drugs (NSAIDs), placebo, or acetaminophen in relieving the pain and inflammation of OA.26–30 Although some of the studies comparing GS with NSAIDs or acetaminophen showed similar reduction in pain and symptom scores, only GS improved indexes of joint function or markers showing improvement of cartilage structure. Typically, the advantages of GS over these other treatments were seen after 2 to 4 weeks of use, but there is some evidence that the longer GS is used, the greater the therapeutic benefit.
Not all studies showed clear positive results, because a few exist that showed no greater benefit for GS over placebo in improving symptom scores.31–36 However, it must be kept in mind that the placebo response in OA is quite high and may confound the true benefit of GS and other approaches to OA. Fortunately, there were several studies that showed objective improvements (discussed in the immediately following paragraphs).
The two longest placebo-controlled trials were 3 years in duration. The results from these studies showed, quite convincingly, that GS slowed down the progression of OA and in many cases produced regression of the disease, as noted by radiologic improvements, and significantly reduced the incidence of total joint replacement even after as much as 5 years after GS discontinuation.36–39
In the first long-term study, 212 patients with knee OA were randomly assigned 1500 mg oral GS or placebo once daily for 3 years. Weight-bearing anteroposterior radiographs of each knee in full extension were taken at enrollment and after 1 and 3 years. Mean joint-space width of the medial compartment of the tibiofemoral joint was assessed by digital image analysis, whereas minimum joint-space width (i.e., at the narrowest point) was measured by visual inspection with a magnifying lens. Symptoms were scored by the WOMAC OA index. The 106 patients on placebo had a progressive joint-space narrowing, with a mean joint-space loss after 3 years of −0.31 mm. No significant joint-space loss occurred in the 106 patients on GS (−0.06 mm). Similar results were reported with minimum joint-space narrowing. As assessed by WOMAC scores, symptoms worsened slightly in patients on placebo compared with the clinical improvement observed in the group that received GS.
To investigate the relationship between baseline radiographic severity of knee OA and the importance of long-term joint-space narrowing in more detail, a subanalysis of data from the 3-year trial was performed.40 Measurements of mean joint-space width, assessed by a computer-assisted method, were performed at baseline and after 3 years on weight-bearing anteroposterior knee radiographs. Those who received GS demonstrated a trend for significant reduction in joint-space narrowing in patients in the highest quartile of baseline mean joint-space width (>6.2 mm). In these patients, a joint-space narrowing of 14.9% occurred in the placebo group after 3 years, whereas patients from the GS group only experienced a narrowing of 6%.
Of 414 participants randomized in the two long-term studies, 319 were postmenopausal women. In a subset analysis, after 3 years, postmenopausal participants in the GS group showed no joint-space narrowing, whereas participants in the placebo group experienced a narrowing of −0.33 mm. Percent changes after 3 years in the WOMAC index showed an improvement in the GS group (−14.1%) and a trend for worsening in the placebo group (5.4%). These results indicated that postmenopausal women might be especially responsive to GS.36
Additional insight into who might best respond to GS was provided in another analysis from this 3-year study that examined the ability of GS to improve a biochemical marker of collagen type II degradation (CTX-II).41 At baseline, the 212 patients had an average concentration of urinary CTX-II of 222.4 ng/mmol creatinine. This was significantly above the CTX-II levels measured in urine samples from 415 healthy controls (169.1 ng/mmol). Although there was no significant difference in the CTX-II response in the placebo group and the glucosamine-treated group, those with high cartilage turnover presented a significant decrease in CTX-II after 12-month glucosamine treatment.
In the second study, 202 patients with knee OA were randomized to receive oral GS (1500 mg once a day) or placebo. Changes in computed tomographic radiographic minimum joint-space width were measured in the medial compartment of the tibiofemoral joint, and symptoms were assessed using the Lequesne (an index of severity of osteoarthritis) and WOMAC. Although symptoms improved more significantly in the GS group, the most telling result was the fact that progressive joint-space narrowing with placebo use was −0.19 mm after 3 years, whereas there was no average change with GS use (an increase of 0.04 mm was the average).38
Another study sought to determine changes in levels of serum cartilage oligomeric matrix protein (COMP) and urine c-telopeptide of CTX-II as markers for cartilage turnover in patients with OA of the knee, in response to muscle strength training in combination with treatment with glucosamine, ibuprofen, or placebo. All three groups increased their muscle strength after 12 weeks of strength training. Glucosamine’s reduction of serum COMP was statistically significant compared with both placebo and ibuprofen; the mean reduction with glucosamine was 13% versus placebo and 17% versus ibuprofen. This suggested an effect by glucosamine on the response of the OA cartilage to a period of joint loading in humans with knee OA. No effect was noted on CTX-II.42
Several head-to-head, double-blind studies also showed that GS produced much better results compared with NSAIDs and analgesics in relieving the pain and inflammation of OA, despite the fact that GS exhibited little direct anti-inflammatory effect and no direct analgesic or pain-relieving effects.43–47 Although NSAIDs and analgesics, like acetaminophen, offer purely symptomatic relief, and NSAIDs may actually promote the disease process, GS appears to address the cause of OA. By promoting cartilage synthesis, thus treating the root of the problem, GS not only relieves the symptoms but also helps the body to repair damaged joints. The clinical effect is impressive, especially when glucosamine’s safety and lack of side effects are considered.
In one of the earlier comparative studies in which GS (1500 mg/day) was compared with ibuprofen (1200 mg/day), pain scores decreased faster in the first 2 weeks in the ibuprofen group. However, by week 4, the group that received GS experienced a significantly better improvement than the ibuprofen group.43 Physicians rated the overall response as good in 44% of the GS-treated patients compared with only 15% of the ibuprofen group.
Additional studies designed to further evaluate the comparative effectiveness of GS to NSAIDs provided even better evidence.44–4648 One study consisted of 200 subjects with OA of the knee given either GS (500 mg three times daily) or ibuprofen (400 mg three times daily) for 4 weeks.44 Consistent with previous studies, the ibuprofen group experienced quicker pain relief. However, by the end of the second week, the group taking GS experienced results as good as those in the ibuprofen group with one major exception—although the rate of side effects with glucosamine were mild and only affected 6% of the group, ibuprofen produced more significant side effects much more frequently, with 35% of the group experiencing them.
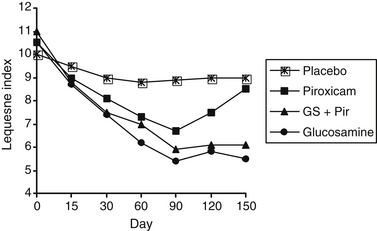
In another study, 329 patients were given 1500 mg GS, 20 mg piroxicam, both compounds, or a placebo for 90 days.45 The main efficacy variable was represented by the Lequesne index, a standard method of assessing disease activity. As can be seen in Figure 94-2, the results of the study were strikingly in favor of GS alone.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree