CHAPTER 68 Fusion Surgery for Axial Neck Pain
INTRODUCTION
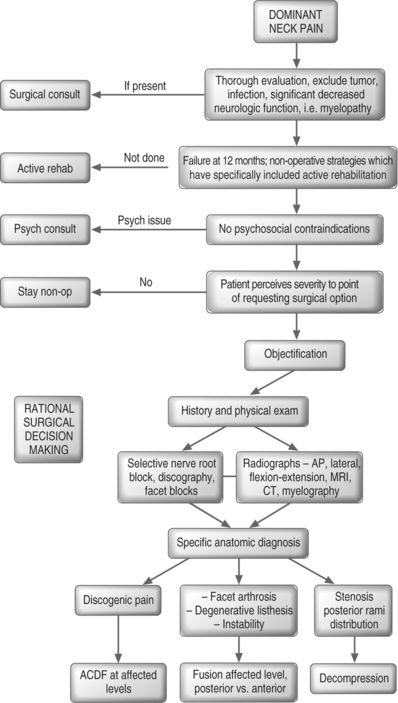
For those suffering from cervical radiculopathy or myelopathy, there is little debate that an anterior cervical discectomy and fusion (ACDF) is a viable treatment option.1–20 However, patients who present with their chief complaint being ‘neck pain,’ with or without referred or radicular symptoms, often are told that there is nothing that can be done surgically. This is wrong! The purpose of this chapter is to enhance the reader’s understanding of the surgical peer-reviewed literature, which leads to a rational decision-making process (Fig. 68.1). For many patients, that decision will be that surgical intervention is a reasonable option with a predictable statistical chance of success. The time-honored adage ‘that it is the decision, not the incision, which is most important,’ cannot be overemphasized.
INDICATIONS – PATIENT SELECTION
While covered in previous chapters, a brief review of the epidemiology and natural history of neck pain is in order. Prevalence studies have noted 35% of the general Norwegian population to have neck pain complaints within the preceding year, with 14% of respondents reporting those symptoms to have lasted longer than 6 months.21 In the Saskatchewan Health and Back Pain Survey, reported in 2000, it was documented that 54% of respondents had experienced neck pain in the preceding 6 months, with almost 5% perceiving themselves to be ‘highly disabled’ by their pain.22 When one looks at the literature of whiplash-associated disorders, it is apparent that while the majority of injured individuals do have spontaneous resolution of their symptoms, a small percentage, yet a significant number of human beings, do develop chronic neck pain.23,34
As with all medical ailments, it is important to appreciate the natural history of a condition. One approaches the patient with a ‘common cold’ with a vastly different sense of urgency than in comparison to an individual with suspected acute meningitis. We must then realize that in studies of natural history many with neck pain never seek out evaluation. Therefore, there is an inherent selection bias to more self-perceived impairment in those who seek out medical care. In an average 15.5-year follow-up study, Gore et al. reported on those presenting with neck pain.35 Seventy-nine percent of patients noted improvement with nonoperative care, with 43% reporting pain-free status and 32% continuing to report modest to severe pain. The severity of initial presenting symptoms, and the report of a significant injury, were more indicative of those with long-term complaints.
In a series of patients with neck-only, or neck and arm pain, DePalma et al. noted 45% of those treated nonoperatively to have satisfactory long-term outcome.36,37 In a surgical series report, DePalma et al. reported that at 3-month follow-up those presenting with dominant neck pain had 21% complete relief and 22% no relief with nonoperative care.36 At a 5-year follow-up time, Rothman noted 23% of patients continued to be partially or totally disabled due to significant cervical symptoms stemming from disc degeneration.36,38 In a review of those presenting with cervical radiculopathy, it was noted that while patients do not typically progress to myelopathy with nonoperative care, they often (two-thirds of the group) will have persistent symptomatology of some degree.39,40
The whiplash literature reveals a common pattern of a small group reporting persistent intrusive symptoms.23,34 In a textbook chapter, McNab and McCulloch summarized ‘about those who had suffered a whiplash injury, approximately 10–20% are left with discomfort of sufficient severity to interfere with their ability to do work and to enjoy themselves in leisure hours.’41 Thus, it must be acknowledged that while many who seek out medical care for neck pain will improve with nonoperative management, a finite low percentage of patients will still have symptoms of sufficient magnitude to cause them to seek out a surgical solution. It is for this group of patients that we need to have a rational surgical decision-making process.
OFFICE EVALUATION
History
When a patient presents for initial evaluation, we ask for their chief complaint, as this will focus our line of questioning and examination. In this chapter, we are concerned with those who complain of ‘axial neck pain.’ However, the typical patient does not say, ‘I have dominant axial pain;’ they state rather that they have neck pain, with or without arm pain. Patients who yield an ultimate diagnosis of myelopathy or radiculopathy will often present with a complaint of neck pain.8,40,42,43 It is up to the medical evaluation to elicit the historical features that will lead to a specific diagnosis.
I question about neurologic function. For myelopathy, I ask about generalized weakness, decreased fine motor dexterity, stumbling or ataxia, sphincter dysfunction such as urinary urgency, and paresthesias which may be nondermatomal. For radiculopathy, often a specific root pattern of numbness, pain, or specific weakness can be elicited. If these symptoms are present, they can help focus the differential to a specific cervical diagnosis. For psychosocial issues, we review the patient intake forms for depression, look for expectations of treatment, and solicit information about worker’s compensation status and litigation as these all may have a bearing on the patient-perceived pain. Specific psychologic treatment may be recommended. It is of interest that our last cervical fusion study did not correlate the presence of worker’s compensation or litigation with poor outcome.9
Physical examination
The physical examination should be straightforward. Range of motion is documented. If flexion hurts more than extension, think discogenic; if extension hurts more than flexion, think facet arthrosis or stenosis. If rotation or lateral flexion is preferentially limited to one side, it suggests a unilaterality of pathology. Spurling’s maneuver, i.e. lateral flexion, extension, and rotation which causes provocation of symptoms, suggests foraminal nerve root compression. If this reproduces the patient’s ‘neck pain,’ particularly into the upper trapezial or periscapular region, think nerve root pain. Assess the reflexes: hyperactive suggests upper motor neuron pathology, hypoactive suggests lower motor neuron pathology; and compare right side versus left side. Check for strength and sensation. If the examination documents pathology to suggest myelopathy or dense radiculopathy, the evaluation focuses on the neurologic deficit. An MRI or myelogram computed tomography (CT) scan should then be sought out. Often, those with dominant neck pain will have some component of arm symptomatology, just as those with ‘radiculopathy’ often have substantial complaints of neck pain.2,7,8,19,44,45
IMAGING
After a history is obtained and a physical examination is performed, one should start with basic radiographs. I prefer anteroposterior (AP), lateral, and flexion extension cervical spine radiographs. I do not routinely obtain an open mouth view or oblique views. One looks to exclude the obvious destruction of tumor and/or infection. We check for dynamic instability by the measurement of listhesis and angular deformity.43,46 We note obvious spondylosis by assessing disc space height, sclerosis, and osteophyte formation.47–49 While it is recognized that with increasing age there is an increasing presence of radiographic spondylosis, the films are helpful. If a young patient has multilevel spondylosis, we think less of a surgical approach; if a single level is involved, we think more of a surgical solution. If gross instability is seen, the patient needs to be counseled about the risks of nontreatment.
ADVANCED INVASIVE DIAGNOSTICS
Most often, the patient with axial pain will have several levels of degenerative change on an MRI study or noted on the X-rays. In those whose history and examination suggest a discogenic source, a discogram can be a very valuable tool. While the selection of this ‘older technology’ of discography still emotes controversy in some, I find it to be particularly useful in the surgical evaluation of those with axial pain. Data from our center has shown a statistical association with patient-perceived outcome.9 Numerous other authors have cited the utility of discography in patient selection.9,17,20,45,50–60
Most often, the MRI alone will not suffice. There are a substantial number of asymptomatic individuals who have MRI-documented pathology, which increases with age.60–63 In a prospective correlation of MRI and discography, in asymptomatic subjects and pain sufferers, Schellhas et al. concluded that MRI often misses annular tears and cannot reliably identify the source of discogenic pain.62 While many asymptomatic individuals had degenerative changes, only 3/40 discs studied in this group elicited a pain response, suggesting a high specificity and positive predictive value.62 Pragmatically speaking, the issue is, does the discogram yield information that reliably predicts outcome, and do published reports document this? The answer is yes, Table 68.1 documents such. What is hard to report upon is when the discogram keeps the patient out of surgery. For example, when every level hurts and there is no control, surgical intervention will not typically yield good results. The clean discographic surgical patient will have significant (greater than 6/10) concordant reproduction of pain at the affected level/levels, with little or no pain and normal appearance at the control level.9
Table 68.1 Outcomes of surgical treatment
| Author | Number of patients | Reported outcome |
|---|---|---|
| Zheng60 | 55 | 76% good or excellent, 18% fair, 6% poor |
| Garvey9 | 87 | 82% good or excellent, 16% fair, 2% poor |
| Ratliff54 | 20 | 85% satisfaction |
| Motimaya52 | 14 | 78.6% satisfaction |
| Palit53 | 38 | 79% satisfactory, 21% not satisfactory |
| Whitecloud19 | 34 | 70% good or excellent, 12% fair, 18% poor |
| Roth56 | 71 | 93% good or excellent, 1% fair, 6% poor |
| White46 | 28 | 62% good or excellent, 23% fair, 23% poor |
| Riley45 | 93 | 72% good or excellent, 18% fair, 10% poor |
| Simmons57 | 30 neck pain | 78% good or excellent, 15% fair, 7% poor |
| 51 neck and arm | ||
| William20 | 15 | 7% excellent, 20% good, 33% fair, 40% poor |
| Dohn50 | 34 | 62% good or excellent, 24% fair, 15% poor |
| Robinson17 | 56 | 73% good or excellent, 22% fair, 5% poor |
A selective nerve block can be useful in determining a surgical level. Such a patient may have neck, upper trapezial, and periscapular pain that increases with Spurling’s maneuver, has foraminal stenosis on MRI, and appears to have symptoms that are more often unilateral. In this patient, I often proceed to a selective nerve block. The selective nerve root block can be both diagnostic and potentially therapeutic. If in the first 30–60 minutes, during the lidocaine anesthetic phase, the patient reports significant diminution, i.e. 70–100% relief of typical pain, that specific nerve root is indicated as a primary pain generator. If steroids give long-term relief, all will be happy.64 If the patient has great relief with the selective nerve root block, unilateral pain, foraminal stenosis, and no instability, then a posterior laminoforaminotomy may be a favored option. If there is bilateral pain, and an additional ‘discogenic component,’ then one may proceed with an ACDF at the affected level.
True facet blocks or medial rami branch blocks are not uncommon in the work-up of patients with neck pain, particularly post-traumatic pain.24,65–68 To date, I know of no study to base fusion surgery on this diagnostic tool. Conceptually, one would think, if the patient had excellent temporary relief of the pain with this injection at a specific joint, that fusion of that joint may relieve the pain. If one were to use this intuitive reasoning to base the surgical decision, I would recommend that it be done in a study fashion with attendant IRB approval.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree