CHAPTER 25 Fractures of the Olecranon
INTRODUCTION
The subcutaneous location of the olecranon makes it vulnerable to trauma.7 Isolated fractures of the olecranon comprise approximately 10% of fractures about the elbow,26,38 with an estimated incidence of 1.08 per 10,000 person-years.26 Most result from low energy trauma such as a fall from a height of less than 2 meters, a direct blow to the elbow, or from forced hyperextension.1,17,20,26,27,38 A fall on a partially flexed elbow may generate an avulsion fracture of the olecranon from the pull of the triceps.7 Amis et al investigated variable impact mechanisms and the resultant fracture patterns in a cadaveric model.1 A trend was noted in which radial head and coronoid fractures tended to occur with forearm impacts with the elbow in up to 80 degrees of flexion.1 Olecranon fractures occurred with direct blows at 90 degrees of flexion, whereas injuries occurring with the elbow in greater than 110 degrees of flexion tended to result in distal humerus fractures.1
In general, fractures of the olecranon have a favorable prognosis following treatment,7,10,17,20,25,26 with estimates that ninety-six percent of patients have a good to excellent long-term outcome with only rare adverse events.25,26
ANATOMIC CONSIDERATIONS
The olecranon, together with the coronoid process, forms the semilunar or greater sigmoid notch of the ulna.7 This articulates with the trochlea of the humerus and confers stability and facilitates motion in the anterior-posterior plane.7 A transverse “bare area” devoid of cartilage is found at the midpoint between the coronoid and the tip of the olecranon. The unwary surgeon may inadvertently discard structurally significant portions of the olecranon if this is not considered when reconstructing the fractured olecranon.7 The ossification center of the olecranon generally appears by 9 to 10 years of age, and fuses to the proximal ulna by age 14 years.7,14 Persistence of the physis in adulthood may occur, and is usually bilateral and familial. In addition, patella cubiti, an accessory ossicle embedded in the distal triceps, may be present and likewise should not be confused with a fracture.7
EVALUATION
Because the fracture by nature is intra-articular with the exception of some avulsion-type fractures of the olecranon, hemarthrosis is frequently present in conjunction with olecranon fracture.7 Although this sign may be obfuscated by pain due to the injury, inability to actively extend the elbow against gravity may be an important indication of triceps discontinuity.7 Because of the proximity of the ulnar nerve, the first and each subsequent examination should document the status of the ulnar nerve.7 Anteroposterior and true lateral radiographs should be obtained to aid in diagnosis and treatment considerations.7 The true lateral film should be examined to determine the extent and nature of the fracture pattern and to evaluate for the presence of other lesions such as a radial head fracture or dislocation, or distal humerus or coronoid fractures.7
CLASSIFICATION OF OLECRANON FRACTURES
Colton9 classified olecranon fractures according to the degree of displacement and fracture pattern. Colton type I fractures are nondisplaced fractures, in which displacement remains less than 2 mm with elbow flexion to 90 degrees or extension against gravity. The patient can actively extend the elbow against gravity.7,9 Type II, displaced fractures, may be further subtyped into avulsion fractures, oblique and transverse fractures, comminuted fractures, and fracture-dislocations.9
Horne et al20 proposed a classification system and treatment algorithm for olecranon fractures based on review of 100 cases. In this system, type I fractures are either transverse intra-articular fractures of the proximal third of the olecranon or extra-articular fractures involving the point of the olecranon.20 Type II fractures are oblique or transverse intra-articular fractures involving the middle third of the olecranon fossa with type IIA representing those with a single fracture line and type IIB representing those with a second more distal and posteriorly oriented fracture line.20 Type III fractures include those intra-articular fractures of the distal third of the olecranon fossa.20 From review of these 100 cases, Horne et al made treatment recommendations, including favoring the use of plate and screw with tension band fixation in cases of delay of greater than 1 week to decrease the risk of nonunion.20 Extra-articular type I fractures were best treated with excision, whereas intra-articular type I and II fractures should be treated with open reduction and internal fixation with tension band wiring. Recommendations for type IIB fractures involved elevation of the depressed intra-articular fracture and buttressing with bone graft, followed by tension band wiring.20 Type III fractures were best treated with plate and screw fixation to provide optimum rigidity to the construct as tension band wiring was less effective at this location.20
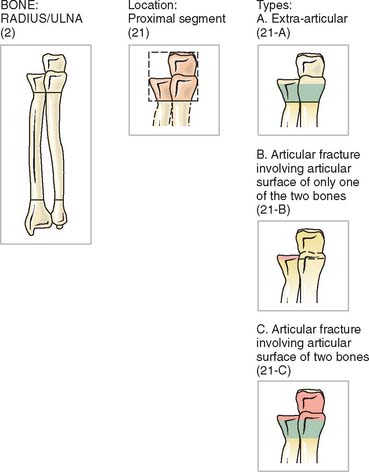
The AO classification system (Fig. 25-1) accounts for both proximal radius and proximal ulna fractures as fracture site 2 for radius/ulna, and 21 for the proximal segment of the radius and ulna. Type A fractures are extra-articular, type B are intra-articular fractures involving the articular surface of either the radius or the ulna, and type C are those involving the articular surface of both bones. Additional subtypes denote comminution, displacement, and location.32 Although the AO classification may be useful for research purposes, it is not commonly used in clinical practice.
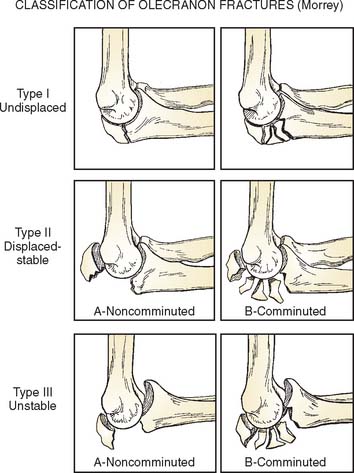
Morrey classified olecranon fractures according to criteria regarding stability, comminution, and displacement.8,31 The Mayo Classification (Fig. 25-2) thus divides olecranon fractures into three types, facilitating classification and providing an algorithm for treatment.8,31
Type I, undisplaced fractures as defined by the Colton criteria earlier, may be subdivided into type IA, noncomminuted fractures, and type IB, comminuted fractures.31 These fractures represent approximately 5% of olecranon fractures. Because these fractures are by definition nondisplaced, the practical significance of the degree of comminution is not significant and types IA and IB may essentially be regarded and treated as the same lesion.31
Mayo type II fractures are the most common type, representing about 85% of olecranon fractures.27,31,38 These fractures, which are stable fractures with greater than 3 mm of displacement, may be noncomminuted (type IIA) or comminuted (type IIB).31 Because the collateral ligaments are intact, the forearm is stable relative to the humerus.31
Mayo Type III fractures are unstable, displaced fractures and represent a fracture-dislocation. Like types I and II, type III fractures may be subclassified into noncomminuted (IIIA) or comminuted (IIIB) types.8,31
COMPLEX OLECRANON FRACTURE-DISLOCATIONS
Olecranon fractures associated with subluxation of the radial head and/or the coronoid process are typically multifragmentary, complex injuries.12,35,37 Anterior fracture dislocations are often referred to transolecranon fracture-dislocations, because the mechanism of injury appears to involve anterior displacement of the forearm, resulting in the trochlea being driven through the olecranon process.12,35,37 The radial head is displaced anteriorly, and this injury is differentiated from the Bado type I Monteggia fracture by the presence of ulnohumeral joint destabilization with preservation of the radioulnar relationship.35,37 Posterior fracture dislocations of the olecranon are more similar to type II Monteggia fractures, with posterior dislocation of the radial head, an apex posterior fracture of the ulna, and similar implications for the stability and function of both the ulnohumeral joint as well as the forearm.12,35 These fractures may be considered a variant of the posterior Monteggia lesion.12 Both posterior and anterior variants are commonly associated with fractures of the coronoid, which are usually basal fractures involving 50% to 100% of the height of the coronoid.35 In anterior olecranon fracture-dislocations, reduction of the olecranon and coronoid fracture fragments results in restoration of stability, with little implication for forearm dysfunction. Posterior olecranon fracture-dislocations, in contrast, have important implications, with elbow instability and forearm dysfunction being common despite fracture reduction.35
TREATMENT
The Mayo Classification provides a basis for a rational treatment algorithm by fracture type and subtype, and conveys prognostic value.31,38
Nondisplaced fractures (Mayo type I) may be treated symptomatically and nonoperatively with 7 to 10 days of immobilization in midflexion and neutral rotation, followed by initiation of an active range of motion program.6,8,17,31 Restrictions on active resisted elbow extension and weight bearing should be maintained for 6 to 8 weeks, with gradual increases in these activities as tolerated.6 Close follow-up with radiographs at 1, 2, and 4 weeks is recommended to assess for displacement and possible need for further intervention.7 Rarely, in select patients, type I fractures may benefit from open reduction and internal fixation to allow immediate motion and stability.8,31 Some type I fractures may be treated with immobilization in a long arm cast at 90 degrees of flexion for 3 to 4 weeks.7 Thereafter, protected range of motion with avoidance of flexion greater than 90 degrees until radiographic evidence of bony healing occurs, usually at 6 to 8 weeks, is recommended.7 Range-of-motion exercises may be commenced at an earlier time point in select patients, such as the elderly, in whom stiffness occurs more frequently.7
Displaced fractures (Mayo type II and III) usually require surgical intervention.6,8,17 Goals of surgical management include restoring the articular congruity and stability of the elbow, maintaining extension power, and providing stable anatomic fixation such that early range of motion is possible, thereby lessening the risk of stiffness.7,16,17,21 Options include excision or open reduction and internal fixation with a variety of devices including tension band wiring, intramedullary screw placement, plate and screw constructs, or bioabsorbable pins.4,6,15,17,27,31,38
SURGICAL MANAGEMENT OPTIONS
Excision
Excision of fracture fragments with advancement and reinsertion of the triceps tendon may be indicated in cases of nonunion, patients who are elderly or who have poor soft tissue viability, avulsion-type extra-articular fractures, and in cases with severe comminution as in Mayo type IIB fractures (Fig. 25-3).7,10,11,13,15,31 Disadvantages of excision include subsequent risks of triceps weakness, instability, stiffness, and a theoretical risk for increased arthrosis due to altered contact pressures.2,7,11,24,29 However, excision obviates risk of nonunion, hardware failure, or prominence, and others suggest a decreased risk of post-traumatic arthritis, because the possibility of incongruity of the articular surface reduction is eliminated with excision of the fragment rather than reduction and fixation.11,17,15
McKeever and Buck determined that one may excise up to 80% of the olecranon without sacrificing stability if the coronoid and anterior soft tissues are intact.7,15,28 If anterior damage is present, instability is a sequelae if too much proximal ulna is excised.7 In addition, An et al2 noted increasing instability of the elbow with olecranon excision, and data from the Mayo laboratory suggest that resection should be limited to 30% of the olecranon. Kamineni et al24 investigated the impact of olecranon resection on stability in relation to posteromedial stresses in a cadaveric model. Resection of osteophytes and proximal ulna was performed to simulate treatment of posteromedial osteophytes, such as in throwing athletes. The investigators noted a clinically significant level of instability with valgus stresses following resection of as little as 6 mm of posteromedial olecranon.24 The authors speculated that this instability may not be clinically relevant in low-demand, elderly patients, but it may be problematic in higher demand athletes or active patients or laborers.24 The increased instability may place increased stress upon the medial collateral ligament, predisposing to possible failure.24 However, excision is usually used in older, low demand patients who may not place such demands on their elbows.
Many authorities recommend reattachment of the triceps at the level of the articular surface.7,11 However, one recent study suggests that attachment more posteriorly results in improved extension strength.11 Didonna et al11 studied variable positions for triceps reattachment following partial olecranon (50%) excision for simulated olecranon fracture in a cadaveric model. Loads were applied along the triceps mechanism at 45 degrees, 90 degrees, and 135 degrees, and the resultant forces were recorded. A significant decrease in extension strength with anterior placement of the triceps relative to normal and relative to posterior placement was noted, with the differences greatest with increasing extension. In contrast, posterior reattachment was noted to result in decreased extensor strength only at 90 degrees. Therefore, the authors recommended more posterior reattachment sites to minimize loss of extension strength.11
Although some authors report less post-traumatic arthritis with excision due to avoiding an incongruent joint, some speculate that excision may lead to increased risk of post-traumatic arthrosis.29 In a cadaveric model with 50% olecranon osteotomy to simulate an olecranon fracture, peak forces across the ulnohumeral joint were measured following either excision of the proximal fragment or open reduction and internal fixation with tension band wiring.29 Elbows fixed with tension band wiring had no significant difference in peak ulnohumeral pressures when compared with the intact elbow joint.28 In contrast, elbows with excision of the proximal fragment were noted to have significant increases in joint forces over the medial and lateral articular surfaces.29 The authors theorized that open reduction and internal fixation with tension band wiring restores the normal biomechanics of the elbow, whereas excision results in abnormal joint forces, which may predispose to arthrosis.29 As such, Moed et al29 favored open reduction and internal fixation in cases in which a large proximal fragment is present.
Nevertheless, satisfactory clinical outcomes (see Fig. 25-3A to C) have been described for treatment of olecranon fracture by excision when used in appropriate patient populations.10,13,15,17 Gartsman17 noted equivalent range of motion, functional status, extensor strength, pain, stability, and incidence of degenerative changes in cases of olecranon fracture treated by open reduction and internal fixation or primary excision.17 In addition, local complications (23% versus 4%) and requirements for additional procedures (an additional 23%), such as hardware removal, were more common in the patients treated with open reduction and internal fixation.17 Such studies demonstrate that excision is a good option for treatment of the appropriate fracture in the appropriately selected patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree