7 Gait analysis in musculoskeletal conditions, prosthetics and orthotics
Total hip replacement
Total hip replacement (THR) is a common procedure to reduce pain and restore function in individuals with osteoarthritis of the hip. A total of 231 000 THR procedures were performed in the USA in 2006 (DeFrances et al., 2008). The majority of THR procedures (55%) were performed on individuals over the age of 65, while 40% of THR procedures were performed on individuals between the ages of 45 and 64 (DeFrances et al., 2008). The incidence of primary THR is projected to increase 174% to 572 000 by 2030, and THR revisions to increase 137% to 96 700 annually (Kurtz et al., 2007).
It is important that rehabilitation professionals understand the resultant gait abnormalities following THR. The majority of studies have been conducted 6–18 months postoperatively and have concluded that gait does not return to normal following THR. In support of these studies, a recent meta-analysis demonstrated that physical function along with walking speed only returned to approximately 80% at 6–8 months postoperatively compared with normal subjects (Vissers et al., 2011) and some research suggests that abnormal gait patterns may contribute to the implant loosening (Foucher et al., 2009).
Spatiotemporal factors
Several studies have reported significantly decreased gait speed, cadence, step length and stride length at 1 month (Nankaku et al., 2007), 1 year (Perron et al., 2000; Tanaka et al., 2010), and 10 years (Bennett et al., 2008) postoperatively. Although 1 month postoperatively may be too early to identify persistent gait deviations, Bennett et al. (2008) provided strong evidence that spatiotemporal parameters may never return to normal. Conversely Miki et al. (2004) and Nantel et al. (2009) reported that gait speed had returned to that of normal controls at 6 months and 1 year postoperatively. However, the mean ages in these studies were 49 and 52.6 years, respectively, which is younger than usual candidates for THR.
Kinematics
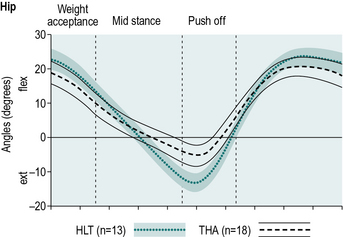
Several studies have observed decreased motion in the sagittal plane about the involved hip, attributing this decrease in range of motion primarily to decreased peak hip extension prior to push-off (Fig. 7.1) when compared with age-matched, healthy controls (Beaulieu et al., 2010; Bennett et al., 2008; Foucher et al., 2007; Perron et al., 2000). Bennett et al. (2008) and Perron et al. (2000) suggested that failure to fully extend the hip during late stance was correlated to decreased gait speed. Several studies have suggested that this decrease in hip extension may be linked to passive resistance or contracture in anterior hip structures (e.g., hip flexors) rather than hip extensor weakness (Miki et al., 2004; Nantel et al., 2009; Perron et al., 2000).
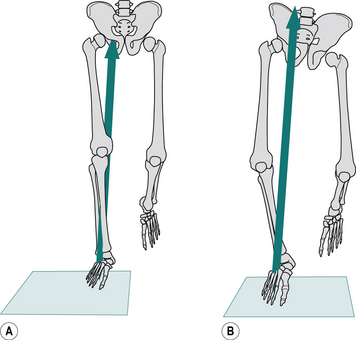
A significant increase in ipsilateral trunk lateral bending has also been observed during single limb support on the operated limb (Nankaku et al., 2007; Perron et al., 2000) along with decreased peak hip adduction angle (Beaulieu et al., 2010; Perron et al., 2000) when compared with age-matched, healthy controls. Both deviations are considered strategies to decrease demand on the hip abductors to stabilise the pelvis in the frontal plane during single limb stance by moving the centre of mass closer to the axis of rotation (i.e. the hip). Nankaku et al. (2007) concluded that lateral trunk bending led to increased energy expenditures. Beaulieu et al. (2010) also suggest that lateral trunk bending may be an attempt to improve balance.
Kinetics
Coupled with the changes in kinematics several changes in kinetics have also been identified. Perron et al. (2000) and Miki et al. (2004) observed a decreased internal hip extension moment during loading response, between 0 and 20% of the gait cycle, which correlated to the decrease in walking speed. This is consistent with the kinematic findings of decreased hip extension range of motion influencing gait speed, suggesting that hip extensor strength is an important factor in the return to a normal gait pattern. In addition, a decreased internal hip abduction moment during mid-stance also occurred, which suggests weakness in the hip abductors (Beaulieu et al., 2010; Foucher et al., 2007; Perron et al., 2000). However, it has not yet been confirmed whether this hip abductor weakness is due to disuse atrophy from pain avoidance strategies prior to surgery, or the effect of the surgery. The lateral surgical approach to THR does involve the detachment and repair of the gluteus medius, yet many of the subjects studied underwent the procedure using a posterior approach, which leaves the abductors intact (Beaulieu et al., 2010). Studies have also noted a decreased hip external rotation moment which may also be attributed to hip abductor weakness (Beaulieu et al., 2010; Foucher et al., 2009; Perron et al., 2000). This moment was identified as a significant determinant of peak implant twisting moment, which is critical for implant stability (Foucher et al., 2009).
Additional clinical relevance
Considering the longevity of the abnormal gait pattern and hip impairments a re-evaluation of current rehabilitation programmes of 2–3 months is warranted (Nantel et al., 2009). It has been suggested that long-term follow-ups (i.e. 6 months or 1 year) be performed with a goal of restoring normal gait pattern. Restoration of normal gait may help in preventing falls and reducing the risk of injury in more challenging activities (Nantel et al., 2009). Early and long-term intervention should focus on alleviating hip flexor tightness and strengthening of the hip extensors and abductors. Gait retraining may also be helpful in achieving a symmetrical and normal gait pattern, and potentially improve overall outcomes.
Key points
• A large increase in primary THR and THR revisions is expected over the next 20 years.
• The majority of studies indicate that gait does not normalise following THR.
• Rehabilitation should focus on improving hip extension flexibility, hip extensor and abductor strength, and symmetry of gait.
• Researchers suggest more long-term follow-up (i.e. 6 months or longer) to address persistent hip range of motion and strength deficits in efforts to normalise gait, decrease stresses on the implants and restore overall function.
Gait analysis in knee osteoarthritis
Jim Richards, David Levine and Doug Daniels
Peat et al. (2001) reported in an average population over the age of 55 years that 25% might have knee pain, with approximately 50% of these patients presenting with radiographic knee osteoarthritis. Knee osteoarthritis affects the medial compartment far more than the lateral compartment of the knee joint with an estimated 10:1 ratio between the occurrence of medial compartment to lateral compartment of the knee. This has been attributed to the mechanics of the knee in the coronal plane which shows between 60% and 80% of total load acting on the medial compartment during normal gait (Andriacchi, 1994; Baliunas et al., 2002; Hurwitz et al., 2002), and up to 100% of the load acting on the medial compartment in subjects with medial compartment knee osteoarthritis (Schipplein and Andriacchi, 1991).
The load distribution between the medial and lateral compartments is to be expected since medial compartment knee osteoarthritis is closely associated with a knee varus deformity, which gives rise to an external adduction moment at the knee throughout stance. The knee adduction moment is the product of the ground reaction force passing medial to the knee joint centre of rotation in the coronal plane. The knee adduction moment has therefore been used in many gait studies of knee osteoarthritis as an indirect measure of medial joint loading (Goh et al., 1993; Prodromos et al., 1985).
In a comparison of normal and medial compartment knee osteoarthritis adduction moments, Kim et al. (2004) found a significant difference in the adduction moment between the osteoarthritis group and an age- and gender-matched normal group, with the medial compartment knee osteoarthritis group having on average a 50% increase in their adduction moments (Fig. 7.2). Kim et al. (2004) also found a correlation between an increase in pain and decrease in function with an increase in knee adduction moment. Whether the knee starts in a varus position which leads to the adduction moment, which will then exacerbate the varus deformity, or whether the presence of an adduction moment causes the varus deformity is unclear. However, the importance of the varus deformity and knee adduction moment in the mechanics of medial compartment knee osteoarthritis is clear (Andriacchi, 1994; Crenshaw et al., 2000; Hurwitz et al., 1998).
Total knee arthroplasty
There is a high incidence of TKAs performed worldwide with 71 527 performed in England and Wales in 2008 (National Joint Registry for England and Wales, 2009), with prevalence expected to increase dramatically between 2005 and 2030 (Kurtz et al. (2007) project 3.48 million annually in 2030 in the USA). The goals of the surgery are to alleviate pain, and restore alignment, stability and range of motion of the knee to improve patients’ quality of life (Ranawat et al., 2005).
Kinematics
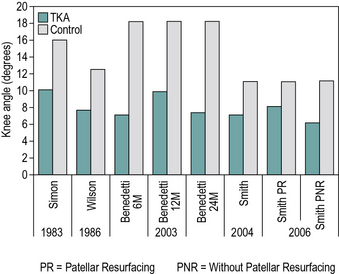
There have been multiple systematic reviews on the kinematics of the knee joint after total knee replacement. There is consistency among the literature that total (overall) knee range of motion is decreased in comparison to controls, with a reduction in the knee flexion during loading response (Milner, 2009) (Fig. 7.3). One systematic review found a range of 9.8–16.0° of knee flexion during the loading response for TKA patients versus 16.0–19.7° for controls (Milner, 2009). The same review found absolute differences of 3.0–11.2° in the range of motion between loading response and peak knee flexion during stance. Additionally, TKA patients often demonstrate reduced knee flexion during swing and usually have a greater knee angle at heelstrike (McClelland et al., 2007; Milner, 2009).
Kinetics
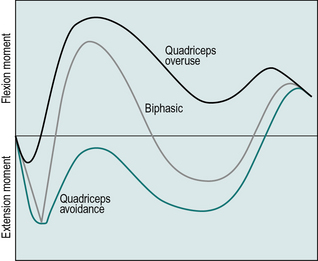
Kinetic changes at the knee joint have been measured after TKA, particularly in the sagittal plane. Normally, a biphasic moment pattern occurs during the stance phase of gait. An external moment across the knee, which causes extension, rapidly changes to a flexion moment, and then changes again to extend the knee and then flex the knee towards the end of stance (McClelland et al., 2007). Internal moments are generated by the leg musculature to counteract these external moments.
After TKA, this normal biphasic pattern is typically not present (McClelland et al., 2007). Depending on the alignment of the lower limb, a flexion moment or an extension moment may be present throughout the duration of stance. When an external flexion moment is present throughout stance, the quadriceps must generate the internal moment to a greater extent. This is termed the quadriceps overuse pattern. When an external extension moment is present throughout stance, there is an absence of quadriceps activity. This is termed the quadriceps avoidance pattern, which is typically discussed with regard to anterior cruciate ligament function (Timoney et al., 1993). Both patterns are common in the TKA population (Fig. 7.4) (McClelland et al., 2007).
The quadriceps avoidance pattern is clinically important as the hip or the ankle must compensate for the reduced knee extensor moment. Resultantly, studies have demonstrated that the hip extensor moment is typically increased in TKA patients compared with controls (Mandeville et al., 2007).
Additional clinical relevance
Quadriceps strength has been correlated with functional performance at both 3 and 12 months postoperatively. Yoshida et al. (2008) found that improved quadriceps strength resulted in significantly faster times in the timed up and go test, stair climbing test and 6-minute walk test (p< 0.05).
The available extension range of motion has been found to be a determinant of limb dominance during stance and walking. Harato et al. (2010) compared weight-bearing strategies of individuals with a diagnosis of bilateral arthritis that had undergone unilateral TKAs. Their findings suggest that patients who have sufficient extension range of movement (ROM) during stance utilise the operated lower extremity as the dominant side. However, patients with decreased extension ROM bear more weight on the contralateral limb, which could increase its rate of degeneration (Harato et al., 2010). One factor that could alter kinetics after TKA is patient weight, as compressive forces at the knee joint increase linearly with patient weight gain. One study found significant weight gain was common in the 2 years after total knee replacement. Specifically, 70 of 106 patients who had undergone a TKA gained an average of 6.4 kg (Zeni and Snyder-Mackler, 2010).
Mauer et al. (2005) compared the abilities of healthy age-matched controls to patients with bilateral TKAs in obstacle avoidance. The TKA group success rate in avoiding a suddenly appearing light band flashed on the floor was 30% less than controls. Clearly, this could lead to significant increases in fall risk and might be addressed in rehabilitation (Mauer et al., 2005).
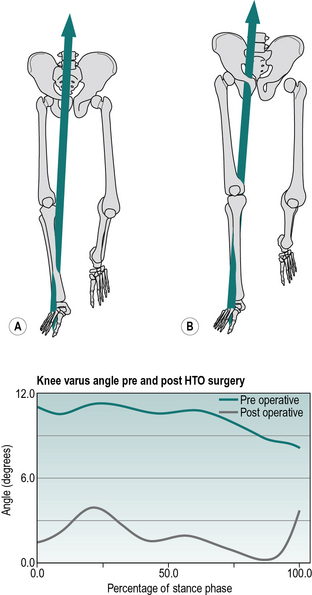
High tibial osteotomy
HTO is another surgical procedure to alter the bony alignment and reduce the varus angle of the knee joint. The aim of an HTO is to evenly share the load between the medial and lateral compartments of the knee. There are two main types of osteotomy for knee osteoarthritis, an opening wedge and a closing wedge. In an opening wedge, a cut is made in the tibia and the two sides are separated. The wedge-shaped space is filled with a bone graft. In a closing wedge, two cuts are made and a wedge-shaped piece of bone is removed. The two edges are then brought together creating the desired change angle. Both types of operation then require the bone to be fixed, usually with a plate and screws. HTOs are often seen as a way of delaying a total knee replacement in those considered too young. Prodromos et al. (1985) investigated the variable clinical results following HTOs for osteoarthritis of the knee with a varus deformity. They found that clinical success or failure could be predicted by the preoperative measurement of the frontal plane moment of force at the knee, those patients with a high moment having a significantly worse result, with a recurrence of deformity, than those with a low moment. Briem et al. (2007) studied the effects of the amount of valgus correction using HTO for medial compartment knee osteoarthritis. Their results showed that physical function improved significantly overall. However, those subjects whose knee alignment was further away from the group’s postoperative mean tended to improve less than those closer to the mean and have higher adduction moments 1 year after surgery. This again illustrates the importance of correct alignment during surgery and its relevance to adduction moments and clinical outcome scores.
As well as its use in comparative trials between two or more forms of treatment, gait analysis is also commonly used simply to quantify the benefit that a patient receives from a particular type of treatment. In such cases, a comparison may be made with pretreatment data values for that patient and with comparable results from normal individuals. Figure 7.5 shows an example of how the operation of HTO was successful in reducing the external adduction moment at the knee, and changing the varus alignment at the knee from 11° to 1.5°.
Conservative management of knee osteoarthritis
Conservative management of knee osteoarthritis includes weight loss, patient education, muscle strengthening, bracing (orthotics) and pharmacological intervention. All of these have been shown to be beneficial (Zhang et al., 2008). A recent study of a weight-loss programme in 157 obese patients with knee osteoarthritis decreased their body weight 13.5% in 16 weeks. This corresponded to a 7% reduction in knee joint loading, a 13% lower axial impulse, and a 12% reduction in the internal knee abductor moment (Aaboe et al., 2011). These findings and others (Messier et al., 2000, 2005) have shown that weight loss in obese adults can lead to improvements in function/gait and decreased pain and disability in patients with knee osteoarthritis. In addition, both patient education and muscle strengthening have been found to have positive effects on knee osteoarthritis in improving function, including gait (Zhang et al., 2008).
The aims of knee valgus braces are to unload the painful compartment, through bending moments applied proximally and distally to the knee joint, and reducing the varus deformity (Pollo, 1998). Several studies have been conducted into the use of valgus knee braces for medial compartment osteoarthritis, and have reported that patients experience significant pain relief and an improvement in physical function (Hewett et al., 1998; Kirkley et al., 1999; Lindenfeld et al., 1997; Matsumo et al., 1997; Richards et al., 2005) and also a reduction in medial compartment load (Jones et al., 2006; Pollo et al., 2002). The use of valgus bracing in the management of knee osteoarthritis has been a point of debate for some time. Two of the most important biomechanical outcomes measures are the varus angle and the knee adduction moment during loading response. Bracing has been shown to reduce the degree the varus deformity by 3° and reduce the knee adduction moment by 14.5%, providing significant pain relief (Jones et al., 2006).
Another treatment that has been suggested is the use of lateral wedging of the foot. A lateral wedged insole has a thicker lateral border and applies a valgus moment to the heel, attempting to move it into an everted position. Lateral wedging has been found to significantly reduce the peak adduction moment during early stance and reduce pain (Butler et al., 2007; Jones et al., 2006; Keating et al., 1993; Shimada et al, 2006; Toda et al., 2001), however, Kakihana et al. (2007) found some inconsistency in knee varus moment reduction caused by a lateral wedging in knee osteoarthritis in approximately 18% of patients tested.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree