Chapter 22 Fractures of the Olecranon and Complex Fracture–Dislocations of the Proximal Ulna and Radial Head
Background/aetiology
The elbow is one of the most congruous joints in the body and is subsequently one of the most inherently stable.1,2 Elbow stability is conferred both by the conforming geometry of the articular surfaces and soft tissue stabilizers.1–3 The semilunar notch imparts intrinsic stability to the ulnohumeral articulation, with the coronoid and olecranon processes acting as buttresses to prevent anterior and posterior displacement. The sagittal geometry of the semilunar notch is that of an ellipse rather than a semicircle, due to the transverse ‘bare area’ located between the coronoid and olecranon processes. This must be appreciated when approaching reconstruction of the ulnohumeral articulation because direct apposition of the hyaline cartilage surfaces will result in over-compression of this region and, consequently, an incongruous joint.
The coronoid and olecranon processes act to prevent trochlear subluxation. Since up to 80% of the length of the proximal olecranon can be resected,4 primacy must be given to the coronoid as the most important articular stabilizer.
The triceps, as well as the biceps and brachialis, create a posteriorly directed force vector with a resultant tendency for the elbow to sublux posteriorly with active contraction. An anterior buttress is required to prevent posterior joint dislocation. This buttress is composed of both the coronoid process and the radial head. The greatest threat to ulnohumeral stability occurs when both the coronoid and radial head are fractured. Biomechanical studies have demonstrated that at least 50% of the coronoid is necessary to achieve functional stability as the ulnohumeral joint nears extension, regardless of the integrity of the other articular elements. With an intact radial head, 75% of the coronoid can be removed, and the elbow is still stable to within approximately 30° of full extension.2 Therefore the radial head should be reconstructed or replaced for all complex elbow fractures and fracture dislocations with associated Mason type II and III fractures.
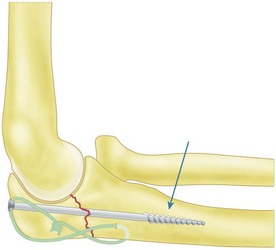
Osseous anatomy is also important when developing a fixation strategy. The olecranon consists of a relatively thin dorsal cortical shell, 1–2 mm thick, surrounding a bulbous mass of cancellous bone.5 The dorsal cortex increases in thickness distal to the coronoid process, or approximately 35 mm from the tip of the olecranon. It is essential to gain purchase in this region of the ulna to maximize the rigidity of fixation when treating olecranon fractures. It is also desirable to obtain screw purchase in the anterior cortex at the base of the coronoid process. The longitudinal axis of the ulna must also be kept in mind. The medullary canal follows a serpentine curve. Baratz and Shanahan5 have shown that a 6.5 mm screw would not engage the cortex with three-point fixation until it is at least 55 mm from the tip of the olecranon (Fig. 22.1). At 65 mm from the tip of the olecranon, it became difficult to advance the screw, as the diameter of the medullary canal decreases to 5.5 mm. Therefore, care must be taken to hand tap the distal medullary canal, particularly in osteoporotic bone, to avoid distal cortical compromise.
Soft tissue plays a crucial role in the pathoanatomy of proximal ulna fractures. This is particularly true with increasing fracture complexity, and especially when associated with ulnohumeral or radiocapitellar dislocations. The primary static restraints are the medial collateral (MCL) and lateral ulnar collateral ligaments (LUCL). The medial collateral ligament is the primary stabilizer to valgus stress, the anterior band being the most critical. The MCL originates from the antero-inferior surface of the medial epicondyle and inserts at a mean of 18 mm distal to the coronoid tip near the sublime tubercle.3 The LUCL complex is important for resisting varus stress and providing posterior rotatory stability to the elbow. The LUCL originates on the distal aspect of the lateral epicondyle and inserts onto the annular ligament and the tubercle of the supinator crest.3 Dynamic forces acting on the elbow include the triceps, biceps and brachialis. The triceps inserts onto the posterior third of the olecranon and proximal ulna. It is intimately associated with the ulnar periosteum and sends fascial expansions both medially and laterally that blend into the anconeus aponeurosis, common extensor origin and the fascial envelope of the proximal forearm. The biceps inserts onto the radial tubercle and contributes primarily to forearm supination, but also plays a role in elbow flexion. The brachialis inserts broadly on the midportion of the anterior aspect of the coronoid and proximal ulnar metaphysis. Besides generating the posteriorly directed force vector that contributes to posterior subluxation, the triceps, brachialis and biceps muscles generate forces that displace the fracture fragments. Resisting this tendency to displacement and instability are the medial and lateral expansions of the triceps fascia, as well as the MCL and LUCL. Once torn, bony fragments are then free to separate and displace. Negation of these displacing forces is necessary to achieve stable fixation.
Olecranon fractures are relatively common, accounting for about 20% of all proximal forearm fractures.6 Owing to its superficial location, the ulna is particularly susceptible to direct trauma, but injuries to the olecranon can also result from indirect trauma, or combinations of both direct and indirect trauma. Most olecranon fractures are intra-articular, due to the unique osseous anatomy of the proximal ulna.1 The majority of fractures occur in older patients and are related to poor bone quality and osteoporosis. When these fractures occur in younger patients they are typically due to higher energy and/or direct trauma. Displaced fractures of the ulnohumeral joint threaten to compromise stability. The mechanism of injury may be due to a fall from standing or a fall from a height, motor vehicle accident, sports or an assault.6 Indirect trauma is typically due to a fall on the outstretched hand with the elbow bent. Forceful contraction of the triceps usually causes a transverse or short oblique fracture of the olecranon. Direct trauma causes the ulna to be impacted into the distal humerus, resulting in articular impaction and/or comminution.
Presentation, investigation and treatment options
Patients with an olecranon fracture typically present with pain and swelling about the elbow. Although most olecranon fractures are isolated injuries, a careful history and physical examination are an essential part of the evaluation. The mechanism of injury and patient symptoms will add important information: whether the injury was direct, indirect or a combination, the amount of energy involved in the trauma, and what types of other injuries are also present. The physical examination will provide detailed information on the severity of the injury and any associated injuries. Associated injuries usually involve the ipsilateral extremity but can involve other areas, particularly if the fracture is a high-energy injury. Wolfgang et al7 reported a 20% incidence of concomitant injuries, including long-bone fractures, skull fractures, splenic and pulmonary injuries, and axillary artery rupture.
The physical examination should thoroughly evaluate the patient, particularly the ipsilateral upper extremity. Evaluation of the ipsilateral clavicle, shoulder, humerus, elbow, forearm, wrist and hand is essential. The upper extremity evaluation should begin with an inspection of the skin as open fractures of the olecranon have been reported in up to 31% of cases.7 The elbow is usually swollen with a haemarthrosis. The subcutaneous position of the olecranon allows easy palpation of the fracture with tenderness at the fracture site and in significantly displaced fractures a defect in the bony contour. Typically, patients will have significant pain with active and passive elbow movement. However, if patient comfort allows, testing triceps function will often show a loss of active elbow extension. The integrity of the radial, median, ulnar and posterior interosseous nerves should be evaluated and palpation of the radial and ulnar pulses documented.
A complete radiographic analysis is essential for fracture evaluation and preoperative planning. A standard elbow series, including anteroposterior (AP), lateral and oblique views, are usually sufficient to characterize the fracture. A radiocapitellar view can also be included if there is sufficient concern that there is a radial head fracture that has not been appreciated on the standard views. It is important to ensure that the radiographs obtained are adequate and, if necessary, the treating surgeon may need to supervise or assist in positioning the patient to obtain true AP and lateral radiographs of the elbow. Additionally, if the patient cannot extend the elbow sufficiently to obtain an adequate AP radiograph, it may be worthwhile to obtain an AP of the distal humerus and a separate AP of the proximal forearm. A CT scan is usually unnecessary for evaluation of the majority of olecranon fractures. However, with complex transolecranon fracture–dislocations, more information may be required regarding the integrity of the radial head and/or coronoid, particularly if it will influence treatment. In these cases a CT scan, including a three-dimensional reconstruction with the distal humerus removed, can be particularly useful for identifying fracture fragments and improving preoperative planning. In most other cases, intraoperative imaging with an image intensifier will provide any additional information required for appropriate treatment. One final radiographic finding that is worth looking for is a small fleck of bone posterosuperior to the tip of the olecranon seen on the lateral radiograph. This may indicate a triceps avulsion injury. Alternatively, the appearance may be due to a patella cubiti, which is an accessory ossicle in the triceps tendon.8,9 Patella cubiti are usually bilateral and if this diagnosis is suspected radiographs of the uninjured elbow should be undertaken.
Numerous classification systems have been proposed for olecranon fractures. These include the Colton, AO, Mayo and Schatzker classification schemes.1,6,10,11 However, none of these classification systems has been universally accepted. A classification system should aid in communicating results, determining treatment and predicting outcome. Unfortunately, comprehensive fracture descriptors become unwieldy or less than adequate when complex fractures, potentially including the radial head, coronoid and soft tissue restraints, are considered. Additionally, the various classification systems are subject to inter-observer variability. Nevertheless, a working knowledge of the classification systems is important for understanding the literature, evaluating radiographs for preoperative planning, predicting outcomes and communicating results.
The AO/OTA classification system combines both radial and ulnar fractures into three broad categories.6 Type A fractures are extra-articular, with A1 fractures involving only the ulna. Similarly, type B fractures are intra-articular fractures and B1 fractures involve only the ulna. Type C fractures include all intra-articular fractures that involve both the radius and ulna. Although fairly comprehensive, the classification system can be difficult to remember, does not provide a significant amount of help regarding treatment and does not address fracture-dislocations.
The Mayo classification describes the fractures based on the degree of displacement, comminution and elbow stability.1 The type of fracture can help determine whether treatment should be surgical or non-surgical, while the subgroups guide the type of fixation required. Type I fractures are undisplaced/minimally displaced, and either non-comminuted (type IA) or comminuted (type IB), and can be treated non-operatively. Type II fractures are displaced but the elbow remains stable – these fractures require surgical intervention. Type IIA fractures are non-comminuted and are usually amenable to tension band fixation but may require supplemental fixation and/or plate fixation if there is significant obliquity to the fracture. Type IIB fractures are comminuted and require plate fixation with or without supplemental interfragmentary fixation. Type III fractures are associated with elbow instability and require surgical intervention. The olecranon can be non-comminuted (type IIIA), but is more likely to be comminuted (type IIIB), and is often associated with a radial head fracture.
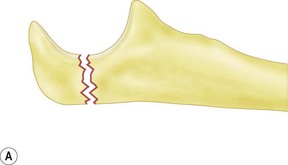
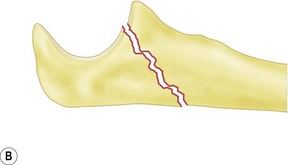
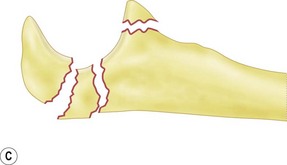
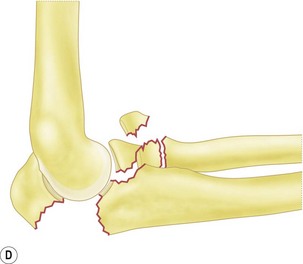
Schatzker’s classification of olecranon fractures implies mechanical considerations related to the type of internal fixation required.11 Thus the choice of internal fixation is based upon the fracture pattern. There are six major fracture types in this classification: Type A fractures are simple transverse; type B are transverse with impaction of the central portion of the articular surface; type C are simple oblique; type D are comminuted; type E are distal oblique; and type F are transolecranon fracture–dislocations which are often associated with a radial head fracture. We present a modified version of the Schatzker classification that attempts to provide the surgeon with a treatment-based classification system (Fig. 22.2).
Treatment options
Non-operative treatment
Any undisplaced fractures (Mayo type I) may be treated non-operatively with the application of a cast or splint. In order to assess stability, however, some authors have recommended evaluation of these fractures under fluoroscopy.1,12 Patients should be treated in neutral rotation and range of motion started after 7–28 days. In general, rehabilitation protocols should avoid elbow flexion greater than 90° to avoid excessive distraction forces. A need to splint in full extension is also a relative contraindication to non-operative treatment. Early reports of this treatment method describe stiffness and a non-functional arc of motion resulting from prolonged immobilization in an extended position.13
Surgical treatment
The goals of olecranon fracture fixation include the anatomical reconstruction of the articular surface and restoration of joint stability, the prevention of joint stiffness and the maximization of power while minimizing morbidity. To accomplish these goals, we recommend a systematic approach (Summary Box 22.3). The type of fracture fixation needed will depend on the fracture type. Options include tension band fixation, intramedullary screw fixation, dorsal plating or hybrid techniques which utilize combinations of the above. There are currently a number of pre-contoured, low-profile plating systems available which facilitate dorsal plating. Supplemental lag screw fixation should be added for oblique fractures and inter-fragmentary screw fixation may be necessary for comminuted fractures. In some instances, when the proximal fragment is too small, too comminuted or osteoporotic, fragment excision may be indicated. We prefer, however, to retain all fragments whenever possible and treat these fractures with indirect fixation through the soft tissue with a FiberTape (Arthrex, Naples, FL, USA) tension band construct.
Summary Box 22.2 Treatment algorithm based on modified Schatzker classification