General Considerations
Peter F. M. Choong
Resections and reconstructions of the proximal femur are usually performed for malignant disease (1,2,3,4,5,6,7). Non-neoplastic conditions may also require similar resections and reconstructions (8,9,10) and these include complications of total hip arthroplasty including gross loosening with bone loss, periprosthetic fracture, and failed conventional treatment of proximal femoral fractures. The nature of the resection and hence the reconstruction will depend on the etiology of the condition. Regardless of the indication, the challenges that unite the treatment of these conditions are the potential for resection of considerable lengths of bone, loss of important soft tissue attachments, instability of the joint, and alteration in the normal function of the hip.
INDICATIONS
Primary Malignancies of Bone
The proximal femur and the femoral diaphysis are common locations for a number of primary bone malignancies. These include chondrosarcoma, Ewing sarcoma, and osteosarcoma. The surgical management of primary tumors mandate adherence to certain principles of oncologic surgery that aim to maximize the local control of disease. The most important aspect of tumor resection is to ensure oncologically sound margins (11,12,13,14,15). Intralesional margins that breach the tumor capsule should be avoided at all costs. Marginal excisions that pass through the edematous zone of areolar tissue immediately adjacent to the tumor capsule should only be employed if a vital neurovascular structure is at risk of injury, and under this circumstance marginal margins should only be utilized in the setting of adjuvant chemotherapy or radiotherapy. Wide margins are preferred and constitute at least 2 cm of tumor-free bone either side of the tumor in the longitudinal direction and at least one named soft tissue layer in the radial direction from the tumor-bearing bone. Radical margins that are seldom used necessitate resection of the entire tumor-bearing compartment, which in the case of the femur is the entire bone. The quality of the surgical margin is judged by the least adequate margin achieved. For example, a tumor resected with wide margins except for one location where the tumor was breached is regarded
as a contaminated wide margin which has the same effect as an intralesional or marginal margin only unless immediate remediation is undertaken with wide re-excision and copious intraoperative lavage (11,14).
as a contaminated wide margin which has the same effect as an intralesional or marginal margin only unless immediate remediation is undertaken with wide re-excision and copious intraoperative lavage (11,14).
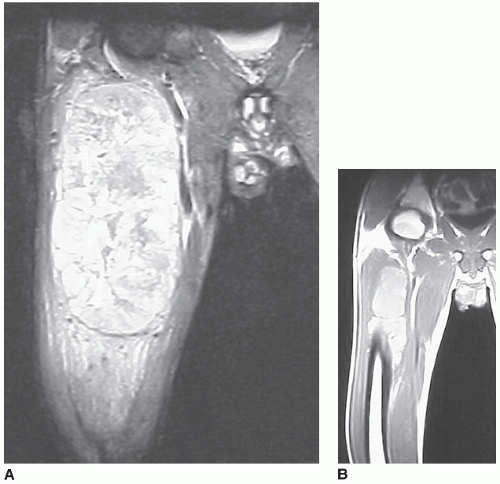
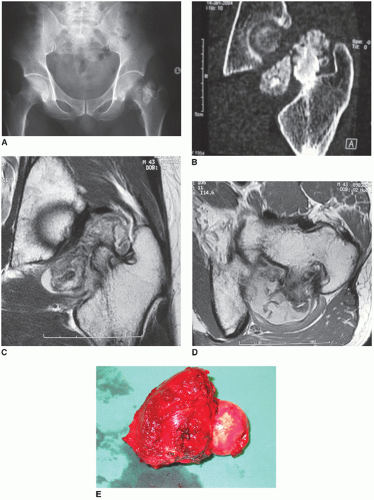
Resections of such large lengths of bone will inevitably impact on the surrounding soft tissue. Specifically, the abductor and extensor attachments are vulnerable to excision, which has obvious implications for joint function and stability. The tumor may alter following neoadjuvant therapy and the nature of this change has to be considered carefully prior to planning resection margins (16). For example, Ewing sarcoma is often characterized by a large soft tissue component with associated edema (Fig. 9.1A). Following neoadjuvant chemotherapy, there can be substantial reduction in the extent of the soft tissue component (Fig. 9.1B) such that the post-chemotherapy margins may not resemble the margins originally anticipated at the time of diagnosis. Further, the intraosseous extent of the tumor may also reduce quite markedly with chemotherapy, requiring less bone resection. In principle, an excellent response to chemotherapy as judged by complete reduction in tracer avidity on functional nuclear scans like positron emission tomography, or near-complete reduction in the size of the soft tissue component should allow a determination of the required wide surgical margin based on the post-chemotherapy imaging of the tumor. In contrast, a Ewing tumor with a poor response to neoadjuvant chemotherapy should always have its surgical margins determined on the pre-treatment imaging. As the periphery of an Ewing tumor is typically the site of the most viable cells, wide margins are mandatory. A similar approach can be employed for osteosarcoma. Chondrosarcoma, however, is not conventionally treated with chemotherapy or radiotherapy (Fig. 9.2A-D). Under this circumstance, wide margins should be planned from the outset based on the initial staging studies (Fig. 9.2E).
Secondary Malignancies of Bone
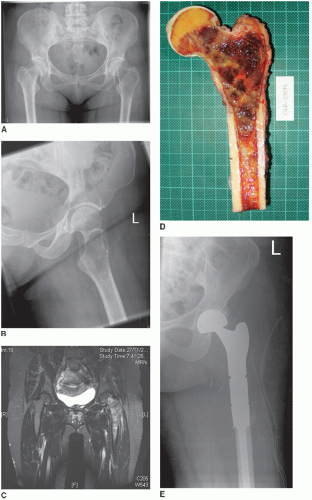
The commonest malignant tumor of bone is a metastasis from carcinoma. The likely primary carcinomas that metastasize to bone include the midline paired organs such as breast, lung, thyroid, kidney, and prostate. The femur is a common location for metastasis and surgeons are frequently called upon to consider the surgical management of an impending or completed fracture. Pain is a major feature of metastatic bone disease and surgery is an important option for management. Femoral resection is often only considered when the extent of tumor involvement or its likelihood to progress in a single site is so great as to make intramedullary rod fixation or internal plate and screw fixation impractical or perilous (Fig. 9.3A-E).
Isolated lesions are uncommon but may occur in relation to thyroid and renal metastases. Occasionally, late presentation of breast carcinoma metastases many years after the treatment of the primary may present as a solitary lesion. In all these cases, en-bloc resection may be attempted with locally curative intent. More often, however, disease arises in multiple sites within a single bone and any solution should seek to protect the entire bone. While the systemic treatment of bone metastasis has improved, its success is generally regarded as temporary
rather than curative. Therefore, in providing a surgical solution to metastatic bone disease, the expectation should be one of disease progression that compels a need for a durable reconstruction. Further, the longevity and status of the patient at the time of the surgery needs to be considered when planning an appropriate response to disease.
rather than curative. Therefore, in providing a surgical solution to metastatic bone disease, the expectation should be one of disease progression that compels a need for a durable reconstruction. Further, the longevity and status of the patient at the time of the surgery needs to be considered when planning an appropriate response to disease.
Complications of Hip Prostheses
Total hip arthroplasty has been one of the most successful procedures in orthopedics. Advances in prosthetic design and materials manufacture and a better understanding of tribology has permitted greater patient activity and improved prosthetic longevity. One of the key advances in arthroplasty has been the recognition of the need for improved revision techniques to address prosthetic complications such as loosening, periprosthetic fracture, dislocation, and infection.
Like the management of bone tumors, the complexity of proximal femoral reconstruction when revising failed hip joint arthroplasty arises when there has been absolute loss of significant amounts of femoral cortical bone or the quality of bone stock is too poor to accept a standard prosthetic replacement (8,9,10). This can be seen in gross loosening of a cemented prosthesis where motion of the prosthesis has caused expansile remodeling of the proximal femur, or migration of the prosthesis into a varus position with or without breach of the lateral cortex by the tip of the prosthesis, or markedly comminuted periprosthetic fractures. In all cases, conversion to a specialized megaprosthesis, enhancement of the native femur by allograft, or a combination of an allograft prosthetic composite (17,18,19




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree