CHAPTER 9 Fractures of the Proximal Humerus
With regard to shoulder girdle injuries, proximal humerus fractures remain challenging in both their initial diagnosis and treatment. Proximal humerus fractures account for nearly 5% of all fractures,1,2 and incidence increases secondary to an aging population and associated osteoporosis.3–6 Nonoperative versus operative management of these injuries depends upon the mechanism of injury, the patient’s physiologic age including activity level, and fracture pattern.7 In general, proximal humerus fractures occur more in female patients than male patients (3 : 1 ratio), and the overall incidence increases with age.
Nearly three fourths of all proximal humerus fractures occur in patients older than 60 years, and they generally occur as a result of low-energy trauma such as a fall from standing height.7,8 A majority of these injuries are nondisplaced or minimally displaced and have a good overall prognosis with nonsurgical management.2,7 Specific risk factors associated with the development of proximal humerus fractures in the elderly include low bone density, impaired vision and balance, lack of hormone replacement therapy, previous fracture, three or more chronic illnesses, and smoking.7–9
In contradistinction to the elderly, younger patients generally sustain proximal humerus fractures during high-energy situations such as motor vehicle collisions, seizures, or electrical shock. These injuries tend to be more severe regarding soft tissue compromise and fracture displacement requiring operative intervention.2,7
ANATOMY
To appropriately manage proximal humerus fractures, it is crucial to understand the complex anatomy of the shoulder girdle. Stability and function of the glenohumeral joint is provided by an interaction of mechanisms that promote near global range of motion and purposeful function. Loads of increasing severity are initially offset by joint surface anatomy, joint volume, atmospheric pressure, and joint fluid cohesion and adhesion. Moderate loads are counteracted by the deltoid and rotator cuff, and larger loads are counterbalanced by capsulolabral structures and bone structure. Proximal humerus fractures alter these complex interactions, resulting in pain, decreased range of motion, and disability.10
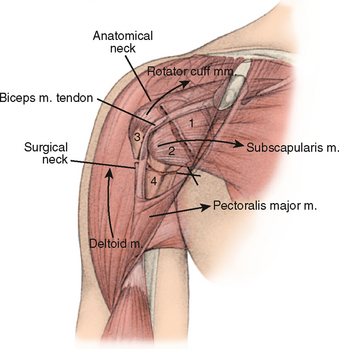
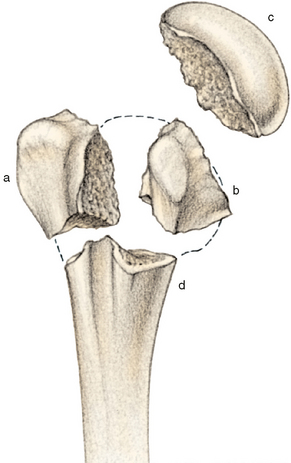
The proximal humerus consists of the humeral head, greater tuberosity, lesser tuberosity, and humeral shaft. Fractures of the proximal humerus occur in predictable patterns based upon the muscular insertions of the pectoralis major, subscapularis, supraspinatus, and infraspinatus (Fig. 9-1).10 The articular head is spherical and has a diameter of 37 to 57 mm.11,12 The most superior portion of the articular surface of the humeral head averages 8 mm above the greater tuberosity,11 and humeral version averages 29.8 degrees (range, 10-55 degrees).13 The head is inclined approximately 130 degrees with respect to the humeral shaft.12
The bicipital groove lies between the greater and lesser tuberosities and serves as a pathway for the long head of the biceps as it traverses from its intra-articular origin from the superior glenoid-labrum complex into the proximal arm.10 The distal aspect of the groove is internally rotated with respect to the proximal portion.14
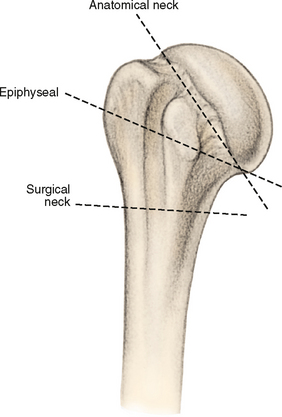
The anatomic neck of the proximal humerus is located at the junction of the articular surface and the tuberosities. The surgical neck represents an indistinct region (metaphysis) below the tuberosities but above the humeral shaft. There are direct implications regarding injuries to these separate locations, because injury to the former (anatomic neck) portends a poor prognosis with complete disruption of the vascular supply to the humeral head (Fig. 9-2).10
The glenoid is a convex structure of shallow depth shaped like an inverted comma. It articulates with the humeral head and serves as the attachment for the labrum and joint capsule.15
The acromion, the coracoacromial ligament, and the coracoid process form the coracoacromial arch, a rigid bony-ligamentous structure that imparts stability to the shoulder girdle (see Fig. 9-2). The rotator cuff, subacromial bursa, and subdeltoid bursa (synovial membranes) pass underneath the coracoacromial arch. Displaced proximal humerus fractures can impede normal movement of these structures, causing impingement and disruption of normal glenohumeral motion.10 In proximal humerus fractures, the subdeltoid bursa can thicken and become fibrotic. These adhesions can limit normal glenohumeral motion. Early range-of-motion exercises after a fracture have been hypothesized to decrease the formation of these adhesions.10
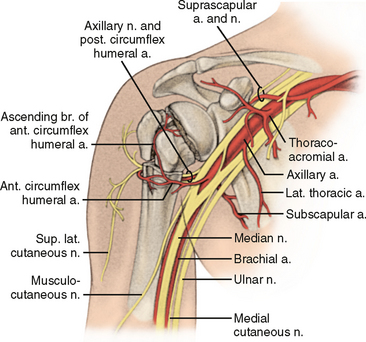
The proximal humerus receives its blood supply from the anterior and posterior humeral circumflex branches from the third division of the axillary artery. The posterior humeral circumflex artery travels with the axillary nerve, enters the quadrilateral space posteriorly, and anastomoses with the anterior circumflex branch, supplying the posterior cuff. The anterior humeral circumflex artery arises from the axillary artery at the inferior border of the subscapularis and provides the majority of vascular inflow to the humeral head by way of its terminal anterolateral branch known as the artery of Laing.10,16,17 This vessel courses parallel to the lateral aspect of the long head of the biceps and enters the humeral head at interface of the intertubercular groove and the greater tuberosity. Additional extraosseous collateral branches can permit humeral head perfusion despite complete ligation of the arcuate artery.18 Injury to the arcuate artery can result in osteonecrosis of the humeral head.16,17
Vascular injuries with proximal humerus fractures are uncommon (5%-6%). Most axillary artery injuries occur in patients older than 50 years, suggesting that comorbid conditions (e.g., arteriosclerosis) play a role in this increased incidence.19,20 Most axillary artery injuries occur at the level of the surgical neck, just proximal to the trifurcation of the anterior and posterior circumflex and subscapular branches.19,20 A careful neurologic examination must be performed in addition to the vascular assessment secondary to a high correlation between axillary artery injury and brachial plexus traction injuries.19,20
The brachial plexus (nerve roots C5-T1, with small contributions from C3 and C4 nerve roots) provides innervation to the shoulder. The most commonly injured nerve in proximal humerus fractures is the axillary nerve and it is most susceptible to injury during anterior fracture dislocations of the proximal humerus.21 The axillary nerve arises from the posterior cord of the brachial plexus (C5 and C6 nerve roots) and travels posterior to the surgical neck through the quadrilateral space with the posterior humeral circumflex artery, lying on the deep surface of the deltoid.
Previous anatomic studies documenting the course of the axillary nerve have demonstrated that the average distance from the proximal end of the humerus to the nerve is 6.1 cm (range, 4.5-6.9 cm), and the distance from the surgical neck of the humerus to the nerve is 1.7 cm (range, 0.7-4.0 cm).22 The nerve sends three distinct branches (including an articular branch) that provide innervation to the deltoid and teres minor. The lateral brachial (cutaneous branch) provides sensation to the overlying deltoid region (see Fig. 9-2).
The suprascapular nerve, the second most commonly injured nerve, originates form the upper trunk and supplies input to the supraspinatus and infraspinatus muscles. It is most susceptible to traction injury at two locations: the origin from the upper trunk and the suprascapular notch where the nerve passes underneath the transverse scapular ligament.21,23
The musculocutaneous nerve obtains neural input from C5, C6, and C7. It originates from the lateral cord of the plexus, passes through the conjoint tendon at a variable distance from the coracoid process (3.1-8.2 cm), and terminates into the lateral antebrachial cutaneous nerve, supplying sensation to the anterolateral forearm. Injury to the musculocutaneous nerve is a rare event, but it can occur with blunt trauma and traction injuries to the shoulder.24,25
Electromyographic studies should be completed at 3 weeks if clinical recovery is not apparent by physical examination. Documentation of motor denervation without improvement on additional studies might warrant surgical exploration for complete injuries at 3 months.7,21,23
MECHANISM OF INJURY
The most common cause of proximal humerus fractures is a fall on an outstretched hand from standing height (or less), particularly in patients older than 60 years.4,5,6–30 Less commonly, high-energy trauma such as motor vehicle accidents, falls from height, seizures, and electrical shock can occur in younger patients. These injuries tend to be more severe with regard to fracture pattern and soft tissue compromise.31–33 In the setting of metastatic bone disease or primary malignancy, a pathologic fracture can occur with minimal trauma.7
CLINICAL EVALUATION
Regardless of the age of the patient, a thorough history and physical examination should be performed. The history should include assessment of mechanism of action, velocity of the injury (associated injuries to ribs, cervical spine, and scapula), premorbid level of function, occupation, hand dominance, history of malignancy, and the ability to participate in a structured rehabilitation program.34 A review of systems should include queries regarding paresthesias, loss of consciousness, and ipsilateral elbow or wrist pain. On physical examination, the surgeon should look for swelling, soft tissue injuries, ecchymosis, and gross deformity. Most patients present with guarding, with the arm in internal rotation. Any attempts at active or passive movement elicit significant pain. Palpation of the shoulder reveals crepitus.7 A careful neurovascular assessment should include evaluation of the axillary nerve, brachial plexus, and axillary artery. Posterior fracture-dislocations can demonstrate flattening of the anterior aspect of the shoulder, with an associated prominence; anterior fracture-dislocations manifest with opposite findings.35 The surgeon should assume a vascular injury (even in the presence of a benign examination) with four-part proximal humerus fractures with axillary dislocation of the humeral head.7,18,19
IMAGING
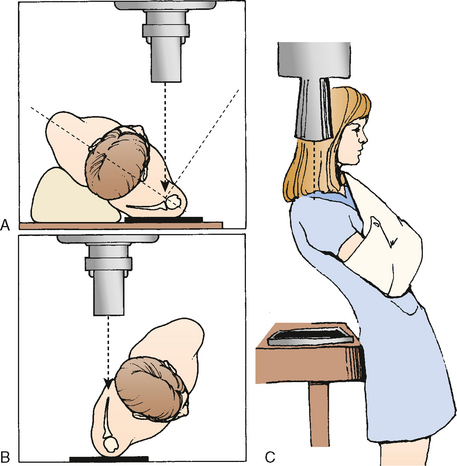
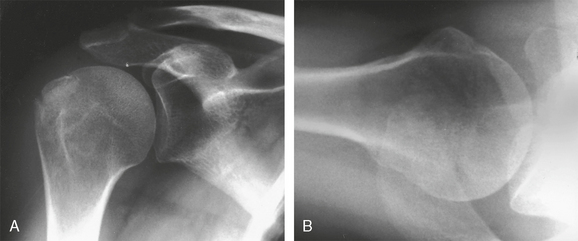
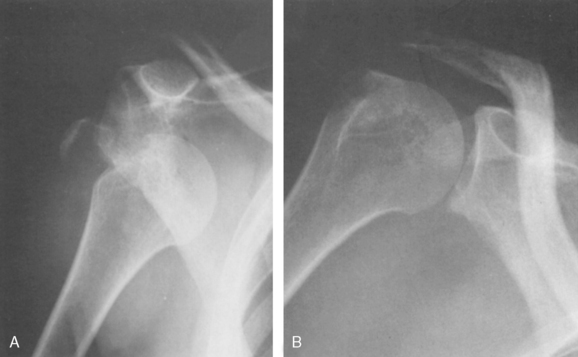
The true AP view may be taken with the patient’s arm in the sling and with the patient standing, seated, or prone. The glenohumeral joint does not lie in either the coronal or sagittal plane, and the glenoid is angled 35 to 40 degrees anteriorly. To obtain the true AP view, the unaffected shoulder must be rotated away 40 degrees, thus allowing the injured side to rest upon the x-ray plate (Fig. 9-3A).
The scapular Y lateral view is obtained by placing the anterior aspect of the affected shoulder against the x-ray plate with the unaffected side rotated out 40 degrees (see Fig. 9-3B). The axillary view is essential in evaluating the relationship of the humeral head to the glenoid, the displacement of the greater tuberosity, and the glenoid articular surface.36–38 This view can be obtained in the seated, standing, or prone position. The arm is gently held in 30 degrees of abduction with an x-ray plate placed on the posterosuperior aspect of the shoulder. The x-ray tube is directed cephalad from a level slightly below the plane of the patient.
Because of the nature of the injury, the patient may be unable or unwilling to participate in the abducted axillary view. The Velpeau axillary view is an excellent alterative and the preferred view in the trauma series (see Fig. 9-3C). The view is obtained by directing the x-ray beam from superior to inferior as the patient leans back over the x-ray cassette with the arm in a sling. Internal-rotation and external-rotation AP views can portray lesser or greater tuberosity fractures, respectively.7,20
Magnetic resonance imaging (MRI) is rarely indicated in the setting of an acute injury. If primary or metastatic disease from malignancy is a possibility, then MRI may be useful for staging of the disease. Computed tomography (CT) analysis may be helpful in evaluating tuberosity displacement, degree of comminution, and glenoid articular surface involvement.7,20,35
CLASSIFICATION
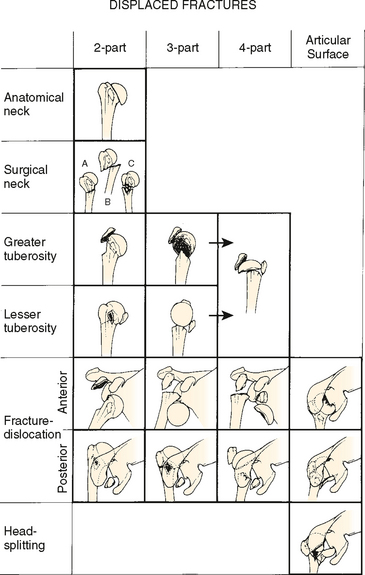
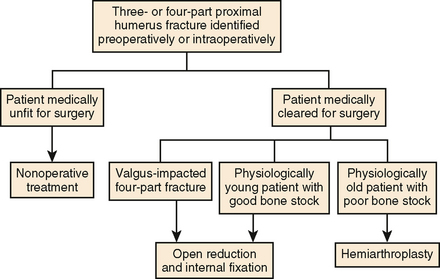
The most commonly used system is Neer’s four-part fracture classification, initially reported in 1970.39 Prior to Neer’s system, several persons attempted to classify these injuries according to fracture location (Kocher [Fig. 9-4]),40 fracture pattern (Codman [Fig. 9-5], De Anquin and De Anquin, and De Palma and Cautilli),41–43 and mechanism of injury (Watson-Jones, Dehne).44,45
Jakob and Ganz from the AO (Arbeitsgemeinschaft Osteosynthesefragen) group proposed a classification scheme involving 27 subgroups based upon articular involvement, location, and degree of comminution and dislocation, with special emphasis on the integrity of vascular supply. This system helped distinguish valgus impacted four-part proximal humerus fractures from other four-part injuries with partial preservation of vascular inflow to the articular segment through the medial capsule.46–48 The complexity of this system has generally precluded its routine use, despite similar intra- and interobserver reliability when compared to Neer’s classification.49
The intra- and interobserver reliability of the Neer classification system has been previously challenged, but it still remains the most reliable and commonly used system for assessment of proximal humerus fractures.50–55 The classification scheme is based upon four segments: the humeral shaft, articular surface, greater tuberosity, and lesser tuberosity, with emphasis on identifying fracture patterns associated with vascular injury to the humeral head (Fig. 9-6). Displacement of a segment occurs when the part (articular segment, greater or lesser tuberosity, shaft) has separated more than 1 cm or angulated more than 45 degrees. If this criterion is not met, the fracture is considered minimally displaced, even if multiple segments are involved.39
Some authors have attempted to improve the reliability of the Neer classification with CT scan augmentation, but they have demonstrated no evidence of decreased variability with this modality. The same authors have concluded that classification of proximal humerus fractures remains a difficult task, with reproducibility depending on the surgeon’s experience and level of expertise.50–58 Shrader and colleagues assert that the problem lies not with an understanding of the classification scheme but with the comprehension of the complex images.59
Hertel and colleagues have modified Codman’s original classification in order to evaluate the predictors of humeral head ischemia after intracapsular fractures of the proximal humerus. According to the authors, the most relevant predictors of ischemia were the length of the dorsomedial metaphyseal extension, the integrity of the medial hinge, and basic fracture pattern (Fig. 9-7).60 The combination of an anatomic neck fracture, short calcar (<8 mm of metaphyseal extension), and disrupted medial hinge demonstrated a positive predictive value of 97% when determining humeral head ischemia. Fracture displacement proved less important with regard to humeral head viability.
METHODS OF TREATMENT
The vast majority of proximal humerus fractures are minimally displaced or angulated and do not require surgical intervention.7,41,61–65 Early protection with gradual mobilization is the guiding principle with nondisplaced injuries. The patient generally wears a sling for 7 to 10 days with or without an axillary pad for comfort. The patient is encouraged to perform active finger, hand, wrist, and elbow exercises. By 2 weeks, active assisted range-of-motion and pendulum exercises may be initiated under the supervision of a physical therapist. Delay of motion beyond 2 weeks has deleterious effects on shoulder range of motion, pain, and function.66–69 Intermittent biplanar radiographs should be obtained to monitor interval fracture displacement or angulation. By 6 weeks, light-resistance shoulder exercises may be performed. Range-of-motion gains are generally noted between weeks 3 and 8.69
Approximately 20% of proximal humerus fractures are comminuted or displaced and can require surgical intervention by means of closed reduction with splinting, percutaneous fixation, open reduction with internal fixation, or humeral head replacement.7,43 In addition to the severity of the fracture, bone quality, rotator cuff status, patient’s physiologic age, activity level, and premorbid health status should be considered when deciding to pursue operative treatment. Patients with low demands and significant medical comorbidities (e.g., dementia) should be managed nonsurgically.68 The ideal goal of treatment, whether surgical or nonsurgical, is to re-establish functional pain-free range of motion.
Greater Tuberosity Fractures
Epidemiology
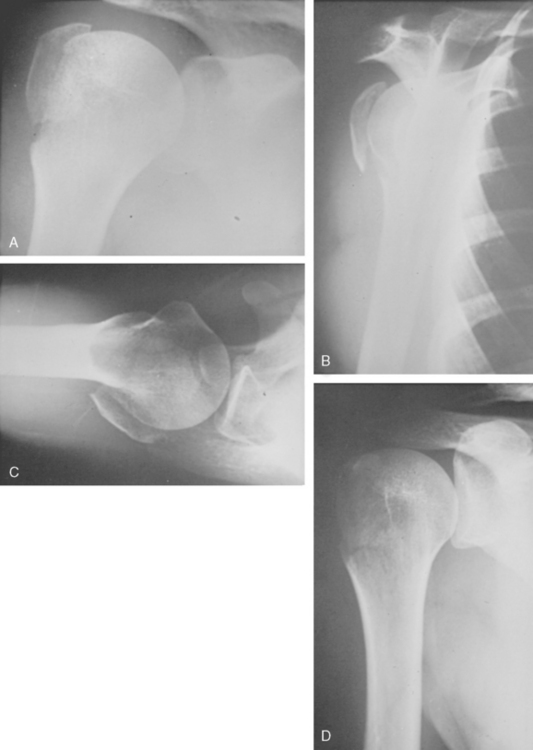
Isolated displaced fractures of the greater tuberosity account for a small percentage of proximal humerus fractures.70 Chun and colleagues, in their review of two-part proximal humerus fractures, recorded 26 out of 141 (18%) displaced greater tuberosity fractures.71 As an uncommon event, these injuries may be overlooked or trivialized by orthopaedic surgeons and other health care providers (Fig. 9-8).
Nature of the Injury
The amount of tuberosity displacement guides decision making regarding surgical intervention. In view of Neer’s criteria regarding displacement, most authors agree that the shoulder has little tolerance for greater tuberosity displacement. McLaughlin suggested that displacement of 5 mm or more can cause impingement and rotator cuff dysfunction.72 Park and colleagues have suggested that fractures in manual laborers or athletes with 3 mm of displacement should be reduced.73
Different mechanisms of injury have been proposed for greater tuberosity fractures, including impaction (fall onto shoulder in hyperabduction) or avulsion and shearing (anterior glenohumeral dislocation), though the pathomechanics have not been clearly elucidated.74
Peripheral nerve injury is the most commonly associated injury, occurring in nearly 33% of patients.75–77 Nearly 50% of patients older than 50 years who have an anterior proximal humerus fracture-dislocation demonstrate a peripheral nerve injury, and the axillary nerve is most commonly affected (Fig. 9-9).78,79
Evaluation
The initial evaluation of a patient with an injured shoulder includes a detailed history with a careful neurovascular examination. Radiographic evaluation should include the trauma series: true anteroposterior, scapular Y lateral, and axillary view. CT and MRI are not routinely used, though three-dimensional CT may be used to better delineate greater tuberosity displacement.70
Treatment
Nonsurgical
Nonsurgical treatment of nondisplaced and minimally displaced greater tuberosity fractures should be limited to low-demand patients. This treatment includes a brief period of sling immobilization for 1 to 2 weeks followed by passive motion. By 6 weeks, active range-of-motion and progressive strengthening exercises may be initiated.70
Surgical
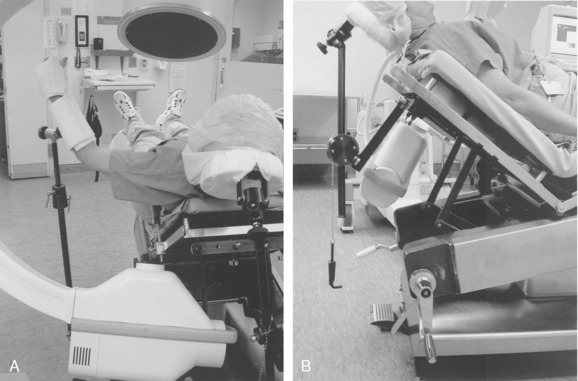
Operative intervention is deemed appropriate for greater tuberosity fractures with more than 5 mm of displacement.72 Patients are placed in the semi-sitting (beach chair) position under general anesthesia augmented by an interscalene nerve block for postoperative pain control. An articulated headrest and arm positioning device (McConnell, Greenville, Tex) is used with a standard operating table, with the patient’s affected shoulder placed over the edge of the table. A C-arm image intensifier may be used to obtain anteroposterior and axillary views (Fig. 9-10).
Surgical exposure for open reduction and internal fixation can proceed by way of a superior deltoid-splitting or deltopectoral approach. Some authors have advocated the use of the deltoid-splitting approach due to the relative ease in visualization of the greater tuberosity fragment. If necessary, an acromioplasty can also be performed with this technique.80 The deltopectoral approach avoids detachment of the deltoid and allows exposure of the surgical neck when there is a concomitant proximal humeral shaft fracture.
Screw and heavy suture fixation are two techniques used for internal fixation of greater tuberosity fractures. Isolated screw fixation is not recommended because the tuberosity can fragment or displace around the screw.70 Screws may be used as a post when placed distal to the fracture site, using sutures for tension band fixation. We recommend fixation with multiple sutures (e.g., No. 5 nonabsorbable) placed at the interface of the rotator cuff tendon and the tuberosity, with cortical approximation through distal bone tunnels through a figure-of-eight technique (Fig. 9-11). If there is an additional rotator cuff tear, this should also be repaired at the time of surgery.
Some authors have advocated percutaneous reduction with fixation to minimize soft tissue dissection, though fixation with a single screw or pin remains a disadvantage.81
Recovery
Postoperative rehabilitation begins the day after surgery with pendulum and passive forward-flexion and external-rotation exercises. Internal-rotation and adduction maneuvers are prohibited until 6 weeks. After 6 weeks, active range-of-motion exercises are initiated, with concurrent passive stretching exercises tolerated in all planes. Rotator cuff strengthening exercises are postponed until 10 to 12 weeks after surgery. All patients need to be informed that clinical improvement might not be maximized until 1 year.70
Osteotomy and mobilization of a malunited greater tuberosity fragment has unpredictable results, often requiring rotator cuff interval slides to reduce the fragment and the rotator cuff. Fixation of the mobilized tuberosity can prove tenuous due to significant osteopenia.
In the setting of nonunion, the tuberosity may be markedly displaced, making mobilization and repair difficult secondary to scarring.72,82,83
Follow-up
There are limited published follow-up data regarding surgical treatment of displaced greater tuberosity fractures. Jakob and colleagues84 treated 17 displaced greater tuberosity fractures but did not report the results of their treatment. Paavolainen and colleagues reported good results in the surgical treatment of six displaced fractures with screw fixation.85 Chun and colleagues treated 10 greater tuberosity fractures with open reduction and internal fixation (8 with screws). At a mean follow-up of 5.1 years, results were graded as (according to Neer’s criteria) excellent in 1 patient, good in 7, and fair in 3. The average active forward flexion and external rotation were 118 and 35 degrees, respectively.71 Flatow and colleagues reported their experience with surgical fixation of 16 displaced greater tuberosity fractures using heavy nonabsorbable suture. At 4.5 years of follow-up, the authors reported 6 excellent and 6 good results according to Neer’s criteria.80
Lesser Tuberosity Fractures
Isolated lesser tuberosity fractures without an associated posterior shoulder dislocation or surgical neck fracture is a rare event.86 Because of the subscapularis insertion, the lesser tuberosity fragment can displace medially in the event of an injury. If the fragment is small, minimally displaced, and does not block internal rotation, a short period of immobilization in slight external rotation is appropriate (Fig. 9-12).71,84,86,87
In the more common situation involving a posterior dislocation and lesser tuberosity fracture, closed reduction and immobilization is also appropriate if the fracture is addressed within 2 weeks of the event. Surgical intervention is warranted for displaced large tuberosity fragments and lesser tuberosity injuries with articular surface involvement.84,86,87 The tuberosity may be fixed either anatomically or into the base of the humeral head defect (reverse Hill–Sachs lesion) if the shoulder is unstable after open reduction.87
Surgical Neck Fractures
Epidemiology
Surgical neck fractures account for the majority (60%-65%) of proximal humerus fractures. Nearly 80% of these fractures are minimally displaced and warrant nonoperative management. Surgical indications include displacement, polytrauma, ipsilateral upper extremity injuries, vascular compromise, open fractures, and patient compliance with a postoperative therapy regimen.88 Malunion can be tolerated fairly well if the tuberosity and articular surface relationships are not distorted.
As Iannotti and colleagues have suggested, there are two distinct patient populations: young, male patients with high-energy trauma and elderly, female patients with low-energy trauma. These should be treated differently even with the same fracture pattern.88 The young patient typically has good bone quality and can generally comply with postoperative therapy, allowing the surgeon to employ surgical methods such as open reduction and internal fixation. The elderly patient might not fully understand or appreciate her role in the postoperative rehabilitation process. Bone quality in elderly patients tends to be poor, with evidence of comminution after minor trauma. Fixation options may be limited, and in some cases, hemiarthroplasty may be a more viable option.88
Evaluation
The amount of displacement is critical when assessing nonoperative versus operative treatment for surgical neck fractures (Fig. 9-13). In the elderly patient, bony contact of fracture segments may be all that is necessary for a functional result. In active patients, less than 50% shaft diameter displacement and less than 45 degrees of angulation may be tolerated.20 Varus deformity, valgus deformity, comminution, and 100% displaced surgical neck fractures are unstable and require surgical intervention.
Treatment
If the initial evaluation reveals a displaced fracture (<50%) without impaction, a closed reduction maneuver may be performed under conscious sedation or hematoma block. Because of the deforming force of the pectoralis major muscle, the arm should be adducted and flexed to 90 degrees. While in this position, a posterolateral translation force is applied in conjunction with longitudinal traction to promote impaction of the shaft and humeral head–tuberosity segments. If the maneuver is not successful, the surgeon should suspect that interposed soft tissues such as muscle, capsule, or the long head of the biceps are preventing the reduction.20 If manipulation is successful, sling immobilization is performed, with weekly examination and radiographs. Two-part surgical neck fracture-dislocations may similarly be treated with immobilization if the fragments are minimally displaced following reduction of the glenohumeral joint.
Management of surgical neck fractures depends on fracture displacement, bone quality, functional demands of the patient, and mental status of the patient. Closed reduction with immobilization is generally reserved for patients with minimally displaced or less than 50% displaced surgical neck fractures who can participate in a rehabilitation program. Not all of these patients do well; Chun and colleagues reported 55% good or excellent results in 56 surgical neck fractures treated nonoperatively with a mean forward flexion arc of 104 degrees.71 Displaced fractures in active patients should undergo open reduction with internal fixation. An alternative option, though tedious and technically difficult, may be percutaneous fixation after closed reduction. The main advantage to this technique is the lack of soft tissue dissection, which can theoretically minimize the risk of iatrogenic injury to the vascular supply of the articular segment.88
Three-Part Fractures
In three-part fractures, cleavage lines occur through the surgical neck and the greater or lesser tuberosity. Degree of displacement of the segments depends largely on the deforming forces of the rotator cuff muscles. The greater tuberosity is more commonly involved than the lesser tuberosity and is usually displaced into a posterior and superior position by the pull of the attached supraspinatus, infraspinatus, and teres minor.88,89 The humeral head is pulled into internal rotation secondary to the subscapularis, while the humeral shaft is displaced anteromedially due to the insertion of the pectoralis major. If the fracture involves the lesser tuberosity, the subscapularis pulls the segment medially. The intact greater tuberosity and articular surface segment are pulled into adduction and external rotation, and the humeral shaft is similarly pulled in an anteromedial direction. Surgical treatment options include closed reduction, closed reduction and percutaneous fixation, open reduction with internal fixation, intramedullary fixation with suture supplementation, and hemiarthroplasty.
Nonoperative management of three-part fractures should follow the same principles that guide treatment of minimally displaced fractures. Closed reduction may be attempted in the medically unfit patient, but it is often unsuccessful secondary to rotatory instability and degree of displacement. Multiple attempts at closed reduction should be avoided to prevent further displacement, fragmentation, and soft tissue injury.20,88–90 If the reduction is successful, the patient should be placed in a sling for 7 to 10 days followed by physical therapy when the patient can tolerate motion.
Neer in 1970 initially reported his experience in 39 patients with three-part proximal humerus fractures treated by closed reduction. Only 3 patients demonstrated a satisfactory result by his criteria. Poor results were due to malreduction, nonunion, humeral head resorption, and osteonecrosis. He concluded that nonoperative intervention for these injuries was inadequate in active patients.39 More recent studies by Lill and colleagues91 and Zyto and colleagues92,93 suggest that good functional outcomes after nonsurgical management of these injuries may be achieved. Zyto prospectively evaluated 40 patients with displaced three- and four-part proximal humerus fractures randomized to nonoperative management or tension band fixation. At 3 to 5 years of follow-up, he found no differences in functional outcome between the two methods, despite radiographic evidence revealing improved position of the humeral head in the surgical patient.93
The majority of three-part proximal humerus fractures require operative fixation or hemiarthroplasty due to the residual humeral deformity and functional deficits that can prevent the patient from returning to premorbid level of activity (Fig. 9-14).
Four-Part Fractures
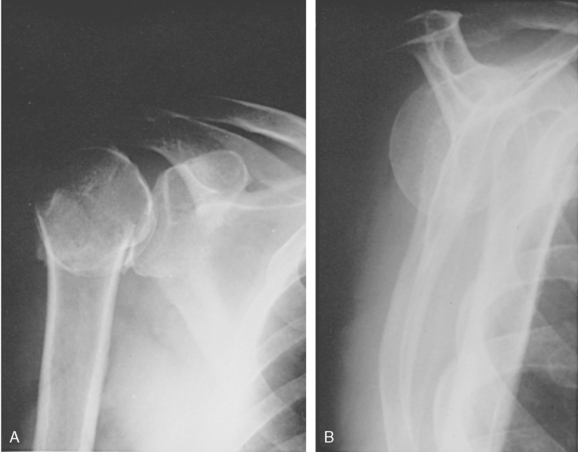
Nonsurgical management of four-part proximal humerus fractures should only be employed in the medically unfit patient. Because of the poor outcomes and high incidence of complications (osteonecrosis, malunion, nonunion, and post-traumatic arthritis) associated with nonoperative treatment, most fractures are treated surgically.91,94 Options include closed reduction, open reduction with internal fixation, and hemiarthroplasty.
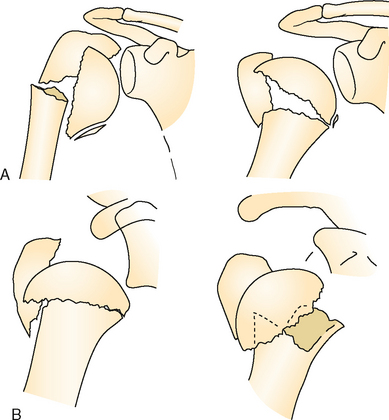
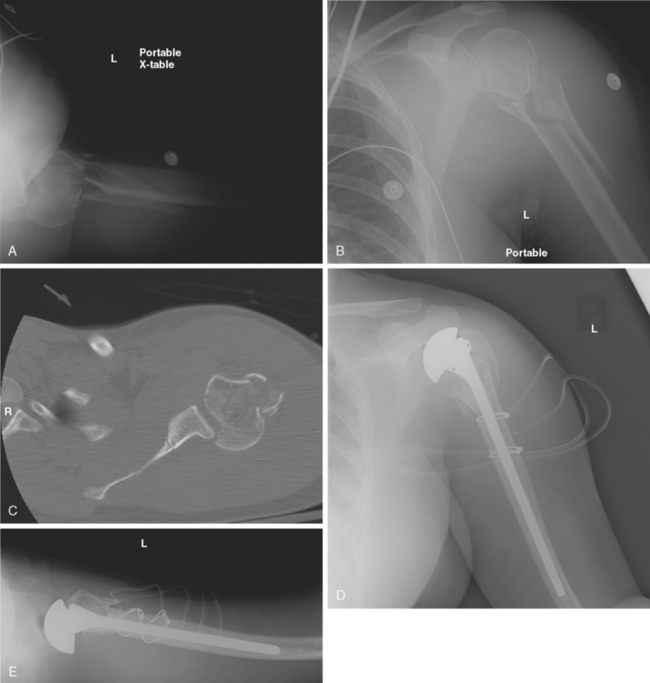
The impacted valgus four-part fracture is an uncommon but important subtype to identify.47,84,95–98 This injury has a more favorable prognosis when compared to other multipart proximal humerus fractures secondary to the integrity of the medial capsular blood supply.97,98 The fracture pattern is characterized by impaction of the lateral aspect of the humeral articular surface due to a fracture of the anatomic neck (Fig. 9-15).95–98 The articular surface faces superiorly toward the acromion rather than the glenoid. The tuberosities typically displace secondary to impaction of the articular surface on the humeral metaphysis. The prevalence of osteonecrosis approaches 5% to 10%, much less than the corresponding standard four-part proximal humerus fractures.47,95,96,98,99
Surgical treatment options include early mobilization, percutaneous reduction with internal fixation, and hemiarthroplasty.88 Nonoperative management is reserved for elderly and sedentary patients with medical comorbidities that prevent intervention. Percutaneous reduction with internal fixation is a viable option for acute injuries (<7-10 days old) with good bone stock and minimal comminution. Open reduction is generally performed for fractures not amenable to reduction by closed means, for fractures with comminution, and for injuries that are 10 days to 4 months old.
Jakob and colleagues achieved a satisfactory outcome in 74% of the patients in his study who underwent closed reduction or limited open reduction with internal fixation. The major reason for failure was avascular necrosis, which occurred in five cases (26%).47 Resch and colleagues performed limited open reduction and internal fixation on 22 patients with four-part valgus-impacted fractures, demonstrating no evidence of osteonecrosis at a mean follow-up of 36 months (minimum, 18 months). Results were graded as excellent, particularly in cases in which anatomic reduction was maintained (12 of 22).98
Hemiarthroplasty is reserved for the elderly and sedentary patient with poor bone stock.88
Proximal Humerus Fracture-Dislocations
Two-part fracture dislocations are amenable to open reduction and internal fixation due to the integrity of the vascular supply that is maintained by the soft tissue attachments to the intact tuberosities.20 Three-part and four-part fracture-dislocations with articular surface involvement similarly require operative intervention. Repeated attempts at closed reduction or delayed open reduction and internal fixation can result in an increased incidence of myositis ossificans.7 Results of internal fixation for four-part proximal humerus fracture-dislocations are poor, and hemiarthroplasty serves as the appropriate treatment method for these injuries (Fig. 9-16). Closed management should only be considered in the medically moribund patient.
AUTHORS’ PREFERRED METHOD OF TREATMENT
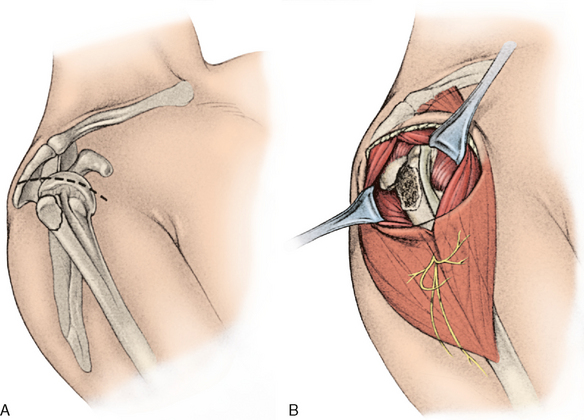
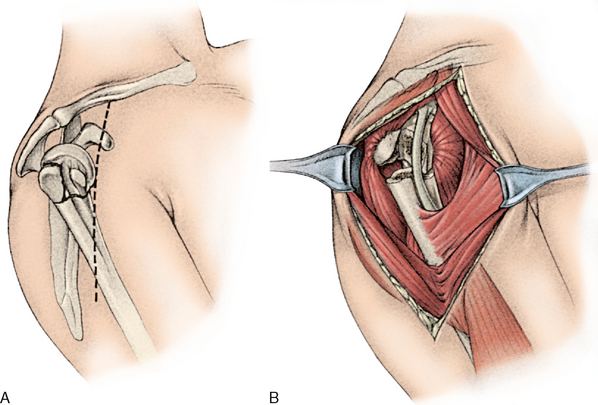
There are two basic surgical approaches that can be used to treat proximal humerus fractures. The superior approach to the shoulder involves a skin incision made in Langer’s lines just lateral to the anterolateral aspect of the acromion (Fig. 9-17A). The deltoid can be split from the edge of the acromion distally for approximately 4 to 5 cm, but, to protect the axillary nerve, the split should not be extended (see Fig. 9-17B).7,20,88 The deltoid origin is not removed during exposure of the superior aspect of the proximal end of the humerus. This approach is useful for internal fixation of greater tuberosity fractures and is helpful for intramedullary fixation of two-part proximal humerus fractures. Rotation, flexion, or extension of the humerus can allow exposure of the underlying structures for appropriate reduction and internal fixation.7,20,88
The workhorse approach is the deltopectoral approach (Fig. 9-18A). In this technique, both the deltoid origin and insertion are preserved. The skin incision begins just inferior to the clavicle and extends across the coracoid process and down to the region of insertion of the deltoid. The cephalic vein should be preserved and retracted laterally with the deltoid. The deltopectoral interval is dissected proximally and distally (see Fig. 9-18B). If more exposure is needed, the superior 50% of the pectoralis major tendon insertion can be divided. This approach is useful for internal fixation of two-part surgical neck fractures and for hemiarthroplasty of three-part and four-part fractures.7,20,88
Nondisplaced or Minimally Displaced Proximal Humerus Fractures
Nondisplaced and minimally displaced fractures are treated with a sling for comfort. Elbow, wrist, and hand exercises are encouraged during the initial immobilization period. If the fracture is stable, range-of-motion exercises may be started within 10 days, if the pain is tolerable. The physician can evaluate the fracture for gross stability by manipulating the elbow and forearm with gentle rotation while palpating the proximal humerus with the other hand. If the entire humerus appears to move as a unit, then the fracture is stable, and gentle passive range-of-motion exercises may be started. It is important to have the patient begin exercises within 14 days of the date of injury to avoid late sequelae such as stiffness, limited activities of daily living, and a poor functional outcome.67 Weekly radiographic evaluation is needed to check for displacement of fracture fragments.67
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree